FINDINGS from a study with Aboriginal peoples from Kamilaroi, Wiradjuri and Dunghutti lands suggest some people are cautious about the COVID-19 vaccines.
What people think and feel about the vaccines, including vaccine safety and perceived benefits and risks, along with social processes, such as distrust in government, may contribute to vaccine hesitancy. Findings from this study confirm recommendations from the Collaboration on Social Science in Immunisation, which suggest a need to prioritise key groups for communication, including Aboriginal and Torres Strait Islander peoples who may need an opportunity to yarn about COVID-19 vaccines and ask questions.
Cultural safety and shared decision making
Shared decision-making is now a core component of quality and safety standards in health care in many countries (here and here). It is a process where consumers and health care professionals make informed and preference-based decisions about health together. Decision aids are tools that use evidence-based information about options, benefits and risks to support the shared decision-making process (here, here and here).
Decision aids are available for COVID-19 vaccines, including the AstraZeneca Vaccine Decision Aid and the Pfizer Vaccine Decision Aid. An evaluation of the interactive web tool found moderate increases in intention to vaccinate after use among individuals with chronic conditions who initially intended to decline. There are very few culturally adapted decision aids and tools more generally; none have been adapted with Aboriginal and Torres Strait Islander peoples to support decisions about vaccines in the context of COVID-19.
Shared decision-making is also a priority reform area within the National Agreement on Closing the Gap, which calls for partnership in “policy” and “place” between Aboriginal and Torres Strait Islander peoples and government. There are existing health inequalities for Aboriginal and Torres Strait Islander peoples in Australia, but culturally safe health care may contribute towards an improvement in this situation. Cultural safety includes good communication, respectful treatment, empowerment in decision making and the inclusion of family members. This aligns well with the principles of shared decision-making, but how it might be adapted into practice remains untested.
To support equity of access in the COVID-19 vaccine roll-out there is a need for Aboriginal and Torres Strait Islander peoples to have a culturally safe approach to making decisions about vaccines. Aboriginal and Torres Strait Islander peoples need an opportunity to yarn about the vaccines and weigh up the benefit and risk. Vaccine decisions are likely be affected by community and family obligations.
To adapt shared decision-making resources for use in the context of COVID-19 and decisions about vaccines, yarning sessions were facilitated with Aboriginal and Torres Strait Islander peoples (herein respectfully referred to as Aboriginal) in New South Wales, including community members and health workers. The term “mob” has been used throughout to identify who we are and where we are from — our connection to our shared identity as Aboriginal peoples.
Approach to adapting shared decision-making resources with mob, for mob
The goal was to rapidly adapt and disseminate culturally appropriate shared decision-making resources for Aboriginal peoples to use in the context of COVID-19 and decision making about vaccines. The group adapted an existing three-talk model for shared decision-making and the Ask, Share, Know question prompt.
A series of five semi-structured yarning sessions brought Aboriginal health workers and community together between 20 August 2021 and 6 September 2021 (Box 1).
| Yarn 1: Knowledge sharing and deep listening |
Yarn 2: Deconstruct and reconstruct |
Yarn 3: Reconstruct, deconstruct and story sharing |
Yarn 4: Deconstruct and reconstruct |
Yarn 5: Finalise together |
| Two-way knowledge sharing: what is shared decision making and different tools for yarning about health decisions?
Sharing stories and deep listening about COVID-19 vaccine concerns from community |
What do you think and feel about the resources?
What do you like or not like about the resources?
What would you change and why? |
What do you like or not like about the new model?
What would you change and why?
How would we describe the different parts of the model to others? |
What do you like or not like about the question prompt?
What change would you make and why?
How would we describe the question prompt to others? |
Have we created resources that could be useful for making decisions about health, including COVID-19 vaccines?
