The sad thing is that the system is behaving the way it was designed to do. Intentional or not, the demise of good general practice has been predictable for decades. The question remaining is whether the community is happy to let it go.
LIKE many of my colleagues, I couldn’t sleep on Monday night after watching the ABC’s 7.30 report. I was trying to make sense of the articles and newspaper reports claiming doctors were rorting Medicare to the tune of $8 billion a year.
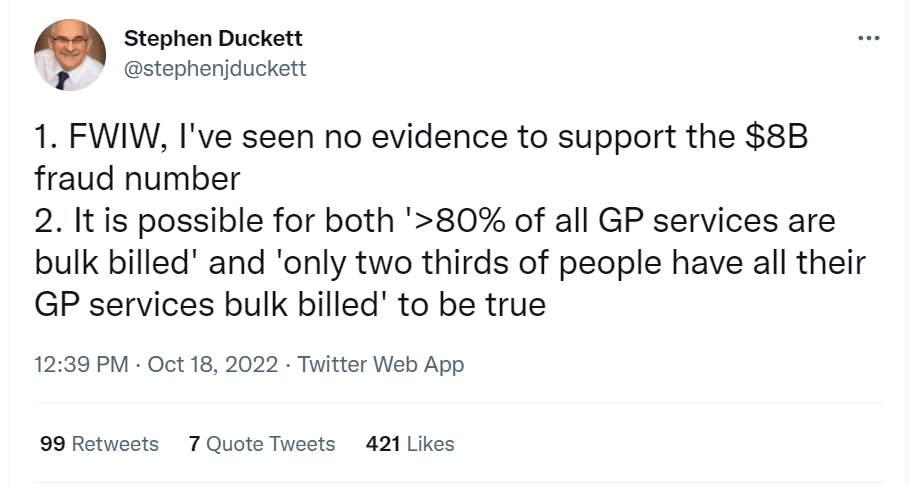
The evidence for this claim is poor. It conflates fraud, “low value care”, misunderstandings of the overly complex MBS schedule and over-treatment motivated by profit. However, to the community, the rhetoric is much simpler. Greedy doctors are “ripping off” the taxpayer and doctors are treating patients inappropriately for financial gain.
There are instances of fraud, over-billing and inappropriate practice in any profession, and medicine is not immune. We should be responsive to legitimate criticism, and the community have a right to understand and expect good care and appropriate stewardship of the Medicare dollar.
However, the scale of this claim is immense. If it were true, it should trigger a fundamental rethink of the way medicine is financed and governed. However, if it is a vast overestimate of the problem, and many experts believe it is, the claims of widespread, callous, deliberate profiteering are a deeply damaging misrepresentation of who we are as a profession.
The impacts of the “Medicare rorts” narrative on general practice
GPs across the country are feeling the impact of recent attacks on our competence, professionalism and ethics. Patients are refusing to pay because we are apparently “rorting the system”, our staff are experiencing escalating abuse. More insidiously, media campaigns damage trust, and we need trust to be able to work with our patients to achieve health outcomes. It is exhausting and demoralising to endure these attacks on our reputation, but more importantly, it’s another nail in the coffin of general practice.
Caring for the community is a privilege and the genuine gratitude we feel for the patients who simply thank us when we go above and beyond is precious. But the balance is shifting, and the cost for us is beginning to outweigh our commitment to serve our communities. Which is why general practice is shrinking rapidly, and the GP is becoming an endangered species in the ecosystem of medicine. Frankly, our habitat, the environment in which we can flourish or even survive, is under threat.
The attacks on my beloved profession in mainstream and social media in recent years have made me feel sick. But I have finally recognised what was going on. The “heart sink” feeling we are experiencing demonstrates that the relationship we GPs have with governments, organisations and some sectors of the community has become emotionally abusive.
The social contract between GPs and the community they serve
I’ve been a GP for 30 years. We do what we do as part of a social contract. When I trained, that contract was clearer. I agreed to give my patients and community the best medical care I could with the personal and professional resources I have. Not just procedural or intellectual services, but compassion and care. “Cum Scientia Caritas”, serving my community with my head and my heart.
