DURING Victoria’s recent fourth lockdown in June 2021 and the current lockdown of Greater Sydney, several positive COVID-19 cases have been reported in staff and residents in Australia’s residential aged care facilities (RACFs).
It has also been revealed that only just over one-third of RACF staff are vaccinated, despite being in the highest priority groups for early vaccination and despite the devastating impact that Victoria’s second wave of COVID-19 infections exacted on RACF residents in 2020.
Although Australia has recorded fewer COVID-19 cases per capita than most other countries, COVID-19 has disproportionately affected aged care residents, who account for 75% of Australia’s 904 COVID-19 deaths. This is one of the highest rates worldwide as a proportion of total deaths.
In early June 2021, 77% of respondents in an Australia Institute poll of 1000 Australians believed that COVID-19 vaccination ought to be mandatory for frontline staff in RACFs. On 28 June 2021, the Australian Government announced that they would make COVID-19 vaccination mandatory for these workers.
This article discusses the ethical issues surrounding mandatory vaccination of RACF staff. In particular, it looks at the potential benefits and costs of such a policy and explores the viability of less restrictive alternatives.
Defining “mandatory” vaccination
To address whether vaccines should be mandated in RACF workers, it is necessary to define “mandatory” and understand available alternatives. The Nuffield Council of Bioethics has formulated an “intervention ladder” for public health interventions of escalating restrictiveness, which can be adapted for vaccination policies (Table).
Table: Vaccination policy options for RACF staff
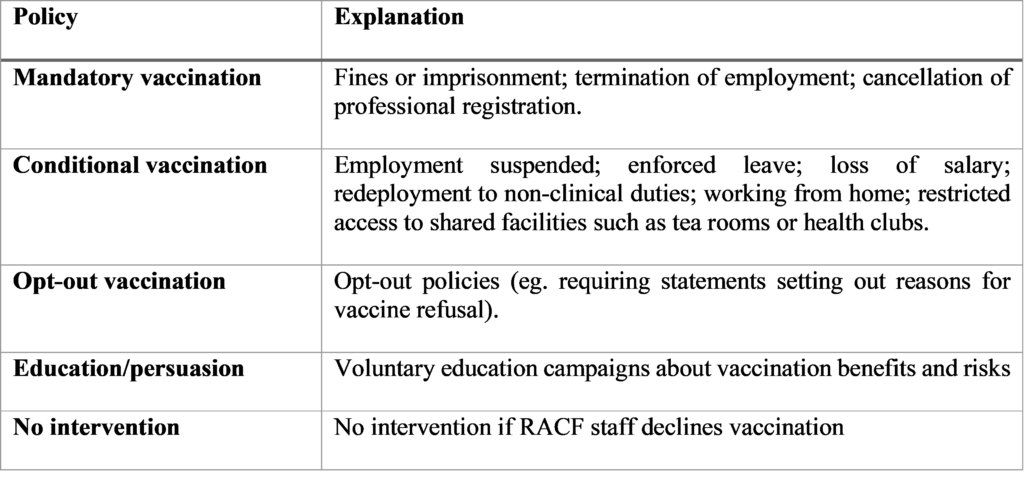
The details of the Australian Government’s vaccine “mandate” were published on 30 June 2021. It states that: “[t]he requirement will be a condition of working in an aged care facility”. Therefore, the current approach adopted by the government would, strictly speaking, appear to be a conditional rather than mandatory policy. As such, available alternatives may be more or less restrictive of personal freedom. However, for the purpose of this article and to avoid confusion, we will continue to refer to the policy as mandatory.
Effectiveness
Vaccination policies that incur personal costs must be effective in reducing the serious threat posed by COVID-19 in aged care. Mandatory influenza vaccination policies in US hospitals have increased vaccination rates and reduced patient morbidity and mortality. While more is known about the safety and effectiveness of influenza vaccines than COVID-19 vaccines, emerging overseas evidence confirms that approved COVID-19 vaccines are safe overall and highly effective in reducing transmissibility and serious infection, notwithstanding concerns about rare blood clots associated with the Oxford–AstraZeneca vaccine.