How would we describe the resources to others? |
| 20 August 2021, 10 am – 12 pm | 25 August 2021, 3 pm – 4.30 pm | 27 August 2021, 10.30 am – 12.30 pm | 31 August 2021, 3 pm – 4.30 pm | 6 September 2021 11 am – 12 pm |
| 165 Aboriginal community members from across NSW | 16 Aboriginal community members from across NSW | 12 Aboriginal community members from across NSW | 12 Aboriginal community members from across NSW | 11 Aboriginal community members from NSW |
Box 1. Semi-structured yarning sessions
The invitation to participate in the yarning sessions, including a detailed information sheet, was sent through a range of existing networks on 18 August 2021. The first yarning session was open to the broader community and attended by a large group of Aboriginal peoples. A small working group was then formed to develop the new resources with community members living and working on Eora, Wilyakali, Gandangara, Wiradjuri, Bundjalung, Darug and Yuin lands.
The yarning sessions were informed by methods used to culturally adapt a generic shared decision-making tool with Aboriginal women in Canada, Dadirii-Ganma and the Aboriginal Eight Ways of Learning pedagogy framework including storytelling, images and symbols, non-linear, community links and deconstruct and reconstruct components (here and here). Rapid prototyping and out-of-session feedback was used to test and validate ideas throughout the process, leading to the adaption of the resources with Aboriginal health workers and community members, an Aboriginal artist and graphic designer, and with Aboriginal leadership at all levels. The Agency for Clinical Innovation (ACI) supported the process and the group received advice from academic leaders experienced in shared decision-making along the way.
The first yarn included story sharing from the community and deep listening about COVID-19 vaccine concerns. Subsequent yarns were framed around the three-talk model for shared decision-making and the Ask, Share, Know question prompt.
The outcome from the yarning sessions is a culturally appropriate model of shared decision-making called “Finding your way” (Figure 1), a collective narrative to describe the model, a question prompt for COVID-19 vaccines (Figure 2), short videos, and a web-based interactive tool (visit https://aci.health.nsw.gov.au/shared-decision-making to access all resources).
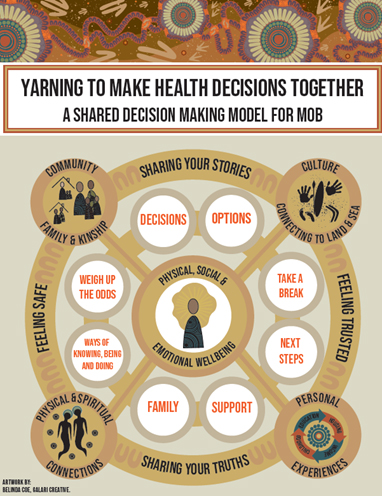
Figure 1. “Finding your way”: a shared decision making model for mob
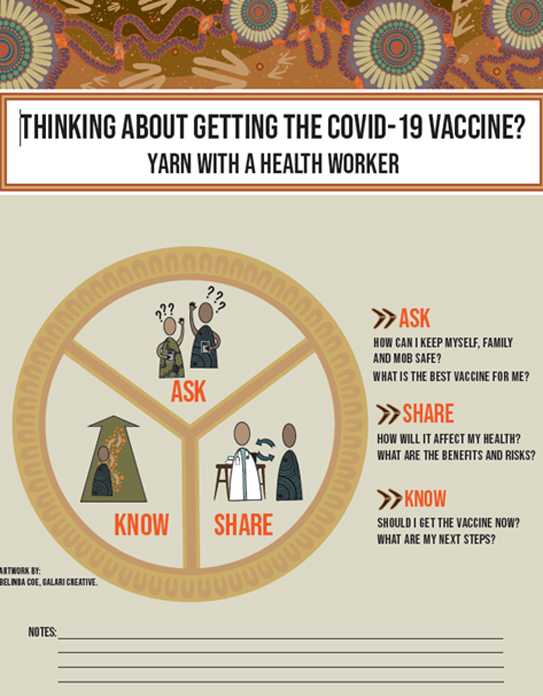
Figure 2. Cultural adaption of the “Ask, Share, Know” question prompt
Shared decision-making is about Aboriginal peoples connecting with health care professionals in a holistic and meaningful way – where mob feel safe and trusted to make informed decisions based on their values and beliefs. The process helps mob and health care professionals to make health decisions together.