With hundreds of my colleagues, I’ve reflected on the millions of hours we have donated to keep the health system afloat over the years. Home visits. Deeply challenging consultations with people in mental health crises who have nowhere else to go. Calls on a Sunday from my patients who are dying, or suicidal, or just stressed beyond their capacity to cope. Setting up respiratory clinics and keeping up to date with the constant shifts in policy, process and evidence during COVID-19. Begging the hospital systems to accept my vulnerable patients. Policy contributions. Research. Teaching. Advocacy. Donating the gap between the Medicare rebate and the cost of care so the nurse in the clinic gets paid and the clinic stays open and the patient gets food on the table. All the unpaid overtime as an intern, resident and registrar.
I could go on. And on and on and on.
And yet the other side of the social contract, the professional respect, the financial support for our care and the granting of autonomy to practice to the best of my ability is slowly eroding away. In its place are compliance measures. Like most doctors, trained for 12+ years in complex care, GPs did not train to simply impose protocols on patients. We were trained to think. To evaluate the evidence, consider the patient’s context and point of view and then negotiate the best outcomes we can achieve with this patient at this time with the resources we have available. Evidence based medicine is the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.” Following a protocol is a vast underestimate of what you need me to do. The paradox of primary care tells us that forcing GPs to follow protocols reduces outcomes.
And yet the idea of “low value care” is often expressed in simplistic terms; take the evidence from studies examining one disease in a narrow population, and assume the outcomes apply to the patient in front of me. This was not what evidence-based medicine was meant to be, but it is how it is being applied. Which is why we have policies based on studies of patients who actually complete an intervention without considering the impact on the patients who drop out, or the people who never opted in. It’s bad science, poor policy and terrible medicine. But still, the rhetoric around low value care continues.
The relationship between general practice, the Commonwealth, and the community
There are so many parallels between what I feel as a GP serving the Commonwealth Government and other abusive dependent relationships. There are tactics – keeping us exhausted. Financial coercive control, which in our case leads 47% of GPs to underbill for fear of the PSR. Crazy-making contradictions in which we are lauded as “the cornerstone of the health system” and, in the same sentence, asked to shoulder more unpaid burdens of care. Dismissing concerns of GPs about patients safety as “turf war” arguments. Frank abuse in our clinics. And now public attacks on our professionalism and ethics. It is important to recognise that intent is not important here. It doesn’t matter what is intended when a perpetrator behaves this way. What matters is the perspective of the survivor.
Medicare has rorted me and my colleagues for years, especially female GPs. They have sucked me dry by cashing in on my empathy, relying on me to donate increasing bucketloads of compassion to plug the holes in the health system. The government knows most of us will do this in the service of our vulnerable patients, so it’s an easy characteristic to exploit.
Yet the “greedy, immoral doctor” narrative just won’t die. It’s too convenient for everyone, especially those who have a business model predicated on managing the “crisis”.
GPs are such convenient scapegoats, because everyone knows we will not turn our backs on our communities. We have been rorted for decades. There are thousands of us who hang on in a system that abuses our empathy – in aged care, mental health care, rural and remote, Aboriginal health.
We are not grubs. We are fools.
Policing “quality”
There is a revolving door of people who are convinced they could do my job. I still remember a close colleague attending one of my lectures on mental health care in general practice and saying with genuine surprise: “I had no idea there was any theory behind what you do”. Nobody really understands what we do, because if it were simple enough to explain in a sound bite, it wouldn’t need 12 years of training to achieve. We have also defunded attempts like BEACH which successfully quantified what we did for decades. However, the lack of relevant data on our activity or our outcomes doesn’t stop criticism from a variety of sources claiming we fail to do “it” well enough.
In the past 3 years there has been audit after audit after audit. There has been an increasing sense of threat from the Australian Health Practitioner Regulation Agency (AHPRA) and the Professional Service Review, including recent moves to publish our names publicly before a case has even been heard. We are all trying to protect our vulnerable young colleagues who are leaving in droves because they can’t cope with the public vitriol. Worse still, we are dealing with the suicidal doctors targeted by all and sundry who would rather drive off the road than go in the front door of their hospital. Dealing with the grief of their colleagues when they do die (and they do – here and here) is heartbreaking.
The result is an over-burdened workforce which feels constantly under attack. Defensive medicine is bad medicine. It is not good for the doctors, and it achieves poor outcomes for the patients. There must be a balance. Over-governance leads to poorer outcomes through defensive practice.
What is the impact on the GP workforce?
But let’s think strategically. There are lengthening waiting lists in general practice because the number of GPs in practice is plummeting. fewer GPs and more dispersed primary care? Isn’t that cheaper? And it it’s less effective, will anyone know? If we do accept role substitution as a solution to the GP shortage, what was all that training and sacrifice around meeting standards the community developed for general practice for? Why did we make the training and assessment so onerous?
