AS part of the budget, the Australian government has announced $A65 million in additional payments to GPs in rural areas. The more “rural” the area, the more money GPs are paid.
But will this contribute to attracting and retaining GPs in these areas?
The plan will provide additional payments to GPs if they bulk bill, and so provide stronger incentives to bulk-bill more services.
Overall, the aim is to attract more GPs to rural areas, help existing GPs stay longer and increase access for patients by increasing bulk billing rates.
The basic Medicare rebate for a bulk billed consultation is $A38.75. GPs already get bulk billing incentives if they bulk bill under 16 year olds and Commonwealth concession card holders. Currently, GPs in metropolitan areas get a bulk billing incentive of $A6.50, and GPs in all rural areas get $A9.80.
The new funding will increase these payments depending on how “rural” the area is, with GPs in very remote areas getting $A12.35 compared to the current $A9.80 – an additional $A2.60.
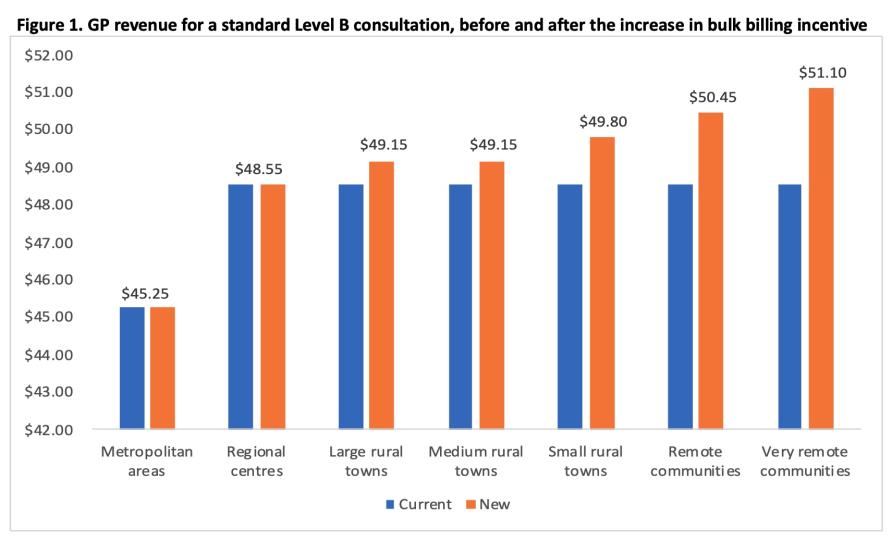
Figure 1 above shows the impact on a GP’s revenue for a standard 15-minute (or Level B) GP consultation that’s bulk billed for an under 16-year-old or a concession card holder. A GP’s revenue per consultation will increase from $A48.55 to $A51.20 (up by 5.3 per cent) in very remote areas.
Does this matter to GPs?
Though GPs will welcome this increase in income, especially after the Medicare Fee Freeze, it’s still unclear what this all means for the typical GP.
This is important to understand, especially if the policy is to work as intended – that is, attracting new GPs to rural areas, ensuring those already there don’t leave, and increasing bulk billing.
In order to get that big picture, GPs need to know how much the total revenue for an average GP would increase in each of these areas compared to their current revenue.
No modelling has yet been released to show how total revenue would change, but it will depend on a complex mix of the number of 16-year-olds and concession card holders seen by the average GP, the proportion they currently bulk bill, whether any additional services are bulk billed as a result of the change, and the mix of different types of consultation.
A key issue here is that these incentives apply only to these specific population groups and no other patients. But these groups will account for less than 50% of standard GP consultations.
Consultations for other patients just receive the basic $A38.75 even if in a very remote area.
So, the impact on total GP revenue is unclear, and it’s also unclear if this will be enough to encourage GPs to move and/or stay rural.
Will financial incentives increase recruitment and retention in rural areas?
There are already a range of policies to encourage GPs to go rural, including financial incentives under the Practice Incentive Program and the Workforce Incentive Scheme for GPs who newly move to rural areas and other health professionals employed in the practice.
Our previous research using data from the Medicine in Australia: Balancing Employment and Life (MABEL) survey has shown that to move a GP from the city to a rural area would take an increase in income of between 18% and 130%, depending on the rural area.
For an average GP who reported their annual income in the MABEL survey as $222 535, this means they would need to be paid between $261 700 and $511 830 to go rural.
These are very large increases and dwarf the likely amount offered by the new bulk billing incentives. Our research also found that 65% of GPs wouldn’t move no matter how much they were paid.