“Finding your way” tells the story of an individual’s journey. We all start at the beginning, but we choose different paths as we walk through our country.
The circular design of the model, and everything in it, represents the holistic concept of Aboriginal health: physical, social, emotional, cultural and spiritual wellbeing for both the individual and the community. The circle represents a continuous cycle a person moves through when interacting with the health system and making decisions about their health in a non-linear direction, finding their way in a forward, backward or sideways direction.
The centre image illustrates the individual, and the glowing aura radiates positive thinking and energy for the overall decision-making process. This image interconnects with many circles represented holistically to evoke conversations and guide the shared decision-making process. The tracks from the centre circle are interconnected and lead to four larger circles. These circles represent the scaffolding needed for Aboriginal peoples to make health decisions.
- Community, family and kinship refer to the interconnectedness of Aboriginal peoples and the importance of community and family connections in all aspects of Aboriginal life. This circle intentionally connects to “feeling safe” and “sharing your stories” to illustrate the importance of story sharing in terms of yarning as a narrative that brings cultural meaning as a process for communication through information sharing and making health decisions with family. It is about fostering reciprocal relationships to allow individuals to feel safe to share their stories.
- Culture and connecting to land and sea refers to the importance of the cultural determinants of health and the centrality of land and water in culture. This circle intentionally connects to “sharing your stories” and “feeling trusted” to illustrate the importance of local knowledge, language, culture and connection to country. It is about finding common ground through sharing stories and yarning about what “actually matters” to the individual. When culture is embraced, it creates a sense of trust for the individual.
- Personal experiences centre on the social determinants of health and influencing factors such as housing, education, income, childhood and access to health care. Aboriginal peoples have faced many hardships and continue to be affected. This circle intentionally connects to “feeling trusted” and “sharing your truths” to illustrate the impacts of colonisation, racism and intergenerational trauma when making health decisions. It is about being mindful of the health inequalities.
- Physical and spiritual connections centres on the notion of physical, mental, and spiritual wellbeing. When the spirit is strong, you can make good health decisions. This circle intentionally connects to “feeling safe” and “sharing your truths” to illustrate our connection to all things, our deepest thoughts, attitudes, judgements, values and beliefs. It is about our ways of knowing, being and doing that are deeply rooted in our ancestral knowledge systems that inform shared decision making.
The model also features eight inner circles that represent the core elements of shared decision-making from a cultural perspective. Each circle is a broker point for a yarn, with prompts to guide the shared decision making process (Table 2).
 |
 |
| Yarn to bring it all together and decide to act now if ready (eg, have the vaccine) or wait. | Yarn about health needs and options available including the benefits and risks of the vaccines. Ask questions, share knowledge and feelings about the vaccines. |
 |
 |
| Yarn about taking a break (if needed) and making the decision later. Come back and yarn on another day | Yarn about the next steps, including how and where to get vaccinated and what might get in the way. Follow up later |

|
 |
| Yarn about what is happening today, including social, emotional and wellbeing needs and supports | Yarn about family and mob. If needed, bring others into the yarn for support |
 |
 |
| Yarn about ways of knowing, being and doing to inform health decisions based on a person’s values and beliefs | Yarn about the vaccines’ possible benefits and risks. Compare options and weigh up the odds individually and for family and mob |
“Finding your way” aligns with the core elements of shared decision-making, including describing options, benefits and risks, weighing up the options, and tailoring information. By adapting the model with Aboriginal peoples, “Finding your way” reflects a holistic approach to health and wellbeing, includes family and other cultural factors, and highlights the non-linear approach Aboriginal peoples often take to decision making about health.
The model and resources have long term potential to be widely adapted on a localised scale, using local Aboriginal languages and cultural references for each different Aboriginal communities across NSW and Australia.