In the UK, introducing multidisciplinary primary care teams did not seem to be effective in reducing hospital admissions, and the evidence for the efficacy of these teams is not clear. While there is no doubt nurses and allied health professionals bring invaluable skills into primary care, the evidence for the best use of multi-disciplinary skills in the Australian context is still evolving.
It may be cheaper in the short term to shrink the GP workforce. The ability to manage the patients no one else will see will drop, but I’m not sure anyone is measuring the metrics that will detect a change. Because trying to develop metrics for truly complex care is hard, and you need us to do it, and the investment in GP research has plummeted.
And I and my colleagues – who weren’t given personal protective equipment (PPE) early in the pandemic, who were told we weren’t frontline workers so we didn’t need vaccination early like hospital kitchen staff, but were frontline workers when we were needed to give vaccinations, who sourced our masks from patients with a sewing machine, who were vilified for protecting the immunosuppressed Granny in our waiting rooms by redirecting people with potential COVID-19 to the respiratory clinics we set up, who are being assaulted regularly in our clinics – we know we are expendable.
I’ve taught generations of doctors, written policy briefs, sat on committees, done GP research, worried myself sick about suicidal junior doctors, mostly unpaid, definitely undervalued. We used to attract 50% of the junior doctor workforce into general practice. Now it is 13%. We are expecting to be 11 000 full time GPs short by 2030. On any metric, this is a poor outcome.
Next steps
For decades I have defended my profession and my patients against policies that will disadvantage the most vulnerable. I have questioned policies that give more “consumer choice” for those with the literacy, health literacy and resources to access it, while reducing equity. I have taught professionalism, ethics and patient centred, value-based healthcare.
But none of us can endure persistent vitriol. It is easy to scapegoat doctors, and hang on to the idea that we are greedy, self-serving grubs. But the consequence is losing thousands of GPs from a shrinking workforce. Like many of my colleagues, I am just too bruised and battered to fight for my patients while I’m being accused of incompetence, callousness and fraud; to have my motives questioned; to challenge the narrative that I’m a greedy elitist with a hidden fortune fleecing the public for my own gain.
After 30 years of dedicated service, I no longer trust political assurances, or the expression of good will. The sad thing is that the system is behaving the way it was designed to do. Intentional or not, the demise of good general practice has been predictable for decades.
The question remaining is whether the community is happy to let it go.
Louise Stone is a GP with clinical, research, teaching and policy expertise in mental health. She is Associate Professor in the Social Foundations of Medicine group at the Australian National University Medical School, and works in youth health.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
From experience, General Practice is not what it used to be, not only in terms of being parasites who rort the system. All the old experienced, Australian trained GPs have retired and the new batch, even from the UK and Ireland, are poorly trained and make hair-raisingly wrong diagnosis.
I had one GP who not only made an alarmingly wrong diagnosis of a common eyelid infection but wrote in her referral to the specialist that I refused to take the antibiotics she prescribed. I could not understand why the specialist clinic did not contact me for over a year until I asked a replacement GP to show me the referral.
When I finally got to see the Eye Specialist in hospital he looked at her diagnosis and prescription and snorted that it was entirely wrong. No antibiotics should have been prescribed. Just one example among many.
In my view, the Govt should abolish the whole GP system, now reduced to writing referrals to specialists, and train a whole lot of specialists who have some depth of knowledge about the condition they are treating.
A letter to Dr Stone
Dear Dr. Stone
Reading your article at first I thought you are talking about the US system but regardless the issue is an international one. The logic for it is simple. Healthcare evolved based on addressing critical care. Critical care is not only expensive but with serious socio-economic consequences. The attack would be correct if it would be addressed on the industry rather than the one component that actually is a victim of the process. The primary care doctors. It is quite evident as we see their numbers rapidly diminishing and what is going to create a major worldwide problem.
But the reality is that the industry is ignoring these situations as evidenced by not only articles like the ones you are referring to but the actual facts in the industry illustrated by the shortage of primary care doctors and the entry of industry outsiders like retailers that is going to have even further negative influence on the delivery of care.
However, as I always say and as a former banker that specialized in bankruptcies and turnarounds the issue is not that there are no viable solutions available but rather that many in the industry look for a pedigree rather a solution.
