WHEN we look up at the stars at night, we can feel insignificant and small, overwhelmed by the vast number of celestial bodies surrounding us. If we take the time to keep looking, we will realise that the stars and planets do not stay in the same position but move across the night sky. Over a longer period, we would discover that these astronomical objects appear to revolve around us.
Claudius Ptolemy, who lived approximately between 100 and 170 AD, also discovered the same phenomenon. A polymath, he was a mathematician, astronomer, and music theorist, who, based on early astronomical observations, wrote a book titled Planetary hypotheses, in which he postulated that the Sun and the planets revolved around the Earth. This astronomical theory, known as geocentrism, became the accepted model for our understanding of the universe for the next 1500 years.
And it is no wonder that it was the prevailing theory at the time and widely accepted. From where we stand as human beings, we can observe two obvious things that support this geocentric model.
First, we can see that the Sun and stars do appear to revolve around the Earth in a consistent manner.
Second, the Earth itself seems stationary and immobile – we do not seem to be moving when we are standing still. Based on our own physical perceptions, it is not difficult, and it is even reasonable, to conclude that it is the Sun, the Moon and the stars that are moving and not the Earth.
However, we obviously now know that this model is, in fact, incorrect, thanks to Nicolaus Copernicus, a Renaissance mathematician, astronomer and doctor, who, a millennium and a half after Ptolemy, came up with an opposing theory based on his own scientific observations, which he first published in Commentariolus (or Little commentary) in 1514, before he released his magnus opum Dē revolutionibus orbium coelestium (or On the revolutions of the heavenly spheres) in 1543. In his works, he outlined his heliocentric theory of astronomy that posited that the Earth and planets revolved around the Sun, which was contrary to the prevalent scientific and religious beliefs at the time.
Less than a century later, we have Galileo di Vincenzo Bonaiuti de’ Galilei from Italy, also a mathematician and astronomer, who was almost a doctor (he apparently started medical school first because he thought that was more lucrative before he changed courses to pursue his true passion in mathematics after only one year in medical school). Galileo wrote Sidereus nuncius (or Starry messenger) in 1610, in which he supported Copernican heliocentrism, even though he ended up being investigated by the church for heresy in 1615.
Similarly, Johannes Kepler was a German contemporary of Galileo, like the others mentioned, a mathematician and astronomer, as well as a philosopher and music writer. He also supported Copernicus’ heliocentric model when he released a series of books culminating with Epitome astronomiae Copernicanae (or Epitome of Copernican astronomy) in 1621.
One reason why Copernicus, Galileo and Kepler rejected geocentrism was because of their use of telescopes and careful measurements of the movements of the celestial bodies. In a geocentric model of the universe where Earth is at the centre, the orbits of the Sun and planets do not trace out a smooth circle or oval around the Earth if you observe their paths across the sky, but rather follow patterns that resemble petals to a flower, paths that make many smaller circular orbits around themselves many times over as they orbit around the Earth. In fact, early astronomical charts based on the geocentric models showed chaotic orbits of the Sun and individual planets around the Earth.
It is only when you change the model to a heliocentric one, and put the Sun at the centre, that everything else falls into orderly place. The orbits of the Earth and the other planets around the Sun follow smooth circular or oval paths, and what we can see, and measure, start to make sense.
So why have I shared with you a brief history of astronomy? What does astronomy have to do with patient-centred care?
When I was an intern, I remembered how structured and orderly it felt working in an emergency department (ED), even though the environment itself could get busy. In an ED, I knew my place as a junior doctor. I had a resident, a registrar and a consultant, my medical team. I had a process of triage; I knew when to see a patient, examine them and order tests. I knew when to escalate, when to refer and when to discharge. To me, patients came and went in a predictable fashion, and I did my job.
Many years later, my daughter, who was a toddler at the time, became severely unwell with uncontrolled asthma, and I had to bring her to the local ED. I had to wait for a long time before being seen. I had contact with different health care workers – nurses, doctors (both junior and senior, and different ones over different shifts), pharmacists and radiographers. My daughter and I were moved from the ED to radiology, back to the ED, then to the short stay ward, and then to the paediatric ward.
