GPs with mental health expertise are leaving the profession, leaving a worrying gap in the delivery of vital frontline mental health care, writes Canberra GP Dr Louise Stone.
In part one of this two-part series, I introduced the concept of mental health generalism, a term I use to describe the core skills required to assess and manage common mental disorders and address other conditions that can profoundly affect mental health.
This kind of work is done predominantly by general practitioners, although generalist nurses and nurse practitioners, particularly in rural and remote settings, do this work as well.
Unfortunately, GPs with expertise in mental health are leaving the profession.
The reason for this shift is clear; I have written before that mental health generalists are underfunded, underestimated and appear to be undervalued.
How are mental health generalists trained?
All GPs are trained to provide mental health care, with mental health deeply represented across the curricula and Fellowship examinations of the Royal Australian College of General Practitioners and the Australian College of Rural and Remote Medicine.
Every workforce is uneven in its skills and capacities, and there is no doubt for every expert mental health generalist, there are others in the GP workforce who lack the skills and motivation to do this work.
In addition, there are GPs with considerable mental health skills, including self-funded Masters degrees in Psychiatric Medicine, Family Therapy and Psychotherapy.
Many more have had years of training in psychiatry, social work or psychology, or simply had a lifetime of supervised expert practice.
I believe these expert mental health generalists are prevented from doing the work they are trained to do by structural and policy impediments.
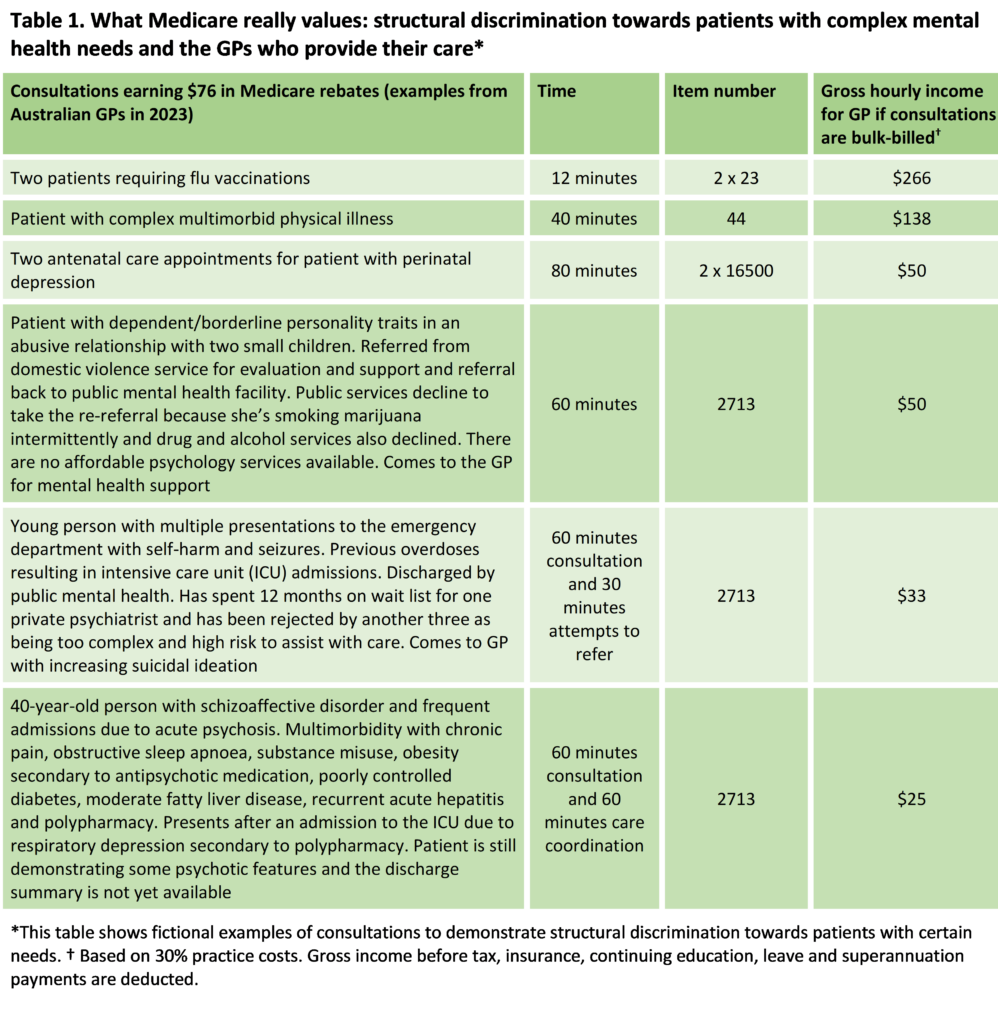
Those who do make a personal commitment to subsidise the Australian health care system by continuing to care for Australia’s most vulnerable patients do so at the cost of their business’s financial viability. I have given examples of this in Table 1.