We developed the only interactive preventive system to address these critical issues. Especially relevant in rural areas. No, it is not a simple video but a solution where a doctor with the use of a simple cellphone can interact and monitor a patient disease-specific and prevent critical and expensive consequences. The solution is especially relevant as it was developed in providing primary care doctors not only the ability to deliver better care to their patients but a new source of revenue to keep them interested to stay in business and especially to eliminate accusations like the article is implying.
However, to accomplish this we have to get beyond talking about and implementing. Over the years I tried to reach out to several of your colleagues in academia as well as the industry but besides a polite response, I never got past even after offering to implement it at cost to prove its value.
Sincerely
In addition to the excellent points Dr Stone makes about the current attack on general practice I would (have previously https://nordocs.org.au/56-hot/1218-all-change) added the change in the focus of government funded support organisations in primary care. The original Divisions of General Practice were supportive of general practice while the Primary Health Networks are antagonistic. This is a point made abundantly clear earlier this year by newly elected RACGP president Dr Nicole HIggins in relation to the North Queensland Pharmacy trials.
Everyone agrees the Australian version of primary care is doomed and it would seem beyond the capabilities of government from either side of the political divide to change that trajectory.
The debate for the future is over whether we follow a UK or a US style of primary medical care. Neither of these options is enticing.
David Guest
Goonellabah Medical Centre
Until last week GPs where “only” severely underpaid, overworked and overbearingly accountable for the ongoing well-being of their patients. Since Monday “Medicare cheater” was added to the job description.
It intrigues me the lack of understanding the author of the article displayed. Completely disregarding the devastating impact these loose accusations have in any medical graduate considering entering the profession and those contemplating earlier retirement.
When the number of new GPs growing only 2.8% vs 6% growth in the retiring group (2021 data from DoH) the bucket is leaking two times faster than is filling.
Before the publishing ”the article”, Deloitte estimated a 28% GP shortage by 2032. Surely the article will help bring this alarming number sooner.
If the intention of this political move was to help kill any desire to become a GP was certainly achieved. Perhaps the option is to let patients get sicker and go to ED, that’s a department working smoothly and has great capacity to deal with the overload…
GPs have been rorted. For decades, millions of phone calls, delivering medical advice, to nursing homes, and patients, has been delivered without charge, many times a day, with legal responsibility, but no remuneration.
Consider the following Census figure that 70% of negative gearing is held by the medical fraternity.
How many times are we invited by hospital staff to not refer to Surgical OPD or Gastroenteeology OPD but to refer to a named specialist so our patient can jump the list and the specialist bulkbill Medicare-essentially shifting the cost from State Government coffers to Medicare- has been very common in Queensland for 30 odd years ?
How many times do patients tell us that their ‘’ ‘ist’’ has told them to go to their GP to get a Management Plan done so the therapist can bill Medicare ?
State Government instrumentalities ripping off part of the 8 billion and therapists similarly if the GP agrees.
How many similar matters if we put our mind to it ?
Medical doctors are an easy target because we are very disunited and mostly to busy providing care to cogently respond to egregious accusations.
A sombre outlook for future health care. Egregious generalisations do not help either understanding the issues or finding the best solutions. I’m
Not sure why many professions are being targeted…. Greedy doctors, slack teachers, corrupt lawyers and politicians. These labels are counterproductive and lead to a general lack of respect in society and that won’t end well.
Yes. Evidence based medicine is tick box rubbish. Easy for bean counters to count. Which they then do poorly.
The study populations but we treat individuals. FACT.
Red tape and other such low value measures to induce beuralysis only bring worse outcomes for patients and doctors while some muppet somewhere in an office can sit with likeminded people congratulating each other on a job well done. It’s time they had a performance review (done out of hours for no overtime, of course) that really dissected what they actually DO.
Personally I think the media show was defamatory against all medical workers .
It is time such were held to account legally .
@David Skewes, utter nonsense. everyone I have spoken to from the UK says the NHS is a horrible, horrible health system to work in. Government deciding what is fair remuneration ? LOL !!
You have to ask why is the public so ready to believe those in the medical profession are rorters.
Perhaps the answer lies in the fact that all Australian adults at some time have been robbed by someone in the “profession”. $300 dollars for a 10min chat with a specialist. $9000 for an orthodontic treatment. $1000 to the anaesthetist so your child can receive dental treatment.
That awful feeling of being blackmailed does not subside easily.
