TRANSCATHETER aortic valve implantation (TAVI) is now the recommended intervention for severe aortic stenosis in elderly patients or those with significant comorbidity (here and here). At the beginning of 2020, TAVI was a treatment option for patients in all states in Australia, except Tasmania.
Collaboration between Tasmanian Health Service stakeholders and clinicians led to the development of a statewide Tasmanian TAVI service. The new service was to be ratified by the national TAVI Steering Committee following a period of direct clinical supervision and proctorship of 10 successful TAVI cases. In 2020, Tasmanian patients with severe symptomatic aortic stenosis, deemed suitable by the local heart team for TAVI, would no longer have to travel interstate for treatment thanks to the new service. This would allow for timely patient access to care and have beneficial economic benefits for Tasmania, which has the highest proportion of patients over the age of 65 years in the country.
But then the unprecedented COVID-19 pandemic happened. The respective state health services properly acted to reduce direct contact, meetings, training and travel between specialists from different states. Quarantine restrictions also posed a threat to the new TAVI program. We describe how the new TAVI program was, nevertheless, successfully established during the pandemic.
As has been described elsewhere, the rapid evolution of TAVI therapy has seen the need for specialised training and mentoring programs. Preceptorship involves the preceptor: a trained and experienced TAVI specialist is responsible for the procedure, supervises in person, and can take over if a situation demands. Proctorship is the next phase. A proctor – or observer – supervises as the TAVI trainee retains overall responsibility for the care of the patient.
An experienced Victorian proctor and TAVI device representative provided clinical and pre-procedural support via teleconferencing. Procedural dates were scheduled and suitable patients carefully selected. Approval for the proctor to travel to Tasmania was sought from the Tasmanian Health Service and an essential traveller permit was approved. The first six TAVIs were successfully performed without complication at the Royal Hobart Hospital with proctor clinical oversight.
The emergence of the COVID-19 second wave in Victoria led to the implementation of Stage 4 restrictions and the Tasmanian state border was closed to non-essential travellers from Victoria. This posed a serious logistical challenge for the TAVI service and a strong possibility that it would be furloughed until state borders were reopened. In addition, Tasmanian patients with severe aortic stenosis would face significant challenges travelling interstate for treatment, including quarantine restrictions and the risk of COVID-19 infection.
After careful consideration by stakeholders, a proposal to perform the remaining four TAVIs via teleproctoring was submitted and approved by the national TAVI Accreditation Committee.
International experience with teleproctoring in cardiology has recently been reported. The required IT equipment and support were provided and redundancy was set up in the system to ensure that audio-visual access was live-streamed. The proctor joined a teleconference from their Victorian-based hospital office computer into the hydrid operating theatre at Royal Hobart Hospital with real-time, digital, bidirectional audiovisual communication (FaceTime with iPhone and iPad; Microsoft Teams and Microsoft HoloLens 2). The proctor could visualise live fluoroscopy and haemodynamic measures during the entire procedure and provide real-time guidance (Figure 1).

Figure 1. The TAVI proctor viewing procedural fluoroscopy and haemodynamic information with real-time digital bidirectional audiovisual communication.
The proctor could visualise the TAVI operators’ field of vision and communicate directly with them via an augmented reality headset (Microsoft HoloLens 2; Figure 2).
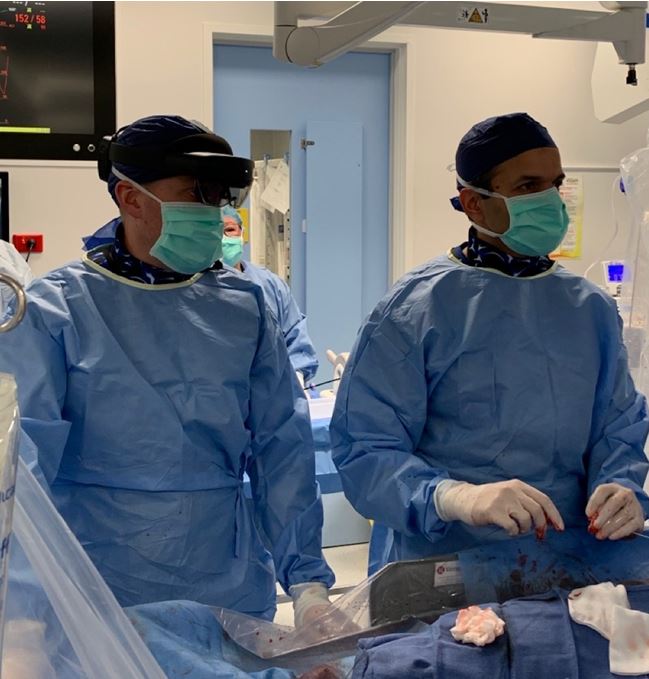
Figure 2. The TAVI operator with augmented reality headset (Microsoft HoloLens 2)
Teleproctoring was successfully delivered during these four TAVIs without procedural complication, and the Tasmanian Health Service successfully satisfied proctorship.
The COVID-19 pandemic will likely have a lasting impact on the way health care and procedural training are delivered. Our experience demonstrates that with collaboration between Australian state health services and clinicians, a state-wide clinical service can be established during a pandemic and teleproctoring can be a successful alternative to direct in-person clinical proctorship.
We wish the new Tasmanian TAVI Service a bright and successful future.
Associate Professor Sonny Palmer is the clinical lead for the Structural Heart Program at St Vincent’s Public and Private Hospitals in Melbourne. Sonny is a Clinical Associate Professor at The University of Melbourne, and is a qualified clinical proctor in TAVI.
Dr Umair Hayat is an Interventional and Structural Cardiologist from the Launceston General Hospital. He performed a TAVI fellowship at The James Cook Hospital in the UK, and performs TAVI procedures at the Royal Hobart Hospital.
Dr Heath Adams an Interventional and Structural Cardiologist and is the clinical lead for TAVI for the Tasmanian Health Service. He is a nationally accredited TAVI practitioner after a dedicated training post at St Thomas’ Hospital London, and is a Dr MG Ciezar Scholar from the University of Tasmania. He also holds an Honorary appointment at St Vincent’s Hospital Melbourne.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert