THERE is no sound ethical argument why health care professionals should not vaccinate children aged 12 years and over who want protection against COVID-19, even if their parents do not consent to the procedure, according to two of Australia’s leading medical ethicists.
Professor John Massie, Professor of Paediatrics at the University of Melbourne and a leading child bioethicist, told InSight+ in an exclusive podcast that at the heart of the issue was the capacity of the child to make a decision in their own interest.
“We assume adults have capacity to make decisions that are in their own interests,” he said. “And we then have to work hard to prove they don’t if they’re making a bad decision for themselves.
“In children, it’s flipped – we assume that children don’t have capacity to make decisions for themselves.
“Most people would think that 16-year-olds can make most decisions for themselves, and then under 16, for virtually anything, children would need the consent of a parent to undertake a procedure.”
The underlying ethical principle that should guide vaccine providers when assessing the child’s capacity was the “mature minor doctrine”, Professor Massie said.
“The mature minor is a doctrine that is situated in the context of the procedure, or intervention that’s being proposed. There’s going to be a range of things that a young person might decide for themselves.
“If they have the capacity to understand the nature of the illness, for example, and the procedure and the side effects and the risks, then they should be able to give consent for that to happen.”
The key was for the vaccine provider to assess each child’s ability to do that on an individual basis.
“It is clear that the onus is on the provider to assess the capacity and record that.”
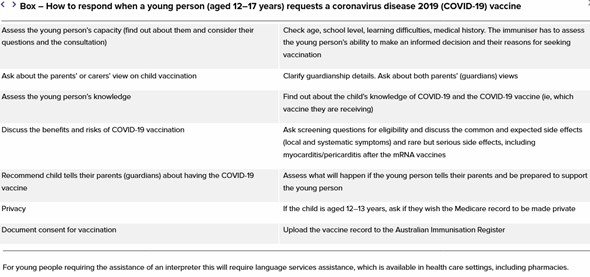
In a Perspective for the MJA, Professor Massie and his coauthors provide a table of the sort of things a clinician might want to consider when assessing a young person who requests a COVID-19 vaccine.
Professor Paul Komesaroff, Professor of Medicine at Monash University and Executive Director of NGO Global Reconciliation, told InSight+ the concept of vaccinating a child against their parents’ wishes was “uncontroversial” and “nothing new”.
“[The mature minor doctrine] is a principle that involves judgment in individual cases,” he said.
“The choice, certainly in [judging] Gillick competence, comes down to the medical practitioner making an assessment of the child on the basis of that privileged relationship that a health professional has with the young person.
“[Massie and colleagues] propose a set of very prudent and, I would expect, practically helpful guidelines for clinicians in all contexts.
“They have been at pains not to state an extreme, exaggerated, or even unfamiliar position. They make links with the existing legal and ethical structures in order to establish the principle that vaccination of young people 12 years and older satisfies the same principles that other forms of medical treatment have.”
Despite the ethics of vaccinating children against their parents’ wishes being clear, the legal protections for vaccine providers in a situation where the parents may object remain “very messy”, according to Professor Massie.
“The Australian Immunisation Handbook says that there are various state rules, but if it’s unclear, the vaccine provider should rely on mature minor doctrine,” he said.
“In some states, like Queensland and Victoria, it’s clear that the 12- to 15-year-old group should be able to get vaccinated under their own steam.
“In South Australia, Western Australia and New South Wales, you need a parent’s consent, but in NSW it’s messy depending on who you ask.”
Professor Massie said it was not the vaccine provider’s role to be “adversarial” with parents.
“We’re trying to preserve parental involvement in the care and treatment decisions – after all parents are the natural decision makers for their kids,” he told InSight+.
“But they don’t have absolute authority or absolute sovereignty over their kids. They’re limited in their decision making by their own capacity to make a decision, which ideally is in their child’s best interest, or at least not harmful to the interests of their kids.
“The emerging autonomy of the child then needs to be taken into account.
“You could build a case here that says the child is deciding for themselves that value judgment about whether vaccines are good.
“So the weighting falls to the kid who has capacity to make that decision.”
In another article published online first at the MJA, authors from the Murdoch Children’s Research Institute and the University of Melbourne have detailed the potential indirect impacts of the COVID‐19 pandemic on children.
“We identified 11 impact areas, under three broad categories,” the authors, led by Professor Sharon Goldfeld, wrote.
Child-level factors:
- Poorer mental health
- Poorer child health and development
- Poorer academic achievement
Family-level factors:
- Poorer parent mental health
- Reduced family income and job losses
- Increased household stress
- Increased abuse and neglect
- Poorer maternal and newborn health.
Service-level factors:
- School closures
- Reduced access to health care
- Increased use of technology for learning, connection and health care
Goldfeld and colleagues proposed five “potential strategy areas” for policymakers to consider:
- Addressing financial instability through parent financial supplements
- Expanding the role of schools to address learning gaps and wellbeing
- Rethinking health care delivery to address reduced access
- Focusing on prevention and early intervention for mental health
- Using digital solutions to address inequitable service delivery
“History shows us that children already experiencing adversity lose out the most, with the potential for widening health inequities,” Goldfeld and colleagues concluded. “Now is the time to not only repair the past, but to start to re-imagine the future for a more equitable Australia for children.”