A shame that G.P’ s, who are largely conscientious hard-working professionals, bear the ire created by the other white coated sociopaths.
This reallity is the same here in Brazil
It’s hard when even the people who like us don’t really think we do anything. I was bemoaning the change to rebates for ECG and how it suggests GPs can’t interpret them, and the practice manager and the 19 year old receptionist both agreed it was ridiculous, especially since they can read an ECG just as well as the GPs…
No one will know how much GPs do to learn and strive to care for other people. This is the invisible pillar of professional training. Doing the best with all the constraints.
The only way it will be missed is when it is no longer around being taken for granted.
Well said Associate Professor Stone. We GP’s all work with people who are/have been victims of family or partner violence. We see multiple patients who have been exposed to gaslighting, coerversive control, financial abuse, and experts at managing variable moods from a volatile, unpredictable partner.
Anyone else seeing the same pattern with GP’s and Medicare?
It’s even at the stage where I am hearing the victims (my fellow GP’s) say “I can’t leave, I have no where else to go” , or “I don’t have the money to leave”, “better the devil you know” and “maybe it will change” and “its not that bad yet” and “they promise they will improve” Think about it. It IS an abusive relationship.
The next steps are “I tried to leave but I kept getting pulled back” “I should have left then when X happened” Maybe in the near future we will hear “I have got the courage/means/ability/help/alternatives to leave” Then we will have the comments, “She should have left years ago, you could see how unhappy she was in that relationship”
We are all hoping that Jim Chalmers will finally raise the Medicare Rebate to an appropriate level in tonight’s budget but we GP’s know how to tell when a system is sick.
The best predictor of future behavior is past behavior. Don’t hold your breath.
Well the ABC has always been a mouthpiece for the ALP. “The crisis in general practice” reports (yeah, the crisis we predicted 40 years ago but nobody listened), then the AMA’s “solution” of capitation (thanks guys, you always did only care for the specialists who make ten times what we do) then the Doctors Rorting Medicare articles – all part of softening the voters up to the proposal of a NHS style system which will be the last nail in the coffin. Glad I’m at this end of my career and not starting out. Though as I become older and more vulnerable I’m not looking forward to being cared for by a pumped-up nurse who doesn’t know what s/he doesn’t know, nor an appallingly bad overseas trained but bulk billing doctor, nor a brutalized hospital system that fetishises keeping patients away. Yet another idea too awful to not be implemented.
Thankyou for such a clear yet heartbreaking article. I worked for many years as a district nurse in England and Australia and also in theatre and the wards. To suggest that a majority of doctors are rorting the system is rubbish and when I think of all the wonderful doctors I worked with in 40 years of nursing it makes me want to cry then swear.
This a great letter.
There is certainly some financial abuse occurring that involves Medicare billing but it would be nothing matching the claims in the 4 Corners report.
The report comes from the ABC which has a particular view and agenda.
The ABC and other sources need to provide hard evidence to support their claims and to identify which areas of the profession is responsibility. In the absence of any response this become nothing more than mud throwing.
John Armstrong
Respiratory & Sleep Physician (retired)
I am a retired Oncology Surgeon. Initial I was overjoyed when my eldest son raised with me that he was thinking of doing Medicine. However, as I thought more about how the treatment and appreciation of the medical community had deteriorated over the years and the appalling way we are treated by AHPRA I hated to think that I cold encourage my son to dive into that mess. After much discussion with him, including telling him how things had deteriorated over the years he decided to look elsewhere.
He still occasionally raises the matter of Medical School but I love him dearly and would hate to see him in the firing line that is constantly aimed at our profession.
Very well written article. Deserves to be seen in the mainstream media.
In 2021 my boss and I both retired from General Practice. Both of us were 60 years old. A lot of knowledge and experience walked out the door when we left. Both of us would have considered giving a few more years if we had felt supported and respected in our role. The current situation in General Practice is not only stopping young doctors from taking it up but is causing us older ones to leave prematurely. Ultimately the patients and the community are the losers.
General Practice, better termed Primary Care, is by far the most important tier of the Healthcare system. To put it bluntly, everyone needs a GP. It is the GP that identifies the need for us to see a specialist to refer us to the most relevant specialist and to implement the care plans recommended by that specialist. I have spent about half a century working in rural and remote centers, mainly in SA. There we see General Practice as it should be. The Practice cares for its people from the cradle to the grave. The country GP knows every patient as a townsperson, a whole person who has an identity and standing in that community. The doctor-patient relationship is continuous, not episodic. This cannot be achieved by a series of 15-minute consultations and a battery of investigations.