We have also evaluated the impact of a change to a rural incentive scheme (what was then called the GP Rural Incentives Program) that occurred in 2010, and that affected GPs outside of metropolitan areas, but not in very remote and rural areas.
This change had no impact on the number of GPs moving to these areas, or to the rate at which GPs left these areas.
But it did have an impact on the number of GPs in training, suggesting that younger and recently qualified GPs could be more mobile and willing to move, compared to GPs who are already established in cities. It seems that these GPs should be the target of policies using financial incentives.
Where to from here?
The single most effective policy for providing access to GPs in regional, remote and rural areas has been the requirement for all doctors arriving from overseas to spend up to 10 years in a non-metropolitan area, with around 40% of GPs in these areas having qualified overseas.
Many other policies also exist that support the education and training of doctors outside of metropolitan areas.
While reducing reliance on overseas doctors has been an objective of government policy, at the moment it remains unclear what other policies can be used instead.
Financial incentives might only work for younger newly qualified GPs and there is little evidence on the cost-effectiveness of other policies. So, it is likely that overseas doctors will continue to be used for the foreseeable future.
On top of this, the role of telehealth and other health professionals in rural areas also needs to be more carefully considered.
Though this budget measure puts more money in GPs’ pockets, by itself it is unlikely to help get more GPs into the bush.
Professor Anthony Scott is Director of the Health Economics Research Program at the Melbourne Institute: Applied Economic & Social Research, University of Melbourne.
This article was first published on Pursuit. Read the original article.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert
As a young, single, female GP who has only worked in rural areas a minor increase in the BB incentive is neither going to make me want to stay in the country or to BB more patients. Its nice to receive a slightly larger bonus for bb the patients that we already do but is laughable for the government to think that a $2 increase (for selected patients) will suddenly make me ignore the $50 gap between our private fee and the Medicare rebate for all patients.
As for rural retention the things that are actually going to influence me staying in a town are basically friends and the opportunity to have activities outside of work. And to be really honest, talking to other single, female doctors another big influence is whether we can find a partner in the area. Most of us want a family at some point and if there are no suitable single men within an achievable travel distance then we may move on.
Lots of interesting suggestions as regards “head hunters” and the relevance of cash incentives. As a 40+ year procedural rural GP who’s is slowly stepping into retirement I have found that 20+ years of educating med students and GPRs has produced very very few rural GPs despite most vouching for great pleasure in their placements. Very frustrating as our town is on the brink of medical break down with the loss of 3 GPs from our practice and a similar loss from the other 2 practices in town this year. Not to mention the imminent retirement of myself and 2 other senior doctors before we go out in a box! I think that a “Queensland model” of supported procedural GP public/private work with adequate team support and restricted on call duties produces a much better “hourly rate” than our days of 1 in 2 or 3 on call whence on-call for A&E/obstets/anaesthetics was busy and the significant income was well earned. One should note that until the Covid pandemic is controlled and international borders open there will be an absence and not just a shortage of IMGs able to apply for jobs with the certainty of actually getting to Australia.
I propose that we remove from discussion the notion that “doctors are paid” by Medicare
And also, largely, the per-consultation metric.
We charge for our service; patients claim (and assign, if BB) a rebate that includes an incentive for SOME
I propose that we speak, instead, of patients’ “purchasing power” for health care (not an original idea – I credit Dr Wendy Burton for opening my mind to a patient-centred perspective). And instead of per-consultation, we look at per-hour rates which drop off dramatically as consultation complexity (marked by duration) increases AND travelling time is lost between home, aged care and hospital
This change produces a modest increase in purchasing power for SOME patients only. Those eligible for the rebate who ALSO have (or will gain) access to doctors who’ll bulk-bill.
Let’s put the patient at the centre and see what’s on offer for THEM.
The evidence actually shows that if you train doctors rurally, they will decide to stay rural. That is the best and only long term solution. So: more rural medical schools and/or funded places and more rural training pathways and infrastructure. The last thing rural Australia needs is more OTDs. The extra money will not go to waste in between time.
I’ve worked in Rural/Remote ED and ED/GP for a long time. I do it by choice. The motivations for working in rural/remote Australia very from person-to-person and money is only part of it. Daily, I receive an email from one or other of the recruiting agencies listing the available positions – it’s ‘funny’ how the same places advertise OVER AND OVER yet can’t seem to fill a position. Yet, the employers never seem to ask WHY. Docs will be attracted to towns that have not just a job – if you have children, there must be schools etc. And we DO talk – “Don’t go to xxx ATM ‘ is common in airports/hospitals around the country. There is SO MUCH MORE that must change – using locums to do the shitty hours that no-one else will do; the huge exposure to potential medicolegal problems as the numbers of nurses and other staff/facilities are cut; the sarcasm and sometimes downright nastiness of some staff (yes, the nurses are the worst here – I can name a few places that struggle as it’s a common theme) make a lot of places a single rotation town. SO, here’s a novel suggestion – why don’t the politicians and administrators actually come and ask those that do the jobs what the problems are, instead of having yet another ‘committee’ , comprising the usual suspects, yet again rehashing the same old issues. Yeah, like that’ll happen.