I was given minimal information, and different teams did not seem to know what the other teams were doing, or for that matter, did not seem to even care, as long as they got what they needed. It was chaotic, like the orbits of stars and suns and planets rotating in unpredictable ways around me – each busy with their own thoughts and jobs.
This is when I had an epiphany – one that is obvious and experienced by countless other patients and family members who have come before me, and many more who have and will come after.
- MJA Supplement: Achieving person-centred primary health care: a value co-creation approach
- MJA Editorial: Achieving person‐centred primary health care through value co‐creation
Even though we say that the health system is patient-centred, it truly is not. We have designed the health system to be provider-centred. Health care workers have designed processes and workflows to be useful for them. For good reason – we want the health system to be efficient and lean. We need to cut cost, remove waste, and be cost-effective. To clinicians, the health system should revolve around them – in fact, for a long time, it has.
This means that when patients enter the health system, what they experience is separate and distinct contact with different health care providers and teams that appear to, and say that they do, revolve around the patients, but in unpredictable, chaotic, and “messy” orbits. Patients requiring health care need to speak to different people and organisations to make multiple appointments for times that suit the different care teams in a system that is clearly not designed for them, but designed over many years and iterations for the various components of the complex world that makes up our health care system.
All this, despite the fact that patient-centred care is now part of the language of every public and private hospital, and every project is now mandated to be co-designed with consumers. We are still living with the health model that is “provider-centric” rather than based on true “patient-centrism”. Clinicians are still the centre of gravity because we still have the locus of control.
This has to change.
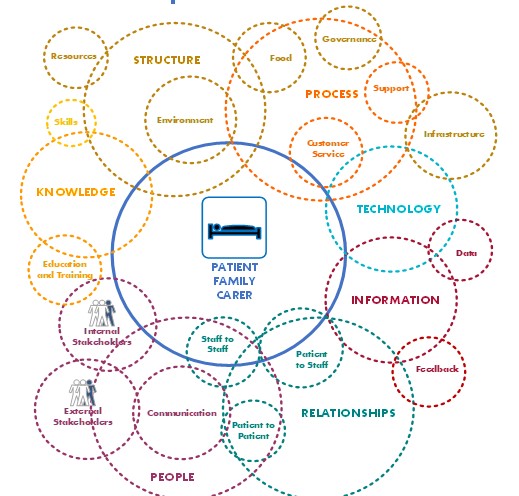
To be truly patient-centric, we need to take the radical step of dismantling the structures that already exist in the different care teams to make each of the parts separately more efficient, and really design from scratch a single system that does put the patient at the centre. This is so that, from the patient’s perspective, they are the ones that are truly stable and immobile, and they can experience health care teams around them in a predictable, orderly manner.
This is a model of a universe in which the patient has the control and ability to get the right care and right information from the right provider at the right time; a universe that is peaceful and structured to the patient, even if that is at the expense of more chaos, inefficiencies and costs for the providers (although this may not need to be the case). This model of the universe is “patient-centrism”. This model of health care may not be practically achievable in our current decentralised, fragmented and siloed health system, according to some people, and may even be considered heretical by others.
But I know that astronomy lived with the wrong model of the universe for 1500 years before a few came up with a new theory. I would rather suggest a new theory of health care today that could perhaps become the prevailing model, hopefully in a shorter period than that.
Professor Erwin Loh is Group Medical Officer and Group General Manager of Clinical Governance at St Vincent’s Health Australia.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Interesting view Professor Erwin Loh The tertiary care system is where being truly patient-centred, becomes complex and focus on this axiom is lost . The closer to primary care the person comes, the closer to receiving truly patient-centred care. Breaking down systems takes time & money – what if the next version gets it wrong? Supporting primary care, the medical home, using digital health & technology as enablers through inter-professional education – that’s the way to go. My thoughts….
