GPs and other vaccinators must help Australians weigh up the rarity of the blood clotting disorder tentatively linked to the AstraZeneca COVID-19 vaccine, against the potentially serious consequences for the unlucky few, and the societal need to protect the community.
On 8 April the Australian Technical Advisory Group on Immunisation (ATAGI) recommended suspension of the use of the AstraZeneca (AZ) COVID-19 vaccine in people under 50 years, following reports of cases of what is now called vaccine-induced thrombocytopenia and thrombosis (VITT).
While it is an option to wait for a Pfizer vaccine, even for those aged over 50 years, Professor Kristine Macartney, Director of the National Centre for Immunisation Research and Surveillance, and a member of ATAGI, told InSight+ that the single most important thing to remember was that COVID-19 “is not leaving the world and we all remain at risk”.
“It’s going to be with us for our lifetimes,” she said.
“We want vaccines to make this virus one that we can live with more comfortably – not having as much severe disease, protecting the vulnerable and being able to reduce overall transmission of the virus in the community.”
While Australia has paused AstraZeneca vaccines for those aged under 50 years, in Germany, the two biggest cities, Berlin and Munich have suspended its use in those under 60 years, Belgium has suspended it in for those under 56 years, and Denmark has stopped giving it altogether. The UK is also offering an alternative to those aged under 30 years.
Although a definitive link between the vaccine and blood clots has not been established, two case series published last week in the New England Journal of Medicine have added weight to the association between the AstraZeneca vaccine and the occurrence of VITT.
The first study involved five cases from Norway who presented with venous thrombosis and thrombocytopenia 7–10 days after receiving the first dose of the ChAdOx1 nCoV-19 (AstraZeneca) vaccine.
“Within 10 days after receiving a first immunization with ChAdOx1 nCoV-19, five health care workers 32 to 54 years of age presented with thrombosis in unusual sites and severe thrombocytopenia. Four of the patients had severe cerebral venous thrombosis with intracranial hemorrhage, and the outcome was fatal in three,” the authors wrote.
“A common denominator in all five patients was a high level of antibodies to PF4–polyanion complexes.
“Collectively, these results suggest that the serum in these patients contained immune complexes with a mixture of antibody specificities similar to those described in the serum of patients with autoimmune heparin-induced thrombocytopenia.
“Our findings indicate a shared pathophysiological basis of the condition in these five patients and should raise awareness that a syndrome similar to autoimmune heparin-induced thrombocytopenia may occur in some persons after vaccination with ChAdOx1 nCoV-19.
“By providing a link between thrombosis and the immune system, these results strengthen the view that vaccination may have triggered the syndrome.”
The second case series involved 11 patients from Germany and Austria in whom thrombosis or thrombocytopaenia had developed after vaccination with ChAdOx1 nCov-19.
“Of the 11 original patients, 9 were women, with a median age of 36 years (range, 22 to 49),” the authors wrote.
“Beginning 5 to 16 days after vaccination, the patients presented with one or more thrombotic events, with the exception of 1 patient, who presented with fatal intracranial hemorrhage. Of the patients with one or more thrombotic events, 9 had cerebral venous thrombosis, 3 had splanchnic-vein thrombosis, 3 had pulmonary embolism, and 4 had other thromboses; of these patients, 6 died. Five patients had disseminated intravascular coagulation. None of the patients had received heparin before symptom onset.”
They concluded that:
“Vaccination with ChAdOx1 nCov-19 can result in the rare development of immune thrombotic thrombocytopenia mediated by platelet-activating antibodies against PF4, which clinically mimics autoimmune heparin-induced thrombocytopenia.”
Professor Macartney, while acknowledging the NEJM reports, told InSight+ that a definitive causal link between the AZ vaccine and the rare condition, and the mechanism behind it, had yet to be established.
“This condition has been reported in adults of with a range of ages — the oldest person to have been reported with this condition is in a case series from the UK where they have indicated that someone who was aged 79,” she said.
“We are saying it’s rare across the age spectrum, but it appears to be slightly less rare in people who are younger. Right now, it’s important to remember that at this stage, across the entire world, there’s only been a few hundred cases in what have been hundreds of millions of AstraZeneca doses given out.
