STIGMA, bias and discrimination are keeping obese patients from getting the treatment they need in the public health system, says an Australian expert.
Professor John Dixon, Head of Clinical Obesity Research at Baker IDI Heart and Diabetes Institute, told InSight+ that public access to bariatric surgeries was “still terrible”.
While globally COVID-19 has caused delays in elective surgeries such as bariatric weight loss procedures, in Australia, the problem isn’t the pandemic — it’s the lack of public access to weight loss treatments.
According to the National Bariatric Registry, there were only 22 public hospitals across the country that reported a bariatric procedure in 2019. Of these, only 10 had a caseload of over 75.
Just 6% of metabolic procedures done in 2019 were performed in public hospitals. The other 94% were in private hospitals.
Bariatric surgery is currently covered by Medicare and most private health insurers also offer coverage. Medicare patients are entitled to subsidised medical services for bariatric surgery, provided they meet the medical criteria requirements – the patient must have clinically severe obesity (ie, body mass index [BMI] of 40 or more, or a BMI of 35 or more with other major medical comorbidities or obesity-related disease). Medicare items 31569 to 31581 and item 20791 provide for surgical treatment of clinically severe obesity and the accompanying anaesthesia service.
Individual private insurers can have differing terms and conditions for weight loss surgery.
“Public access is still terrible,” said Professor Dixon.
“Its impact on the nation’s obesity [levels] is trivial. It’s particularly difficult for regional centres. Most people with clinically severe obesity don’t get any attention at all.
“It’s not [the obese person’s] fault. They could do all the exercise in the world; they could try dozens of diets. They learn it doesn’t work. They float up and down. Yet they still blame themselves and they still feel it’s their fault because they lack willpower,” he said.
“We’ve got to understand we need to treat those with severe obesity with proper treatment like we do every other disease like cancer, diabetes, heart disease etc.
“The main problem with managing obesity today is weight stigma, bias, and discrimination. There is no reason why these very sick people are not treated at public hospitals and other hospitals with appropriate treatment other than those reasons,” Professor Dixon said.
This lack of access is not new. Many studies have detailed the socio-economic inequalities in access to bariatric surgery. However, the fact that there has been little improvement is concerning.
Fortunately, there are a few reasons for cautious optimism.
In late 2020, the Australian New Zealand Metabolic and Obesity Surgery Society (ANZMOSS) created a National Framework to provide clear guidelines for health policymakers, clinical governance boards and health practitioners.
They developed these guidelines with the Collective Bariatric Surgery Taskforce to provide efficient, patient-centred care, sustainable use of resources and provide surgical care to the most appropriate patient populations.
The report gives a detailed analysis on how to determine eligibility for bariatric surgery and then how to triage priority.
It talks about the surgery recommended including gastric banding, biliopancreatic diversion and gastric bypass, although according to Professor Dixon, the current worldwide trend is sleeve gastrectomy.
It also covers the end-to-end service including the importance of patient education and post-operative care, including clinical and annual dietetic reviews.
The first National Framework for Clinical Obesity Services in Australia was developed by the newly created National Association of Clinical Obesity Services (NACOS).
The framework aims to offer practical guidance on how to best provide weight management services for health care professionals, consumers, those working in the health insurance industry, and policymakers.
Approximately 7 million of people have clinically significant weight-related health impairments. In the past, obesity has been blamed on individual risk factors (biological and behavioural).
However, according to the NACOS framework, it’s now recognised that “increasingly ‘obesogenic’ environments and their interactions with individual risk factors most likely explain the rapid worldwide changes in body weight and the differences in obesity rates between countries”.
While frameworks and guidelines have now been developed, progress is slow, mainly thanks to COVID-19.
“It’s hard to get traction at any time but even more now with health being a major issue over the last few months,” Profession Dixon admitted.
According to Dr Evan Atlantis, Secretary and Founding President of NACOS, the guidelines have renewed interest in the area and health ministers across the country have responded positively so far.
“We would welcome the opportunity to work with all state/territory governments to help implement the recommendations in both frameworks,” Dr Atlantis told InSight+.
The seeds are sown for a much better deal in Australia. Hospital and allied health services recognise weight management services in our public hospitals are inadequate and need to change.
It is hoped that with the rollout of the COVID-19 vaccine, there may be an increased focus on improving services for people suffering from obesity.
Professor Dixon hopes the message gets through that obesity is a chronic illness and not an individual’s fault.
“Shaming and blaming is never a way to treat a chronic condition, it just makes it worse,” he concluded.