Unlike the community or hospital settings, staff working in RACFs spend long periods of time in close contact with residents to feed, wash, lift and assist them with personal hygiene. Therefore, RACF staff pose a particular infection risk to residents. Vaccinating RACF staff would directly protect residents. Indeed, the Strategic Advisory Group of Experts on COVID-19 Vaccines (SAGE) in the UK believes that sufficient protection against COVID-19 can be achieved if 80% of RACF staff are vaccinated. Currently, only 30% of RACF staff in Australia have been vaccinated.
Residents also pose an infection risk to each other since they share a confined living space. However, many vaccines are less effective in older people. Therefore, while vaccinated residents may still pose a risk to each other, vaccinated RACF staff are less likely to introduce infection from the community that can lead to outbreaks. Moreover, while 30% of RACF residents have declined vaccination, there is a moral difference between declining to protect oneself and declining to protect others. RACF residents can choose to be vaccinated but cannot choose who cares for them.
We therefore argue that the Government’s mandatory vaccination policy is likely to be effective if the goal is to reduce the risk of transmission of infection within RACFs.
Necessity
The second policy consideration is necessity. Public health interventions are necessary only when less restrictive alternatives are ineffective. Mandating vaccination would be necessary if less coercive options outlined in the Table would insufficiently protect vulnerable RACF residents.
In the case of influenza, we know that mandatory vaccination policies are more effective than incentives and education campaigns in increasing vaccine uptake among health care workers. Nevertheless, whether mandatory COVID-19 vaccination is necessary in the RACF context depends on the degree and speed of vaccine uptake required. If our target vaccination rate is 80% of RACF staff as recommended by SAGE, then Australia remains significantly below that target. Although active COVID-19 case numbers among RACF residents is currently low, we know that this can change rapidly as new variants spread. Therefore, coercive measures may be ethically justified in order to ensure that vulnerable Australians are protected in case widespread transmission occurs. COVID-19 represents a serious and imminent threat to RACF residents even during periods of low prevalence, particularly when vaccination rates among the wider Australian population are so much lower than comparable jurisdictions, such as the UK.
Even if a vaccine mandate is necessary now, this may change in the future if vaccine uptake increases to levels that afford sufficient protection to RACF residents, particularly if governments also seek to understand and address underlying barriers to vaccination among RACF staff through the use of incentives. For example, the Victorian Government recently announced that it would prioritise RACF staff presenting to its vaccination hubs, while the Australian Government has pledged $11 million to support RACF staff in receiving their vaccination through paid leave and incentive payments. If vaccination rates rise, these incentives alone may be sufficient.
Proportionality
Ultimately, the moral question of how best to balance public health outcomes against coercive interventions comes down to proportionality. A public health intervention is proportionate when the benefits achieved by the intervention are sufficient to outweigh costs. In the case of COVID-19, the desired outcome from vaccination is a reduction in transmission and serious infection, while the principal costs are liberty infringements, the risk of adverse vaccine reactions, and alienating RACF staff.
A mandatory vaccination policy is coercive because it exerts a controlling influence on RACF staff that can undermine the voluntariness of consent and decision making. This represents a significant moral cost for individuals who value their autonomy and privacy, breaches of which can lead to psychological harm. Moreover, there are more than 235 000 RACF workers in Australia. Mandating vaccination could impose coercive pressure on a large number of people. However, the right to autonomy is not absolute through a range of ethical lenses. In addition, many Australian health services already require employees to be vaccinated against, or prove immunity to, prescribed diseases. Therefore, liberty infringements alone are not a reason to reject a vaccine mandate.
Adverse vaccine reactions are another cost of mandatory vaccination. Information about rare complications from COVID-19 vaccines continues to emerge and understandably causes anxiety. Therefore, for a mandatory vaccination policy to be proportionate, it must mandate only the safest available vaccine based on scientific evidence at the time. In this regard, the Australian Government’s vaccine mandate includes the guarantee that all RACF staff will receive access to the Pfizer COVID-19 vaccine, for which there is mounting evidence of both safety and efficacy.
Finally, there are concerns that the vaccine mandate could drive low-paid RACF workers from the aged care sector. The recruitment and retention of RACF staff is already challenging and many Australian aged care workers have been emotionally and physically impacted by the pandemic. However, we believe that these concerns should not dissuade the government from its vaccine mandate because it is likely that the majority of RACF staff will ultimately agree to vaccination. This issue serves to remind us all of the importance of addressing vaccine hesitancy amongst all health care workers by engaging with RACF staff from culturally and linguistically diverse communities and by supporting conversations that address misinformation and fear.