Training cannot fix this problem.
Although it is tempting to respond to the problem of mental health care gaps by upskilling the least capable GPs in the system, subsidising training while disincentivising practice is like putting a foot on the accelerator and the brake at the same time.
It can’t improve the capacity of general practice to deliver better service.
Why are mental health generalists leaving the workforce?
Our health system is dependent on volunteer GP labour.
Governments nudge GPs into financially unsustainable bulk billing, by feeding the narrative that this is what the public deserve.
GPs enable public dependency on cheap primary care by donating increasing amounts of time, energy and skill for the sake of their vulnerable patients.
The inability to care for our most vulnerable patients and the moral distress of realising how deeply financial exploitation extends are destroying the workforce.
The only way to effectively manage this unhealthy dependency is to walk away, and mental health generalists are leaving.
The attrition of GPs has been devastating for many communities, particularly in rural and remote Australia.
If we lose mental health generalism – and we are losing the GPs doing this work through financial and emotional bankruptcy – we also lose other capacities.
Losing female GPs
Many of the GPs doing this work are women.
It is common for women to carry the emotional labour of the workplace, and for this work to be partly responsible for the gender pay gap.
As we lose mental health capacity, we will also lose workforce expertise and capacity in women’s health and complex chronic care.
Saving mental health generalists from extinction
Mental health generalists have become an endangered species.
Hopes to replace these expert generalists with teams of subspecialised experts in psychiatry, psychology and social work assume there is a well trained and distributed psychiatry, nursing and allied health workforce willing to work for $50 per hour.
To replace mental health generalists, we would need to backfill generalist diagnostic and management skills into specialised disciplines.
New multidisciplinary team structures would need to have the capacity to make physical as well as mental health diagnoses, manage multimorbidity, and maintain a system with no barrier to clinical entry.
More realistically, we could support mental health generalists to do the job they are trained to do; that is, reversing policy disincentives to do mental health work.
Maintain a diverse and skilled workforce without a 30% gender pay gap.
Offer psychiatry, psychology and social work consultants, not just specialists, so GPs can bring in clinical expertise, rather than refer patients out to yet another complex team.
In doing so, we could save the mental health generalists we have left before they are nudged out of the workforce altogether.
Psychiatrists, psychologists, mental health nurses and social workers are obviously critical members of the mental health workforce.
However, they are not the experts in the management of patients who they never see.
It is time to support mental health generalists and recognise them as the experts they are.
This part two in a two-part series in on mental health generalism. Read Dr Louise Stone’s first article published last week.
Dr Louise Stone is a Canberra GP with clinical, research, teaching and policy expertise in mental health.
She is Associate Professor in the Social Foundations of Medicine group, Australian National University Medical School.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Thank you Professor Stone for another excellent piece. I spent almost 1.5 hrs with a patient today and would have been reimbursed approx. $45 for that work.
I’m not going to privately bill someone who is vulnerable and facing homelessness but I can see how others cannot do this work. Currently I have a very limited number who have a bulk billing arrangement and the money I get from ‘easier’ presentations is use to justify billing them.
Another female ex-GP turned psych reg. I’m still early on in my training but I can’t see myself going back to GP at this point. No one has replaced the level of care I was providing to my GP patients.
This article is so true, I am a female rural GP and within the last month I left GP work.
Being a person that patients felt they could talk to meant that they were revealing the mental health burden of their conditions to me. Even a “simple script” for blood pressure medications in the town of Lismore would turn into a long consultation, with PTSD after the flood, non-compliance with routine healthcare after their home was washed away, insomnia and chronic pain, worsened by having to clean up after a disaster.
The threat of Medicare compliance letters has also been a big issue, with a RoboDebt-like approach to how I have ordered tests and services. This threat has disproportionally targeted female GPs because we look after more tired women as patients and because people want to talk to us.
I left General Practice so I can focus on consultations which don’t include mental health and complex chronic care. I am earning far more, getting home on time and not getting called after hours. I despair for the future of healthcare in Australia, it is entirely supported by the GP and yet the GP is undervalued, underpaid and under appreciated. No wonder it is not seen as a career option for new medical graduates.