Thankyou Erwin for your erudite representation of the single biggest challenge we face in healthcare. The same goes for and extends to after hours care, the construct of a 5 day working week.
Erwin come back to the world of the 21st century.
‘Patient-centered care’ is a rarity and, I would proffer is a myth purported by government and health bureaucrats’.
Firstly, as to my work within the Health Industry and secondly, my direct experience as a patient (sarcoma) including reading the medical literature and consultations with patients and those working in the health care system, there is a vast chasm.
Key Issue 1: is treating the person – Jenny, Luigi, Lee, Sally, Claude, Ali – the human being; not just a particular body part.
It is purported that specialists are time poor, therein, do not have time to know their patients – for me and others it is usually no more than a maximum of a 10 minute consultation to get results – by the time the specialist has stated the status re reports, treatment, etc the time is up and you are out the door – questions galore swimming in one’s head.
Stress and anxiety abound and this can have a multiplier effect on the patient ie the impact ‘stress’ has on the immune system and its relationship to metastasis.
What is required is “Whole-of-Person” care – the physiologic, emotional and spiritual. See: “Funding for Research into Cancers with Low Survival Rates. Submission 244”, page 2
Key Issue 2: is health practitioners working in ‘silos’ – communications between, for example, cancer surgeon, flap surgeon, oncologist, GP, wound therapy nurses and so on results in little understanding of the impact/outcomes for the patient as to their ‘Quality of Life’.
Key Issue 3: is patients’ reluctance to question the medical practitioner as to understand their own body, their health/wellness problem and the treatments/medications prescribed as to the side effects and impact on their health/well-being.
Key Issue 4: is that specialists are time poor therein, don’t have time to know their patients – for me and others it’s no ore than a maximum of a 10 minute consultation to get results – by the time the specialist has stated the status re reports, the time is up and you are out the door – questions galore swimming in one’s head.
References:
“Funding for Research into Cancers with Low Survival Rates. Submission 244”, page 2 and 9 [Inquiry by Parliament of Australia. Select Senate Committee into funding for Research. ‘Rare Cancers with low Survival Rates’].
“End of Like Choices. Inquiry by Parliament of Victoria. Submission_965_-_Bourne_and_Associates.
“Eat Bananas. Identity Abuse in the care of Older Australians.” Submission to the Australian Productivity Commission.
https://www.australianageingagenda.com.au/executive/the-neglected-form-of-abuse/
Anyone who has spent hours waiting in reception for a medical appointment knows the doctor’s time is valued far above the patient’s time. Overbooking is standard practice. No patient is told when they will be seen. Any anyone who walks out will never be given an appointment again.
Rather than analogising Copernicus, one could attribute patient-centred care to its true instigator, Hippocrates: “Into whatsoever houses I enter, I will enter to help the sick, and I will abstain from all intentional wrong-doing and harm…”
Hardly “a new theory of health care today”, an oldie but a goodie.
In any activity, there are many stakeholders who are affected. The stakeholders each have some influence on the activity, based on the power they have. That power does not necessarily corelate with the impact that activity has on them. Medicine has been a field where the patient had insufficient power considering the impact. However, in rectifying it, it does not mean that patients should have 100% of the power. Prophylactic antibiotics may benefit the patient, but causes public harm with superbugs, and the doctor needs to weigh the balance. Taxpayers and medical staff also have rights, which need to be weighed in the balance.
As a 68 year old GP ,I could not agree more with the author. Firstly as a medical student,then an intern,3 years as a Resident,two as a “Casualty Registrar” ,a year as a Career Medical Officer and then entering General Practice,with continuing educational requirements. I have observed the de evolution of what once upon a time was a better system where patints were rarely disharged without being fully sorted. The Outpatient Clinics served as the failsafe arrangement.
Accident and emergency departments once were able to easily move patients to an observation ward. Now they are under pressure to meet targets of first seeing the patient then either admitting or dischargeing within a certain time frame or risk budget cuts should these targets not be met. These departements are not judged on patient outcomes rather on arbitary bureaucratic targets. They are told to see their GP .