It is taken for granted that the GP will manage residents in their homes, in Residential Care, and in the local hospital with little financial recognition and recompense.
Metropolitan General Practice has degenerated to coming a managed business.
I became a Geriatrician in England in 1973. I spent a year in general practice to raise the money to take myself and my family to England. On arrival, it became obvious that living in London was very expensive and a senior Expat Australian doctor helped me to find locum work.
I was appalled by what passed for general practice in metropolitan London.. I discovered that my role was to write prescriptions and health certificates and send everybody else to A&E at the regional hospital. As a locum in A&E, I took histories, performed medical examinations, and arranged tests and investigations
When I became a Registrar in Canterbury I met the equivalent of the GPs that I had worked with and for in Adelaide. In England. What I see in Australia now, is very much like the disaster that I saw in London in 1973.
“One of the best healthcare systems in the world” is a mess. The Royal Commission into Aged Care Quality and Safety had very broad Terms of Reference to examine the whole of Healthcare of which Aged Care is a part and failed to do so.
I am now working on a critique of the RC. It will be interesting to find out who will be game to publish it
sa
Lock-stock-& barrel reform of the health system is required. The belief repeatedly stated that ‘Australia has the best system’ is a glib misrepresentation of the reality, which is one of chronic underfunding, leading to increasing costs to patients. It’s time the fee-for-service system was dismantled, and replaced by an appropriately funded NHS-style federally-funded system whereby doctors are employed by the State, with guaranteed five-yearly updates of terms & conditions, including remuneration in line with inflation and costs.
selective reporting and biased against good doctors (the vast majority)
How very true.
Very eloquently put.
Please please this needs to be published in the mainstream media.
How true. I cried reading it. Please please publish this in the mainstream media.
I am a specialist surgeon, but I sympathize very stongly with GPs and the statements expressed in this article. The lack of respect given to GPs by the government, the media and the public has degraded the fundamental component of patient care that is General Practice. The system has redefined doctors from highly intelligent and highly trained professionals to be low grade, subservient public servants. The time is fast coming when Doctors will revolt, divorce themselves from Medicare and bill patients directly. You can’t defraud a system if you don’t work in it. Patients will become aware of the costs. Patients may well choose for themselves what treatments they have.
Medicare defines its aim as “to provide basic health care”. This does not match with the care most GPs wish to provide. Caring is so much more than basic health care! (I do not know a single GP who is not intrinsically a caring altruist.)
I find it very hard to believe, has the research on this been peer reviewed and published?
Stop using medicare items
Bill the patients directly. (in advance) in 6 minute increments’ (as per lawyers).
Charge the same rate as plumbers for home visits.
Let the patients take their bill to the medicare office to claim a refund. Medicare can determine what the appropriate item number was. This shifts the “fraud” allegations and compliance burden to medicare and the patients (which is were they belong).
The patients who won’t or can’t pay can attend the public E.D.’s
If all GP’s did this for two weeks then your problems would disappear.
Makes me want to cry. As soon as the story broke, I immediately thought of all these self-sacrificing GPs who would be deeply wounded by the accusations raised, which mostly do not apply to them. This may well be the final nail on the coffin of many family general practices, as we heard a lot of the doctors are nearing retirement age; I fear they will all start closing their doors at once and we’ll all be worse off for it for years to come. (I’m a non-procedural medical specialist who charges a gap and who has always been practising with the principle of putting patient’s’ care above any self interest ).
There needs to be an expose of the corporatization of GP practices, private radiology services and large cardiology conglomerates – the latter are run by bureaucrats and accountants who impore their salaried specialists to overservice, run multiple tests that are without clinical benefit and this is pretty much all funded by the Medicare Golden Goose. We call this “Churning”…….The owners of these practices can’t get enough of it……..the tax payer is funding their profits and impressive company equity…….leave our GPs and non-corporatized specialists alone.
Medical practitioners are selected for their intelligence and honesty and then trained in the skills required to provide services to patients. Those who are unethical would normally have been found out by the profession and dealt with in a collegiate manner. Unfortunately things have changed.
Patient care and the responsibilities of the profession have been taken over by non-medical bureaucrats in a big way, particularly those with a vested interest in controlling the medical profession.