“At present, we don’t know of any risk factors that predict the condition because it is new. Based on what we know, it appears to be idiosyncratic, meaning that we cannot predict who will develop it.
“We all hope the answer to that comes quickly because it they may allow us to understand some risk factors which predict the condition.”
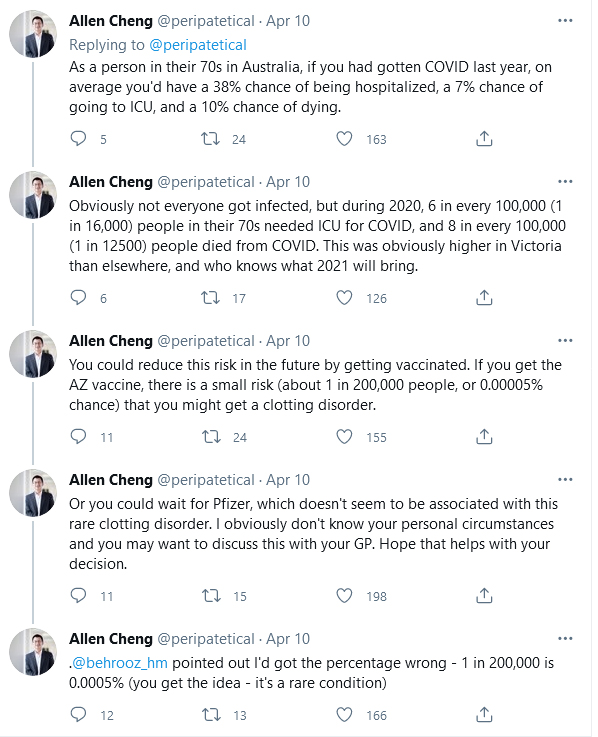
Professor Allen Cheng, Professor of Epidemiology and Preventive Medicine at Alfred Hospital and Monash University, is currently Deputy Chief Medical Officer of Victoria. He took to Twitter last week (@peripatetical) to put in perspective the risks of developing VIPIT as a result of vaccination with the AztraZeneca vaccine.
“As a person in their 70s in Australia, if you had gotten COVID last year, on average you’d have a 38% chance of being hospitalised, a 7% chance of going to ICU, and a 10% chance of dying,” Professor Cheng tweeted.
“Obviously not everyone got infected, but during 2020, 6 in every 100 000 (1 in 16 000) people in their 70s needed ICU for COVID, and 8 in every 100 000 (1 in 12 500) people died from COVID. This was obviously higher in Victoria than elsewhere, and who knows what 2021 will bring.
“You could reduce this risk in the future by getting vaccinated. If you get the AZ vaccine, there is a small risk (about 1 in 200 000 people, or 0.0005% chance) that you might get a clotting disorder.
“Or you could wait for Pfizer, which doesn’t seem to be associated with this rare clotting disorder.”
Professor Macartney emphasised the importance of raising awareness of the symptoms of VIPIT.
“We have an obligation to inform people that if they are developing significant new symptoms in this time period after vaccination around four to 20 days, that it is very important that they are medically reviewed,” she said.
“This is not a typical deep vein thrombosis (DVT).
“This condition is serious and is characterised by clots forming in unusual places — either in the draining veins of the brain or in the splanchnic, which is the abdominal vessels.
“It can present as either a severe new headache, or neurologic symptoms, or presents as abdominal pain.”
Professor Macartney told InSight+ that work was continuing in many laboratories around the world to find definitive answers about VIPIT and who was most at risk and why.
“We have a long way to go with this virus, and we will get there, but it’s not going to be quick. It’s a tricky position to be in.”

 more_vert
more_vert
I am in agreement with your response no.18 from Catherine Sharp about the need to pull back the syringe to ensure needle not located in blood vessel. I am also a nurse. It seems crazy that the injection procedure is not being modified in this regard.
FROM THE EDITOR: Our advice is always to talk with your GP.
At 76 I am very worried at I had thrombosis at the age of 23, had an operation to remove the clots, and warned to be careful. So what do I do now?
Simon, I think Professor Paul Monagle is the expert opinion you should seek. He is an internationally regarded haematologist and actively involved in the Astra Zeneca debate.
I have had an immune reaction to my platelets following injections of G-CSF for heart failure at St Vincents Hospital -Garvan Institute as part of a clinical trial. My platelets dropped from 90,000 down to 5,000. This is a very rare complication of G-CSF usage.