Conclusions
During public health emergencies, understanding the competing rights and responsibilities of health workers assumes greater importance. Despite the personal and moral costs of a vaccine mandate for RACF staff, it will likely be the most effective policy in protecting vulnerable RACF residents.
Although there are currently low numbers of COVID-19 cases in Australian RACFs, this can change quickly and we ought not be complacent. Recent state and territory lockdowns exemplify this. Australia cannot keep its international borders closed indefinitely and, once they re-open, rates of infection will rise. It is essential that the Australian aged care sector is prepared for this by maximising vaccination rates. A vaccine mandate for COVID-19 is entirely consistent with legal mandates imposed on health care workers with respect to other transmissible infections and is also consistent with the ethical and professional obligations of health care workers more generally.
In our view, a mandatory vaccination policy for RACF staff in Australia is ethically justified and represents sound public health policy.
Dr Owen Bradfield is a doctor, health lawyer, 2020 Fulbright Scholar and PhD Candidate at the Law and Public Health Unit, Melbourne School of Population and Global Health, University of Melbourne.
Professor Dominic Wilkinson is a consultant in newborn intensive care and Professor of Medical Ethics at the Oxford Uehiro Centre for Practical Ethics, University of Oxford.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert
All those who voted strongly disagree should be deregistered.
And give up your drivers licences if you are that worried about a 1 in 50,000 clot risk, from which 80% recover anyway , as car driving is more risky.
The ANONYMOUS poster at 11:46 am makes several serious errors. First, these vaccines are based on technology that has been tested for years. All approved vaccines have completed Phase III clinical trials. We also have safety data from many millions of doses delivered all around the world. Effective vaccine campaigns in the UK and US have already shown a significant effect on infection and transmission. What would be unethical would be to allow COVID-19 infection to run rampant, or, alternatively, to keep borders shut and communities un lock-down long-term.
Next, anonymous claims that evidence of effect in producing immunity is “spectacularly lacking”. This is just not so. The evidence is presented here: https://www.gavi.org/vaccineswork/how-do-we-know-who-immune-covid-19?gclid=Cj0KCQjw0K-HBhDDARIsAFJ6UGhOipxV3Km_zVC_V1eoMjIQPUquAtmel9txTEkzsUVHPheA8_hkCKEaAnaXEALw_wcB
Whether a person posting anonymously claims to be “generally in support of vaccines” is neither here nor there. These vaccines HAVE been tested by the “usual means”.
Then, “anonymous” gives themselves away: the ivermectin chestnut. Some people believe that there is a worldwide conspiracy of clinicians, researchers, regulators and governments to “suppress” evidence that re-purposed drugs – in this case, an anti-helminthic – is an effective treatment for COVID-19 (and, between the lines, therefore we don’t need vaccines).
Next, the full conspiracist emerges: “This has been a conversation that has been silenced at every stage. Why should people trust what they are being ordered to do by governments when there has been persistent suppression of the debate itself and extraordinary misinformation being perpetuated by “authorities”?” Oops!
Perhaps this anonymous poster should review the data on people in NSW currently in ICU and on ventilators for COVID-19 infection, including how many of them were fully vaccinated.
The readership has good reason to question anonymous comments full of conspiracy theories and misinformation.
Residential Aged Care workers get the virus in the community. When the community uptake is as high as we needs it to be and every effort has been made to enable RAC workers get vaccinated voluntarily in high enough numbers then the ethics would become less troublesome. At 30%vaccinated , more of them have voluntarily done so than other sections of the population. We should be thanking them not implying negligent, irresponsible behaviour. The sub-group who do the real hands on care are young, the bread winners of their families, they cannot risk illness from side-effects in themselves – they must be provided with a vaccine that has the least risk to their safety if we are to mandate uptake. We are even having to consider this restrictive approach because of failings in other areas. If we are considering mandating in some groups in whom else should we do that?
Should family members of RAC residents be mandated to have the vaccine or not be allowed to visit?
Mandatory vaccination of anyone using vaccines with no long term safety data is highly unethical.