 more_vert
more_vert
I’m not surprised that 86% of people strongly disagree to this. How come all norms doesn’t apply anymore when it comes to COVID 19. I think this article should have been made to cover general vaccination but specifying COVID 19 has made it seem unpopular. I’m afraid very soon kids will ride over their parents and it will be acceptable if they have been vaccinated. Taking away all parents rights over their children is could be dangerous, We are helping to push more kids on the streets.
This is a hard, but not a new one. Confronted by a parent refusing any vax for an infant they own, I have had the urge to seize and jab, but never the courage. When one parent, after a relationship split has fronted with an 8 y.o requesting vaccination thereof, I have acquiesced, after first considering the personalities of those involved (not being the bravest). Consider: There is no age where we suddenly are mature enough for independence from our long term “owners”. Society allows this ownership, trusting parents to make good decisions for their off-springs, a trust that is often challenged by kids, especially teens.
Death rate from covid in this case is real but small. Death rate from vaccination is real but I hope, smaller, but this won’t help if it is your kid or your patient on the death bed.
Can there be an answer of Y or N? Not ethically as the parents have a right and can we deny the 12 yo the right of immune protection? Legally, likewise as court cases often depend on performance of the many players and appeals often win.
Post my comment – 77% disagree – I had interpreted as 77% agree.
Peter Strider makes a great point in the comments.
A fascinating and complex area of bio ethics I’m actually very surprised at such a one-way vote on such a complex proposal.
I think extreme care needs to be taken in this decision. Whether or not a doctor may feel a sense of doing the “right” thing because “they” feel it is right may be sorely tested should a moderate/severe adverse reaction occur (myocarditis – to others more severe) – how could one confront the parents in that potential (albeit unlikely) situation? It’s a big responsibility for a non-parent to replace a parental role and take on with a 12-16yo.
But most concerning would be the legal extrapolation of that precedent – in a time when there is a campaign to increase the legal culpable age of criminality in children to reduce their imprisonment – this would not be helpful. Saying on one hand they are old enough to make a medical decision for themselves would make it very hard to argue the opposite ie that children on the border age of 12-16yo are too young/immature to have full insight (and therefore do not culpable, criminal responsibility) to be imprisoned for their actions.
Cosmetic surgery – esp for girls this age – would be another dire ethical area should it be “decided” that 12-16yos can decide to have cosmetic surgery without parental consent… any surgery for that matter but cosmetic surgery likely being the most sort after by vulnerable teens.
So while for many I can see it may seem to be a righteous and “good” thing to do but the complexity, legal extrapolations, and unintended outcomes of that could have very undesirable unintended costs. One would have to measure the cost and benefits which is pretty easy for a 65yo with heart disease and diabetes but for an average healthy 15yo girl – let’s just say the formula would give different results for diff cohorts and take much more time than I have.
Oh dear. The majority of anonymous posters obviously cannot read.
The title of the article has the hint “You can vaccinate……..”
Not you have to. Or even You should.
Exactly like you can initiate a blood transfusion or cancer treatment. (Both far riskier than vaccination).
Be a doctor. Make a judgement call. Oh and to the poster conflating sexual consent to vaccine consent, you should google age of consent in the Northern Territory and not rely on puritanical moral judgement from hypocritical Americans.
Disagree strongly. This is a disgrace that you would even suggest vaccinating children without parental consent. ?
Thank you Ken Parker for bringing some sense into this discussion.
We do know that these young individuals have a diminished capability of seeing the consequences of actions and decisions due to the prefrontal cortex situation in these age groups.
Also let’s remember that the ability to make good sensible decisions is a matter of training and practice as much as individual personality traits.
Peer influence does also influence greatly especially in those undergoing (or about to undergo) the hormonal influences of teen years.
I am not saying that there are no individuals in this age group who are able to think well for themselves, quite the contrary, however, only a parent will know their developing individual teen or preteen well enough to know which ones do consistently.
As a consequence of this pandemic, I no longer trust “experts”.
So many great responses, yes another example of overreach. When we no longer have politicians dictating our professional decision making (and using coercive behaviours to do so) and health care workers / peak bodies pretending to be politicians, only then can we start having rational diacussions on ethics.
Suffice to say you are crossing into dangerous territory by taking away parents rights to make decisions for their children. (Copied)
And whi will look after these children if they suffer adverse reactions!
A 12 year old is 5 years younger than the smiling teenager with her arm around a smiling Prince Andrew, yet she is now suing him for lack of consent, a couple of decades later.
While I am resolutely pro-vax, and all my children were fully immunised including the optional extras like Meningococcal B, I am also pro-consent. A 12 year old cannot consent to anything, neither surgery nor drug treatment nor sexual intercourse. Parental/guardian consent (or a court order, as in transfusion of Jehovah’s Witness children) is required even for essential medical treatment.