My question is where do I go to get an expert opinion founded on facts rather than opinions as to the risks and whether I should avoid the Astra Zeneca vaccine?
Perhaps use of Astra Zenica vaccine in Australia is more relevantly compared to Takata airbag rather than motor vehicle accidents themselves . A potentially lethal complication of a preventative measure.
Deaths from Takata airbags:
“There have been more than 330 injuries and 30 deaths reported worldwide, with one death and three injuries in Australia, including one serious injury.”
https://www.accc.gov.au
I’m a 70 year old female of bi-racial (Australian Aboriginal & European) heritage, with several major health issues. I really do not want to be given the ‘AZ’ vaccination and I am prepared to wait for something safer, however long that may take.
I have been following every report about this vaccine and I am definitely not an ‘anti vaxxer’, so I feel that after much discussion with family, my decision is an informed one.
What a polite discussion and what a difficult problem. It is instructive to have a look at US medical forums now that J&J vaccine may be associated with the same clotting issues as Astra Zeneca. The consensus building seems to be “why would I give an Adenovirus vaccine when RNA vaccines seem so much safer ?” And, that Adenovirus platforms vaccines should be reserved for the developing world where Coronavirus is rife, cold chains are harder and second best has to good enough.
We have done so well in Australia and it seems such a shame that we are now in a difficult position regarding vaccination . Perhaps one of our few mistakes as a nation has been not to source a broader range of different vaccines at a time that efficacy and rare side effects were unknown for all of the candidates. Maybe, we have put too many eggs in the Astra Zeneca basket. But, we are where we are, and now us GPs have to help our patients make difficult decisions and the nuance we use is all important . We can compare vaccine risk to MVA risk or lightening strike risk or whatever but right now when there is zero community spread I would be mortified if one of my patients where to die from a vaccine for an infection that is non existent outside quarantine in this country. I have been a yellow fever vaccinator for years, YF vaccine has a risk of mortality, especially in the elderly, and like most vaccinators I have tried very hard not to give it to patients where the risk of vaccination seems to outweigh the risk of getting the disease and to ask worried patients if they really need to travel to a yellow fever endemic country. At this point of time in this country we are asking people to choose between a very low risk from a vaccine and a next to zero risk of disease. All fine, if you are one of the 199 999, not so fine if you are the 1 .
Of course we all believe that sooner or later Coronavirus will be back in the Australian community ( sooner rather than later if Qantas , the Queensland tourist industry and the universities get their way ) , and then it would be good if most of the country was immune, but at this pint of time I am seeing a lot of personal vaccine hesitancy including amongst doctor friends and vaccine enthusiasts and I completely understand that. My bookings for the few Astra Zeneca vaccines I have are well down this week and that is before I have discussed the issue with patients. A few more Aussie deaths associated rightly or wrongly with the AZ vaccine and the whole thing may become a flop.
Perhaps the conundrum of getting our country protected against Covid can only be solved by the government throwing a lot of money at CSL and Pfizer and urgently building our own RNA vaccine manufacturing capability , accepting that it will take six months more to get the population vaccinated and I suspect in the end that’s what will happen.
Or we could have vaccine passports in which case someone may have the unenviable task of telling the Chinese that their vaccine is not up to scratch.
Difficult times and above my paygrade.
I have had the Astra Zeneca vaccine personally.
“Based on the maths your risk from the vaccine is orders of magnitude less than the virus. “. The risk from the virus in Australia is virtually nil. The from AZ vaccine, while remote is still currently higher than the risk from Covid in Australia (although obviously not in other parts of the world). The urgency to vaccinate in Australia is driven by economic / business imperatives to open the borders ASAP when Covid cases will increase. Personally the closed borders have not impacted me much so the AZ vaccine is a hard sell right now. Comparing this with risk of driving and so on is comparing apples with oranges. I can take the bus.
Those contemplating the risk benefits of a vaccine should be aware of the uncertainties in the data used to calculate the estimates of the incidence of VITT.