 more_vert
more_vert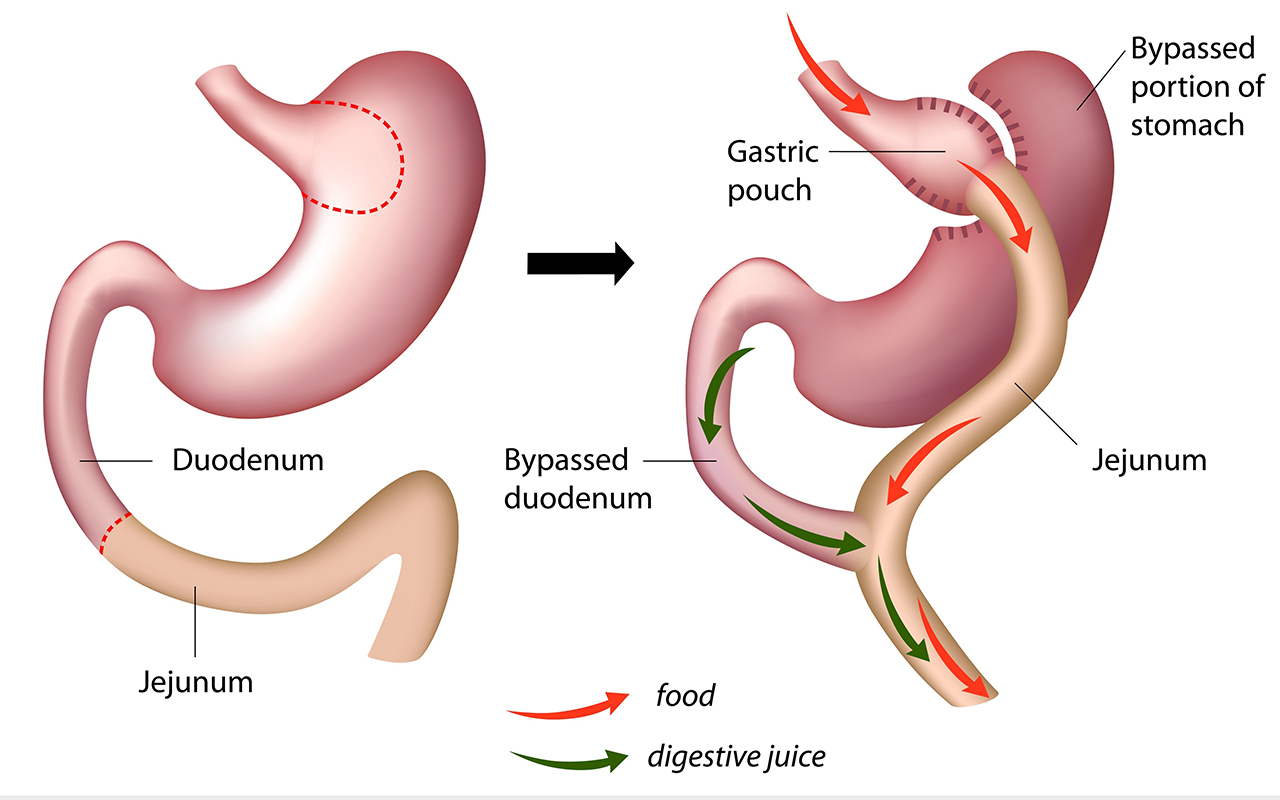
As a GP who tries to advocate for and exemplify Lifestyle Medicine, I’ve gotta admire Andrew Renouf,..A general surgeon who rather than making a living for himself from gastrointestinal plumbing on the unaware, preaches healthy activity and nutrition.
Is “ Bariatric Surgery “ evolving into a niche industry (like Cosmetic Surgery), in need of marketing and seeking the holy grail of Medicare funding?
One final comment: I consider the $700 million (approx) that is currently spent treating 30,000 patients (approx) with bariatric surgery annually would be much better spent on educating the 15 million who have the same condition.
Diets “don’t work” because people don’t stick to them. It needs to be a total lifestyle change involving a decent diet (mostly vegetables and stuff that actually looks like food and no soft drink – ever), intermittent fasting (which busy, active people tend to do without thinking about it), regular exercise (including incidental exercise on a daily basis). Give me a group of obese patients for at least 4 months where I have total control over all these factors and I am certain I could have the same or better outcome vs surgery and for a fraction of the cost (as Andrew Renaut pointed out- this trial is yet to happen)
John when you say that bariatric surgery works physiologically I’m assuming you mean that it’s removing the ghrelin-producing part of the stomach. Which is pure happenstance, because the original intention of the operation was to enforce calorie restriction which of course has been proven to fail because this shuts down BMR and the calorie deficit is quickly lost, hence the plateau.