While there is an unspoken assumption that the vaccines stop spread of the virus, there is complete lack of evidence that the vaccines significantly reduce spread of new variants and no evidence that humoral (B cell) immunity, such as that predominantly induced by RNA vaccines (and a single resulting polypeptide), lasts longer than a few months.
Humoral immunity to the virus itself generally lasts less than a few months, so there is good reason to question the long term effectiveness of current vaccines. It is T cell immunity that seems to confer longer term protection and is generally far more important for these viruses, and evidence for this from current vaccines is spectacularly lacking. Furthermore, while I am generally in support of vaccines, the current RNA vaccines have not been approved or properly tested by the usual means. Rather they have been approved under “emergency use” legislation on the grounds that there are no suitable alternatives. However, information regarding efficacy of ivermectin (and several other pharmaceuticals) has been silenced and suppressed by main stream and social media and the authorities but now includes over 28 published double-blind placebo-controlled studies and more than 54 studies in all for various stages of the disease including prophylaxis. See the FLCCC website for details.
While more information is required, the Novavax vaccine sounds more promising because of possible T cell immunity. But again, mandating vaccination when there is no long term data is unethical.
This has been a conversation that has been silenced at every stage. Why should people trust what they are being ordered to do by governments when there has been persistent suppression of the debate itself and extraordinary misinformation being perpetuated by “authorities”? The lab leak hypothesis is a classic example where any decenters were silenced. The WHO denying airborne spread of the virus for the best part of a year, and it’s reluctance to acknowledge the effectiveness of high dose steroids is another. Again, the shaming and silencing of advocates of vitamin D is another. Yet vitamin D – both spectacularly safe and cheap – has now been shown to be of prospective benefit. It is apparent that the so called authorities simply haven’t read proper scientific studies and are ignorant of their findings. Mike Yeadon, the previous chief scientist for Pfizer, has stated that ivermectin is probably superior to vaccines, so this should at least be discussed – not silenced. Again, Craig Kelly was effectively silenced from presenting the scientific evidence for ivermectin in parliament. Not much of a democracy!
There is an assumption that the vaccines do what they claim. While there is complete lack of evidence for reduced transmissibility for new variants with those who have had the vaccine, why are vaccines being encouraged for anyone under the age of 50 with no other risk factors? One has to question the reasons for wanting to vaccinate younger people with a vaccine that has no long term safety evidence at all, and may have serious long term consequences that could outweigh the benefit of short term immunity to a virus that is of little danger to the young and healthy. Yet governments are doing this.
The public has good reason to question the competence of the government good reasons not to have the vaccine should they chose not to be vaccinated.
I think this is not easy. What is the objective of immunization of health care workers? To protect the workers? To protect patients?
I think there is good evidence of a high level of protection against clinical covid-19, particularly against hospitalization and death. My view is that current vaccines are effective in protecting the health of workers.
However, I think the evidence for prevention of transmission is nowhere near as good. The best study of which I am aware is that of Shah et al[1], who investigated cases in households of vaccinated and unvaccinated health care workers. They found the effectiveness of vaccination of health care workers in preventing cases in unvaccinated household members to be around 30%. There are some caveats around this result, the report is a pre-print, and effectiveness may be higher. While this level of effectiveness is helpful, it is not enough to prevent broad-scale transmission, especially for variant genotypes of SARS-CoV-2 with basic reproduction numbers of 5 or so.
1 Anoop S V Shah, Ciara Gribben, Jennifer Bishop, Peter Hanlon, David Caldwell, Rachael Wood, Martin Reid, Jim McMenamin, David Goldberg, Diane Stockton, Sharon Hutchinson, Chris Robertson, Paul M McKeigue, Helen M Colhoun, David A McAllister
medRxiv 2021.03.11.21253275; doi: https://doi.org/10.1101/2021.03.11.21253275
I thoroughly agree with this and cannot understand why it is not being considered at the same time. The latest fatality involving a 90 year old contracting Covid from her community carer is one good example of why this should be the case.
I would love to see mandatory vaccination also apply to disability residential workers, where at the moment it is just “recommended”. Another very vulnerable population.
I understand that some people may not want to be vaccinated, but there should be repercussions for that personal decision. The inability to work with high risk populations should be one of them.