The number of vaccinations performed is well documented however the number of complications depends on recognising/diagnosing the complication and then reporting the complication to the authorities. Around the time of the initial description of VITT very few cases were described and the reported incidence was only about 1 or 2 in a million. As the health profession became more aware of the syndrome more cases were diagnosed and reported and the EMA and UK medical authorities reported increased incidences of between about 1 in a 100,000 and 1 in 200,000. Both authorities rely on voluntary reporting and may underestimate the incidence.
Smaller countries with health systems that enable close follow up and more complete reporting of complications after vaccination may provide a better estimate.
Finland reported 2 cases of VITT after 140,000 vaccinations, an incidence of 1 in 70,000, and paused the use of the AstraZeneca vaccine on 22 March.
https://thl.fi/en/web/thlfi-en/-/thl-temporarily-suspends-the-use-of-the-astrazeneca-covid-19-vaccine
Norway was one of the first countries to recognize an increase in incidence in atypical clotting in patients receiving the AstraZeneca vaccine. The issue was widely discussed in their scientific and popular media. https://sciencenorway.no/covid19-vaccines/this-is-why-norway-is-still-saying-no-to-the-astrazeneca-vaccine/1832874
Norway began AstraZeneca vaccination on 7 February and paused vaccination 11 March after reports of atypical clotting. Follow up of the 120,000 people vaccinated eventually identified 6 cases of VITT (5 of these cases were reported in the NEJM publication), 4 of these cases have died.
https://sciencenorway.no/covid19-vaccines/norwegian-health-authorities-will-keep-investigating-possible-side-effects-from-the-astrazeneca-vaccine/1835781
This is an incidence of VITT of 1 in 20,000 vaccinations and a mortality of 1 in 30,000.
If everyone in Australia was vaccinated with AstraZeneca vaccine an incidence of 1 in 200,000 implies there would be 86 cases of VITT, an incidence of 1 in 20,000 implies 858 cases of VITT. The mortality of VITT is about 40% and there is a substantial but seldom mentioned morbidity. However the recent reports in NEJM investigating the pathogenesis of VITT provide hope that early diagnosis and specific treatment of VITT will reduce this mortality and morbidity.
There are three independent descriptions of 39 people with the newly described syndrome of VITT. The syndrome is similar to HIT but our understanding of the pathogenesis is incomplete. Treatment with IV immunoglobulins, steroids, and non-heparin anticoagulants may help, the editorial accompanying the third report states “We expect that the high mortality rate associated with VITT will decrease with earlier recognition and improved intervention.”
https://www.nejm.org/doi/full/10.1056/NEJMe2106315?query=recirc_curatedRelated_article
Now our most urgent priority is to make sure any further cases of VITT in Australia are detected promptly and then managed appropriately. Patients should be warned that the incidence of VITT is uncertain and may not be as rare as initially thought. Patients, 3-20 days post vaccination, with symptoms suggesting VITT, should be seen urgently and admitted to hospital for further investigation and management if there are any concerns.
Patients and probably many medical practitioners are currently unaware of the high mortality and long-term morbidity of VITT and the importance of prompt diagnosis and treatment.
Why haven’t the randomised trials identified VITT?
The numbers in the trials are too small to reliably identify rare complications.
However, recently, 6 cases of VITT after J&J vaccination were found. (J&J is a type of vaccine similar to AstraZeneca) One case report pointed out that a young man in the J&J randomised trial developed CVST after vaccination. https://www.nejm.org/doi/10.1056/NEJMc2105869
The trial was paused, the case investigated, but, at that time, considered to be not related to vaccination. After a more recent review of this case the company has confirmed that the platelet factor 4 antibodies were positive and the platelets were low, typical of VITT. https://www.nejm.org/doi/full/10.1056/NEJMc2106075?query=featured_coronavirus
Thus, with the advantage of hindsight, the incidence of VITT in the J&J randomised trial was 1 in 50,000.
The latest series of cases of VITT after the AstraZeneca vaccine, published in NEJM, reports that, in a single week, 23 cases of VITT were referred to a haematologist in a London hospital. https://www.nejm.org/doi/full/10.1056/NEJMoa2105385
The incidence of VITT appears to be somewhat higher than the chances of winning a lottery.
I concur with Catherine Sharp
A risk from a necessary activity is conceptually different to a risk from a risk.
Annual death risk on the roads in NSW is 400/8M, i.e. 1/20,000. That’s overall, irrespective of pedestrian/driver/rider status; obviously higher if you speed while drunk etc.