Gosh that Table 1 is a slap in the face when you see it in writing, hey?
I particularly love your comment
“Psychiatrists, psychologists, mental health nurses and social workers are obviously critical members of the mental health workforce.
However, they are not the experts in the management of patients who they never see.”
Mental Health Generalists are lost in the GP realm and go unrecognised by others in the profession.
Fellow of Australian College of Psychological Medicine was formed in year 2000,
and then disintegrated into a Society for want of focussed training input and enthusiasm.
It is time for wisdom from GP academics like Dr Louis Stone to be recognised by all Colleges and the profession in general!
Struggling along in rural with zero other resources than the local mental health team, I constantly get that more complex cases are “ not in their remit”. That a distressed and potentially psychotic patient has used marijuana once for their distress, so they should be under drug and alcohol services. That a head injured, epileptic, depressed patient with ADHD is not entitled to a medication opinion for their depression because of their background ADHD.
( and there’s no way they can afford to get their ADHD diagnosed and find a treating/ overseeing psychiatrist at $1000 for the assessment and then $300 for the prescription appointments, even with the GP doing the heavy lifting to get the patient worked up and monitored
Oh and the rebate for what often turns into an hour of mental health anguish is around $75 At least if they had a sprained ankle that took as long to treat, the patient would get back $113….
Why didn’t I do advanced psychological medicine training? Well, I didn’t want to spend all day being battered and devalued by a system where the triage nurse or the bureaucracy can decide what my complex patients are allowed to have as conditions before they offer any help
This is exactly my story. Six months into psychiatry training, doing much easier work for not much less pay, even as a registrar. I self selected into mental health. I was never much interested in the more lucrative parts of GP. I doubt I’ll be back.
Reminds me a bit of The Relative Values Study if anyone is old enough to remember that .Again , a great article ,policy makers should take note.
Thank you for this article.
As a female GP in a large rural town, managing the combination of mental health & complex health conditions is core to my work.
There is not only a lack of funds for training, Medicare acts as a barrier to appropriate billing let alone adequate billing. It is common to have a 2713 + 23, 36 or 44 billing rejected & hence we give up that battle with Medicare & artificially compartmentalised our patient’s health & literally halve our income.
I have argued that the same payments made for procedural skills training for rural generalists should be extended to both mental health training as well as other chronic disease special interest training.
Thank you for this article Dr Stone. I have always taken pride in my work in mental health, but aware of the cost to our practice and to myself. I feel seen by your article.
Every day I feel more burned out and look at taking a break from general practice to do something else. I feel bad for my patients as we are so short of GPs here no one has much capacity. We need urgent health reform.
Wonderful analysis of the business realities facing practices. And let’s not forget the fact that expenses are soaring, whilst the Medicare rebates stagnate.
Absolutely spot on Professor Stone. There has long been a resentment that the skills of mental health Generalism are not valued as much as a procedural action oriented skill. Both are skilled but only one gets a high value and therefore social capital status. Care work traditional undervalued underpaid and unseen. The invisibility reflected that across the budget the GDP contributions of voluntary domestic labor are not included. That’s billions of dollars of productivity donated and uncounted. Moreover it’s assumed. In Finland in 1975 women stopped voluntary labour and the country ground to a halt.
In the 1980’s Professor Carol Gilligan contributed research that articulated an ethics of care approach to sociology and culture.
This age old bias is built into the structures of the MBS and it firmly belongs in the last century. ANU academic and labor minister (Professor) Andrew Leigh ( Assistant Minister for Competition, Charities and Treasury) has written a hopeful book called “Reconnected A community builders handbook”
There are many of all genders recognising the shift and absence and low value applied to “care”. The relative values study applied to Medicare Benefits Schedule was ahead of its time. It continues to be quoted but not applied. The only answer to that deficit is bias. Bias against care. Bias against reform. Bias against work that is hard to measure and easy to dismiss. Yet consider the following.
We can fly rockets to the moon, but cannot solve intractable diplomatic issues around the world. Soft skills are hard. Care actually works from infants to aged care.
So a perfect storm of bias traditional power structures and wilful resistance to necessary change has brought us here.
Mental health is the canary in the coal mine of larger cultural issues.
It’s all of our concerns and women (and all who work in GP mental health) leaving medicine are just another symptom of the need for a monumental shift.
It’s long past time to act. Care must be integrated into every strata of our society. It’s urgently need to restate our commitment to care and this includes funding that unique expert complexity that GP mental health generalists bring.