Acknowledgements: We acknowledge the contributions of everyone who participated in these meaningful conversations and for adapting the shared decision making resources. As the host of these conversations, we acknowledge that NSW Health was privy to the ancient and traditional process of yarning and the respect and sharing of knowledge that this involves. We acknowledge the lands on which these conversations took place, the lands of an ancient and continuing culture, and we respect the elders’ past, present and emerging of these Aboriginal lands. These lands always were and always will be Aboriginal land.
We thank Jean-Frederic Levesque, Kim Sutherland and Tracey Tay from the Agency for Clinical Innovation (ACI) for their ongoing support. The ACI also commissioned the artwork from Belinda Coe, Galari Creative. We thank Belinda very much for her deadly artwork. The artwork is reproduced with permission from the ACI.
Tara Dimopoulos-Bick is the Evidence Generation and Dissemination Manager at the Agency for Clinical Innovation (ACI). Her work focuses on bringing the knowledge, expertise and wisdom from individuals and groups to the forefront as part of the ACI’s evidence model.
David Follent is the Senior Project Officer in Chronic Care for Aboriginal People at the Agency of Clinical Innovation and the current chairperson of the National Association of Aboriginal and Torres Strait Islander Health Workers and Practitioners. He is a proud Bundjalung man living on Gadigal lands.
Catherine Kostovski is a Yuin woman and the Project Officer for the Agency for Clinical Innovation. Catherine is passionate about improving health services for First Nation’s peoples.
Val Middleton works within the Primary Healthcare Institute, Integrated Care and Aboriginal Health, Agency for Clinical Innovation (ACI), to bring a primary health perspective to ACI’s key initiatives.
Cory Paulson is a Worimi, Minjinbul man working with Far West Local Health District in community Mental Health Drug and Alcohol service.
Stewart Sutherland (PhD) raised in Wellington NSW the heart of Wiradjuri country. For nearly two decades he has worked in Indigenous health, in more recent years focusing on identity, mental health, culture. His PHD, at the Australian National University Canberra, the focus of which was the interplay between reconciliation (apology) and the Social Emotional Wellbeing of people forcibly removed from their families.
Melissa Cawley, Wiradjuri woman and Program Support Officer for the South East Sydney Local Health District’s Aboriginal Health Unit. She is committed to driving change and enhancing equity for Aboriginal people.
Marsha Files is an Aboriginal woman from Barkindji Country and has worked in the health sector for the past 18 years, Marsha’ passion is for her communities to become empowered around their health.
Larissa Karpish is a Ngunnawal woman and registered nurse working as a part of the Aboriginal Population Health Traineeship Initiative with the Sydney Children’s Hospital Network.
Sue Follent is a Bundjalung woman living in Bogangar, Far North Coast NSW (Bundjalung Country). Sue is a retired Aboriginal Health Manager and Worker, and active Aboriginal community member on the Tweed Coast.
Regina Osten is the Stream Manager for Integrated Care and Aboriginal Health at the Agency for Clinical Innovation, and she leads the Chronic Care for Aboriginal People Team, and the Aboriginal Chronic Conditions and Rural Health Networks, Virtual Care, and the Primary Healthcare Institute.
Lyndal Trevena is a Professor Emerita at the University of Sydney and is an active general practitioner. She has received international recognition for her research in shared decision making and co-led the NHMRC Centre for Research Excellence ‘Ask, Share. Know: Rapid Evidence for General Practice Decisions.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert
Excellent, outstanding, urgently needed. ACI please also make all the resources readily shareable – not only on your website – but via social media links – especially which reach out to diverse mob across Australia. Very important and timely. Great processes. Congratulations to all who led this & the communities who participated. @Tara Dimopoulos-Bick @David Follent @Catherine Kostovski @Val Middleton @Stewart Sutherland @Melissa Cawley @Cory Paulson @Melissa Cawley @Marsha Files @Larissa Karpish @Sue Follent @Regina Osten @Lyndal Trevena
It’s great to see this kind of model development with our mobs.