Also, do the calculation on how much extra take home pay is available AFTER Tax, and work out why the increase in Medicare rebate means bugger all.
The question of education costs for children, as they grow up is another large problem, and as was mentioned earlier, what is the wife going to do, if she’s not a Nurse or a Doctor, plus the “bush nurses” don’t like working with Doctor’s wives (as Nurses), if the Doctor does work at the Hospital.
Many problems not understood by the academics, who find all these wonderful solutions.
The other major factor to consider, is that students who come from the bush are more likely to return there, than any city students ever would.
Great article Professor Scott.
Very much appreciate the comments too from George Burkitt. This distribution issue is a challenging one and there are many many human factors involved. I know I have heard comments from younger Drs that they would quit medicine if they were forced into remote. Others where workforce issues for partners or the need to find a partner is an issue. Childcare a prominent issue given the workload in a rural community & has also been raised by those in the field. The average age of registrars is now much older around 34 yoa so these people are not as young and not as mobile and have relational commitments that support their practice of medicine— a key part of human infrastructure. Medicine was rarely practiced alone. It’s a major problem with complexities replicated in international literature.
There are geopolitical considerations too given the infrastructure in remote and rural areas. Transport Technology and educational resources part of the equation. I agree with the comment regarding technology but this can’t be seen as a complete solution to rural workforce. Training requirements and advanced skills also a part of the deal.
Working through and understanding the vast body of research by those in the regions affected is key. Each region unique.
I think that there is a fundamental error in the way the fees have been calculated. Bulk billing allowances are only available for those patients who are eligible. Most patients are not eligible for a bulk billing allowance.
Even if all patients were eligible, the (touted elsewhere) figure of $50,000 pa to a bulk billing rural doctor equates to close to the maximum 69 services per day.
Access to locum services, transport, peer support, and markedly better behaviour on the part of State Govt. entities are also required.
The system simply needs flexibility, just like how the mining industry works. You can’t have a one box fits all approach. For example in areas without enough doctors for years, there should be a”headhunter” type approach like happens in mining and you just keep increasing the pay or specific conditions the doctor wants until the position is filled. Simple. Mining industry makes it work because they just pay double pay if they have to or change flexible FIFO arrangements until they get the right people in the position. Why don’t we employ a HR mining executive who has had experience in finding people to go to isolated areas to get the job done. Think like the private industry and you will solve your problem. Sure, it may cost more in terms of medicinal officer pay but that is supply and demand model, our problem is that we are still trying to use an outdated recruitment model for professionals. That’s why the locum industry works, locums list the money and conditions they are willing to accept individually. Long term the dividends will come in less morbidity and mortality in rural and remote areas and less reliance in retrieval’s. Having good health in a town also improves its local economy.
I’m not a GP, but after years in private practice in cities I now do some locum work in rural and semi-rural areas, and enjoy it.
However, about 8 weeks at a time is my limit. I think that is the issue – getting breaks from the full on location. The amount of extra money being offered to GPs is not enough to make much difference, and I’m not sure a lot more would. Quality of life and access to family is more important.
Scholarships for country students may help. Most of those who became country GPs in my graduating year were those who had grown up in rural areas.
Solo GPS in country towns are on call 24hrs a day, 7 days a week. locus support for weekends and holidays provides much needed breaks and may prolong stays in rural practice.
A realistic and factual assessment consistent with my experiences and views after more than 40 years as a GP (and then supervisor) in a wide range of environments including city, regional and remote. I wish I could see a long term solution. As I can’t, I’m retiring back to the city! Hopefully I will then be able to access health services if or when I need them!
Apart from income, a key reason for GPS not being attracted to rural areas is that their partners, who are usually also tertiary educated, have great difficulty in finding work. This problem is increased the smaller and more remote the country area. In a former generation, doctors were more often male with non- working wives so this was less of an issue. The quality of education for children is also an important issue. Now women are a much larger proportion of the GP workforce and their tertiary educated partners are likely to be in technical vocations much more sought after in major centers. GP couples might be more inclined to go rural with good support for locus etc especially if they themselves have grown up in the country. Older city doctors whose families are off their hands might also be encouraged to have a tree change with the right incentives.