The disease is extremely mild in most children, so the vaccine confers minimal benefit to the child recipient. Vaccinating the child as a human shield for unvaccinated adult contacts is ethically dubious. Likely non-family contacts like GPs, dentists, teachers, and in some states, transport and retail workers, have 100% vaccination rates. It is hard to imagine an informed consent process which adequately covers the risks of myocarditis and the risks of domestic violence against the child when the parents find out.
Phrases like “mature minor” and “emerging autonomy” have some role in the legal grey area of 14-16 year olds, in areas of significant benefit to the patient, such as contraception. But the potential vaccine benefit to the 12 year old patient is negligible (ask former Qld CHO Dr Young) – it’s not like marrying a prince.
This is not acceptable
To take away the rights of mature children to receive vaccination even if the parents disagree is tantamount to a prison state. We saw how that worked in Nazi Germany when individuals lost their rights to live a free, lifestyle without any rights to exist. The State can remove children from their parents if the standard of care as set out by the State Health Authorities falls below a certain standard. Children in exceptional circumstances have the right to divorce themselves from their parents and under age marriages are allowed so why can’t mature children request and receive the vaccine which could save their life. Those anonymous replies to this vexed issue are merely quoting the accepted standard as laid down by APHRA. We followed the teachings of Galen for 1500 years before the age of enlightenment. If we don’t go forward, we go backward.
You Call that Ethical!! I Strongly Disagree.
It has been some years since I practised medicine as an anaesthetist. I have been a firm believer that to combat this COVID SARS pandemic, isolation of the affected individuals is essential and complete vaccination of everyone likely to come into contact with the virus which I think we all agree is airborne and for this very reason, masks are totally ineffective in preventing anyone who breathes air from getting the virus. I think that doctors often under estimate the intelligence of teenagers and upon explanation of the pros and cons should be able to give consent to be vaccinated.
Interestingly, we are not setting any precedents here. For many years the child of a Jehovah’s Witness could be given a blood transfusion even if the parents have forbidden it. What is so different in this case?
Beyond comprehension that any decent, rational, educated human being could think it’s ok to vaccinate children when parents don’t consent.
I strongly disagree that children are capable of making a sound and informed decision at that young age.
I disagree with vaccinating children without parental consent, children will not research but will go along with peer pressures to socialise with out considering future health problems…
Gillick competence in a healthcare setting + doctor is one thing, but there are additional issues when the child is getting the vaccine *in school*, where the parent-school and student-school relationship is quite different (no Gillick framework, in an environment ripe for coercion, peer pressure, etc.).
Strongly disagree as a child of that age is not able to make real medical decisions as they are not able to do and understand the reasearch that is required to make such an informed decision.
I am heartened to see that 77% of poll respondents (at the time I accessed the article) disagree. There is some hope for the profession.
Just another example of the state eroding parents rights. Who will look after this child should they suffer an adverse event? The parents!
When we no longer have politicians dictating our professional decision making (and using coercive behaviours to do so) and health care workers / peak bodies pretending to be politicians, only then can we start having rational diacussions on ethics.
Suffice to say you are crossing into dangerous territory by taking away parents rights to make decisions for their children.
Does this logic mean we also can’t vaccinate a child against their wishes even when the parents wish it?
I know quite a few rebellious teens who like to take risks – smoking, drinking, drugs and the like. Vax refusal seems another great way to upset their parents and gain peer cred as really radical!
The suggestion that we can do things to minors without parental consent is nothing but a destruction of family. It is reasonable, as a child matures, to want his or her consent as well as the parents’ but no matter how persuasive the argument, eg for immunisation, it sets a precedent for the state taking authority over their own children away from parents. I am surprised and appalled that ethics leaders of our profession should take this stand. This is already happening in educational institutions overseas if not here. It’s more than disappointing that our profession should be aligning itself with this concept.
My biggest concern about vaccinating children without parental consent is that in my experience, where parents and children disagree, the kids want to be vaccinated for social reasons and are completely unaware or uninterested in the medical side of the decision. Whilst vaccinating adults has a comfortable cost risk ratio, it is definitely not as secure with children
Thank you Cate Swannell for your insight into how medical ethicists think.
Thankfully we live in a world where legalities merely define boundaries of appropriate behaviour rather than dictate it.
Equally, we live with the knowledge that from 12 years we prune our neurology with diminished prefrontal cortex capability and a distinct tendency to escalate risk taking behaviour within a shift from a family oriented axis to peer group.
Given the forgotten imperative to facilitate protection of the vulnerable with vaccines that various government adverse event registers document alarming concerns in those age groups mildly effected by covid.
Further, apply consideration of the practicalities of consulting a consistently familiar GP within an AHPRA rather than Hippocratic regulated framework.
Within an overarching ‘state of emergency’ enabling the continued use of substances merely provisionally approved with selective collection of response data.
Moreover, with politicians bent on looking good in the face of looming elections and appointed bureaucrats making decisions secretly in something called ‘national cabinet’.
Oh, and dare I mention multinationals satisfying shareholders in the light of losses from previous fines.
Perhaps the broader ethical issues would bear examination?