Road death risk in an arbitrary period of 3 weeks, approx. 1/300,000.
Same order of magnitude as VIPIT in that timeframe, post vaccination.
Those who fear vaccination need to consider a hermit existence away from the road risk, far more than the vaccine risk.
To date there have been roughly 100,00 deaths from COVID in the USA in people under 65.
That’s not counting people with long COVID and other permanent sequelae.
“risk of serious harm … rare”
Really ?
If anything, the thrombosis risk with this vaccine (and for that matter any intervention) highlights the substantial risk of dismissing the ability of our own immune systems to do the very same job. And that of course is determined by maintaining a healthy lifestyle through eating sensibly and exercising regularly. Something this country (and a first world country at that!) fails miserably at.
As a cancer surgeon with a degree in immunology I speak with some authority
The risk of serious harm in the short term from the various covid vaccines incl AZ seems rare. The long term risks are unknown. The risk of serious harm from covid19 in healthy people under 60 seems equally rare. How can we ethically justify mass vaccination of the minimally at risk part of the population?
I’m a 74yo recently retired GP, in good health. I had idiopathic thrombocytopoenia as a child, recovered spontaneously just short of splenectomy. Presumably virus related.
I was booked for AZ vaccine, but have cancelled.
I am hoping Prof Cheng or another learned colleague may have advice. I would prefer to wait for Pfizer or other non virus vector vaccine at this stage. Prepared to self isolate if/when international borders open.
Over a long professional career, l think this is the first vaccine l have seen introduced to have death as a complication, though l stand to be corrected.
To Anonymous 1
We humans, even the highly educated are notoriously poor at assessing risk . We are emotional creatures and fear is a very powerful emotion. However when you look at overseas and the tragedies occurring there, the risk from covid is so real. We will have ‘our’ epidemic at some stage and in the panic vaccines will suddenly be hard to get
Based on the maths your risk from the vaccine is orders of magnitude less than the virus. Rely on the maths and not your emotional response and you’ll make the lower risk decision.
I am a registered nurse. I trained in the UK in the 1960s. We were taught to give intramuscular injections by:
* Inserting the needle into the muscle (whether arm, buttock or leg);
* Withdrawing the plunger of the syringe to ensure that no blood was aspirated;
* If no blood was aspirated we would inject the contents of the syringe into the muscle;
* If blood was aspirated this could indicate that the needle had pierced a blood vessel;
* The needle was immediately withdrawn and needle and syringe discarded into a sharp’s bin;
* Then we’d start all over again.
I see, on TV, injections being given by nurses without withdrawing the plunger. If the plunger is not withdrawn how can anyone be sure that the needle is not in a blood vessel and that the contents of the syringe are not being injected into the blood stream?
Could this perhaps be one cause of blood clots? Just a thought.
The Australian Immunisation Handbook basis it’s rationale for not withdrawing the plunger on one paper on pain in babies receiving injections where the plunger was withdrawn in half the babies and not withdrawn in the other half.
When doing a pubmed search however I found a few papers where aspiration of blood was shown to occur sometimes when plungers were withdrawn.
I want the nurse who gives me my vaccine to withdraw the plunger!
Unfortunately the bias caused by this announcement is that the clotting disorder is a significant risk. It’s not – it’s serious but very rare.
Covid is here for a long time and needs to be managed on a population basis so mass vaccination with the available vaccine (AZ) will save lives and limit morbidity (eg acute illness and long covid) with approximately 1 in a million chance of death from rare clotting disorder.
I’m getting vaccinated because I don’t want to get covid, I don’t want the risk of long covid (approximately 30%) and I want to resume normal life at some point as soon as mass vaccination will allow.
At 58 years of age with no underlying health conditions I am concerned about the risk, albeit rare, of VIPIT. Even though I’m a GP the risk of contracting covid-19 currently in Australia & dying from it is extremely low. In addition if community transmission occurs we have measures we can employ to avoid infection, whereas the occurrence of VIPIT after receiving the AZ vaccine is unpredictable, spans across all age groups, as seen overseas, & has an inherent 25% mortality. I am not prepared to take that chance.
It appears to many that the SARS CoV vaccines are rushed and therefore may be unsafe.