The physiological aspect that needs to be addressed as I mentioned before is IR which develops secondary to the pancreas being forced to produce ever-increasing amounts of insulin. And undoubtedly the latter is secondary to a psychological problem, namely the addiction to refined carbohydrate. IR itself shuts down BMR. So the answer is to remove IR, boost BMR and establish a calorie deficit at the expense of calories-in. All of this is explained in my book The Users Manual For Your Body. I’ll happily send you a copy.
Introducing an anecdote (bariatric surgeons themselves undergoing surgery) I’m afraid weakens your argument.
Oh, I wish bariatric surgeons would understand the mechanisms of bariatric surgery. Surgery works physiologically not psychologically or behaviourally.
I know many bariatric surgeons who have had surgery. None changed their behaviour!
It’s not a defect of will power but a neurobehavioral disease the surgery usually effectively treats.
In the ‘real world’, where you end up living really matters.
When it comes to treatments, access to adequate clinical obesity care is very limited in our health system, as it is elsewhere in the world. And this is especially so for those living in socially disadvantaged communities which determines your chance of both having obesity and accessing treatments.
Our vision at the National Association of Clinical Obesity Services (NACOS) is to “live in a society that provides timely and equitable access to the best available care for the effective management of obesity and its complications.”
If you are a health care professional who shares our vison, you should join NACOS now: https://www.nacos.org.au
You can also download a copy of the first National Framework for Clinical Obesity Services on our website:
“insanity is doing the same thing over and over again and expecting different results” – we all know the individuals with weight issues have tried the same so called ‘treatments’ which have never worked for them and some still want us to continue the same!!
we need to look at funding so much more than the actual surgery – there needs to be careful patient screening, education, expectation matching and mental health support in addition to lifestyle modification training/coaching – funding the simple surgical episode without the prehab and the rehab wont’ change much…
@ Anonymous 11.43. Much like the surgical solution for treating an infective process (H.pylori). But not before millions (literally) were subjected to a partial gastrectomy. It’s called surgical dogma. Plus ca change……..
And I repeat – I’m a general surgeon.
Whilst we are happy to offer publicly funded treatments for the complications of severe obesity; diabetes, hypertension, dislipaemia, GORD, arthritis, etc, not offering effective treatments for the root cause of most of these conditions, i.e. the severe obesity, does not make any sense. This approach of only treating the complications, is not only more expensive, but is also nowhere near as effective as treating the obesity.
It is analogous to repeatedly painting the ceiling, painting the walls & changing the carpets in a house that has a leaking roof, rather than repairing the leak in the roof.
Whilst I agree that preventing obesity should also be a major focus, there are effective treatments (demonstrated in RCT trials) for managing severe obesity; including lifestyle measures, pharmacotherapy & bariatric surgery. We should therefore provide universal access to all of these treatments rather than only providing treatments which help with the downstream effects of obesity.
I have long been sceptical of a surgical solution to an overwhelmingly psychiatric problem.
The bariatric surgeons could help their cause by conducting a randomised controlled trial. Just one would do. Bariatric surgery versus a full-time lifestyle/health/counsellor for 4 months because that’s what you could get for $25k ie the cost of the operation. Bariatric surgeons are free to admit the operation only works in patients who also make the lifestyle changes. And those changes need to specifically target the underlying problem, namely insulin resistance (IR). IR causes obesity not the other way around which is why the only sustainable method of maintaining a healthy weight is intermittent fasting and eliminating refined carbohydrate. Bariatric surgery does not achieve this.
I’m a general surgeon who does not do bariatric surgery. For good reason
So many people are essentially being palliated for a treatable condition. So many are severely disabled by a treatable condition. The rich and the middle class have a way out with private insurance or paying out of pocket, it is only the poor that must die or live disabled. Non-surgical pharmacological treatments are also prohibitively expensive and not covered by the PBS. Well said Prof Dixon -“This is a human rights equity issue based on stigma, bias and overt discrimination.” Couldn’t agree more.
Heath systems have a right to be concerned about epidemics. The answer is to take them on in a positive manner; not simply ignore them.
The current obesity epidemic generates many of the admissions related diabetes, cancer, heart disease, and, yes
major joint replacements.
Discard myths and look at the facts. This is a human rights equity issue based on stigma, bias and overt discrimination.
Unfortunately all the talk of “obesity epidemic” scares administrators into avoidance of an “obesity surgery epidemic”. Our public health system is not equipped to deal with a deluge of patients equivalent to those awaiting joint replacement surgery. Saying there’s inequity over and over again does nothing; providing a robust selection criteria that can act as a gatekeeper to keep numbers serviceable should be the imperative. This will be different to the selection criteria used by some in the private sector, hence a moral dilemma: provide service to a select few public patients or (essentially) no service at all?