Non-medical (particularly governmental) bureaucrats should never be allowed to dictate the care of patients. It is an excellent time to re-evaluate the billing processes and return the responsibility of billing for services rendered back to the practitioners.
And while we’re at it, it would be an excellent time to consider returning the care of patients to the medical profession. The regulation of standards should be returned to the profession and not dictated by lawyers, administrators, and government bureaucrats.
Dear Louise,
you say it so eloquently. It is the constant undermining and using our ( free of course ) empathy and compassion at the same time. this article is not about fraud,rorting discussion – it summarises the emotional injuries over time , in which the undifferentiated broadcasting is only the icing on the cake. I am so passionate about my job – but now cant wait to get out – a very sad ending of my love for the profession. I wonder how many of the commentators are male and do not feel the emotional injuries ( I am NOT accusing all males of not being empathic and compassionate, just to forestall any complaints ) and hence comment on the discussion about rorting the system ? I do know that my female colleagues are burning out at speed of light after years and years of turning the other cheek. I sadly think that GP land as we know it is coming to an undignified slow and painful end.
All of us have observed evidence of Medicare fraud or at least gaming of the system to maximise billings. The extent of the problem is huge but individual GPs are u fortunately feeling like they are the scapegoats for public concern. As per the 7:30 Report, the real concerns are with these corporates running GP Practices and what is happening in Radiology corporates in particular is where there is real cause for concern.
The corporatisation of general practice has totally destroyed it. The profit motive is not a good driver in health. The same could be said about aged care where are our most vulnerable aren’t given enough to eat in the interests of profit. Nationalising medicine is not the answer either- look at NHS. Australia has a health system that is the envy of the world. Bulk billing should be reserved for those who are genuinely in financial hardships- everyone else should support a fraction of the ever increasing costs of medicine with a co-payment.
Its always been a delicate balance of trust and respect. GP’s go above and beyond because we are basically motivated by wanting to help patients , often at personal and economic costs. If you break that spell, and we feel we have a government who does not value us on behalf of the community, then you quickly find out how valuable the service was, and how much free service you were getting . Because GP’s are walking away. If COVID taught Government anything, they need the goodwill of General Practitioners. Build a fair and transparent system. then just get out of they way.
Lets turn to volume down on the media hype. Its simply mischievous.
A very well written overview of the current GP crisis .
From my perspective It is indeed disheartening that after 30 plus years of multigenerational patient care we can be treated with such disrespect with narrative of “Greedy doctors “
Indeed the profession has been heavily burdened during the last few years of the pandemic and many are tired and will consider earlier retirement or other options.
Negative media doesn’t help promote the profession to the
new graduates.
The article needs to be on general media for the public to read .
The bond between the doctor and patient is sacred. Currently in Australia that bond is fractured. When it’s broken, the system collapses.
The most recent episode of “File on 4” on the BBC includes a heart-breaking recording between ambulance services and an elderly man lying on the floor following a fall. He called repeatedly and no service came over many hours and in the end in great pain and with fortitude he was telling the operator that he would die, as he indeed did. Having observed family practice over six decades, I consider it very improbable that this egregious failure of care would have happened before government policies and regulation led to the profound decline in access to general practice. Sadly we are following the UK over the cliff.
Congratulations Dr Stone on putting perspective in this matter. Unfortunately the ABC, strident voice of the extreme left wing, will have neither the courage nor political honesty to make a programme that gives such perspective. The shortage of GPs cannot be solved by importing doctors from low and middle income countries seeking a better life (those countries need them even more than we do) but by addressing the problems so well set out in the article.
There are no doubt some are rorting the system which is set up for it without the patient’s’ contribution. The most egregious examples touted in the media damage us all. Amalgamating professional misconduct, honest errors in a complex system and “low value service “ is inappropriate. The majority who try to do the right thing by their patients and the system burn out or go broke because of underfunding. Very depressing.
This is a defensive article
No one claims $8 billion is being rorted – that figure includes waste and inappropriate claims, as well as outright fraud.
In my wide-ranging career I have glimpsed the latter and been tempted myself. I am an honest person, but opportunities are rife, and the risk of detection almost non-existent. If my experience is typical, then if not widespread, fraud is still very common. Surely I am not the only one….
Moving to the UK style capitation payment will be cheaper for the government and disastrous for the care of the vulnerable. This campaign is a preliminary probing in the process to move away from fee for service. Patients will be the ones who suffer.