A CARDIOVASCULAR disease risk assessment tool that is not currently covered by the Australian Medical Benefits Schedule could be used to identify a “considerable number” of people who could benefit from statin treatment as primary prevention.
Coronary artery calcium is a sensitive marker of subclinical coronary atherosclerosis, and calcium scoring is an accepted re-classification tool when assessing risk in middle-aged people, according to the authors of research published in the MJA, led by Professor Thomas Marwick, Director of the Baker Heart and Diabetes Institute.
“A zero calcium score indicates that the risk of cardiovascular disease is lower than 0.5% per year, while the risk reduction achieved by statin therapy in asymptomatic people with calcium scores of 100 or more is similar to the benefit of statins prescribed as secondary prevention,” Marwick and colleagues wrote.
Fewer than 30% of people in Australia at high risk of a primary cardiovascular event receive guideline-recommended statin therapy.
“The National Vascular Disease Prevention Alliance (NVDPA) guidelines for managing absolute cardiovascular disease risk were most recently updated in 2012, and they differ in important details from overseas guidelines,” Marwick and colleagues wrote.
“Firstly, the Australian absolute cardiovascular disease risk (ACVDR) calculator, used to select patients for primary prevention statin therapy, is a locally calibrated version of the Framingham risk equation, which has been superseded in the United States by the pooled cohort equation.
“Secondly, the definition of intermediate risk, the threshold for considering statin therapy, is lower in US guidelines (10-year risk, 7.5% – < 20%) than in Australian guidelines (5-year risk, 10–15%).
“Further, the Australian guidelines do not mention computed tomography … coronary artery calcium scoring. US guidelines include calcium scoring as a decision aid, recommending statin therapy for people over 55 with non-zero calcium scores and for anybody with scores of 100 or more; they recommend not initiating statins for people with zero calcium scores.”
Marwick and colleagues analysed data from the Coronary Artery calcium score: Use to Guide management of Hereditary Coronary Artery Disease (CAUGHT-CAD) trial (ACTRN 12614001294640), a randomised controlled trial assessing the utility of coronary artery calcium scoring for guiding risk evaluation and primary prevention statin therapy in patients with family histories of early onset coronary artery disease (CAD).
“We have identified two problems with the assessment of cardiovascular disease risk according to Australian guidelines,” Marwick and colleagues found.
“First, the statin treatment threshold (5-year risk of 10%) is higher than overseas and excludes many patients with both family histories of early onset CAD and subclinical atherosclerosis.
“Second, all the cardiovascular risk tools examined were moderately sensitive for identifying people with coronary artery calcium, but the [Australian absolute cardiovascular disease risk (ACVDR)] calculator was among the least sensitive in this regard.
“As cardiovascular event rates for people with family histories of early onset CAD and coronary calcification exceed those associated with US guideline-defined intermediate risk thresholds, our findings suggest that Australian patients are undertreated by international standards. However, the ACVDR identifies people with coronary artery calcium poorly, so that lowering the treatment threshold alone would lead to unnecessary treatment for a considerable number of patients.
“Our data support the Cardiac Society of Australia and New Zealand position statement that calcium scores are most helpful in patients at intermediate 10-year risk (10–20%).
“We propose a 5-year ACVDR risk of 5% as a suitable threshold for coronary artery calcium scoring for patients with family histories of early onset CAD.
“Risk estimation is central to primary prevention of cardiovascular disease. Australian guidelines for statin therapy minimise overtreatment, but can also lead to not treating patients with family histories of early onset CAD,” Marwick and colleagues concluded.
“Because the prediction and management of coronary risk (rather than other events) is the main driver of clinical decision making in familial CAD … calcium scoring may personalise the application of the ACVDR calculator [to this large and heterogenous group of patients].
“Coronary artery calcium scores could be used to re-classify risk in one-half of our sample, and could change decisions about statin treatment in 41%.”The authors stated that “further outcome studies will be needed before changes to risk assessment and statin treatment thresholds in Australia can be recommended”.
Also online today at the MJA
Systematic review: Recruiting and retaining general practitioners in rural practice: systematic review and meta-analysis of rural pipeline effects
Ogden et al; doi: 10.5694/mja2.50697 … OPEN ACCESS permanently
Research letter: Improving communication with Aboriginal hospital inpatients: a quasi-experimental interventional study
Communicate Study Group; doi: 10.5694/mja2.50700 … OPEN ACCESS permanently
Podcast: Adjunct Professor Annabelle Farnsworth, Medical Director of Douglass Hanly Moir Pathology, winner of the 2019 MJA/MDA National Prize for Excellence in Medical Research … OPEN ACCESS permanently
Podcast: Professor Tom Marwick and Dr Prasanna Venkataraman from the Baker Heart and Diabetes Institute … OPEN ACCESS permanently

 more_vert
more_vert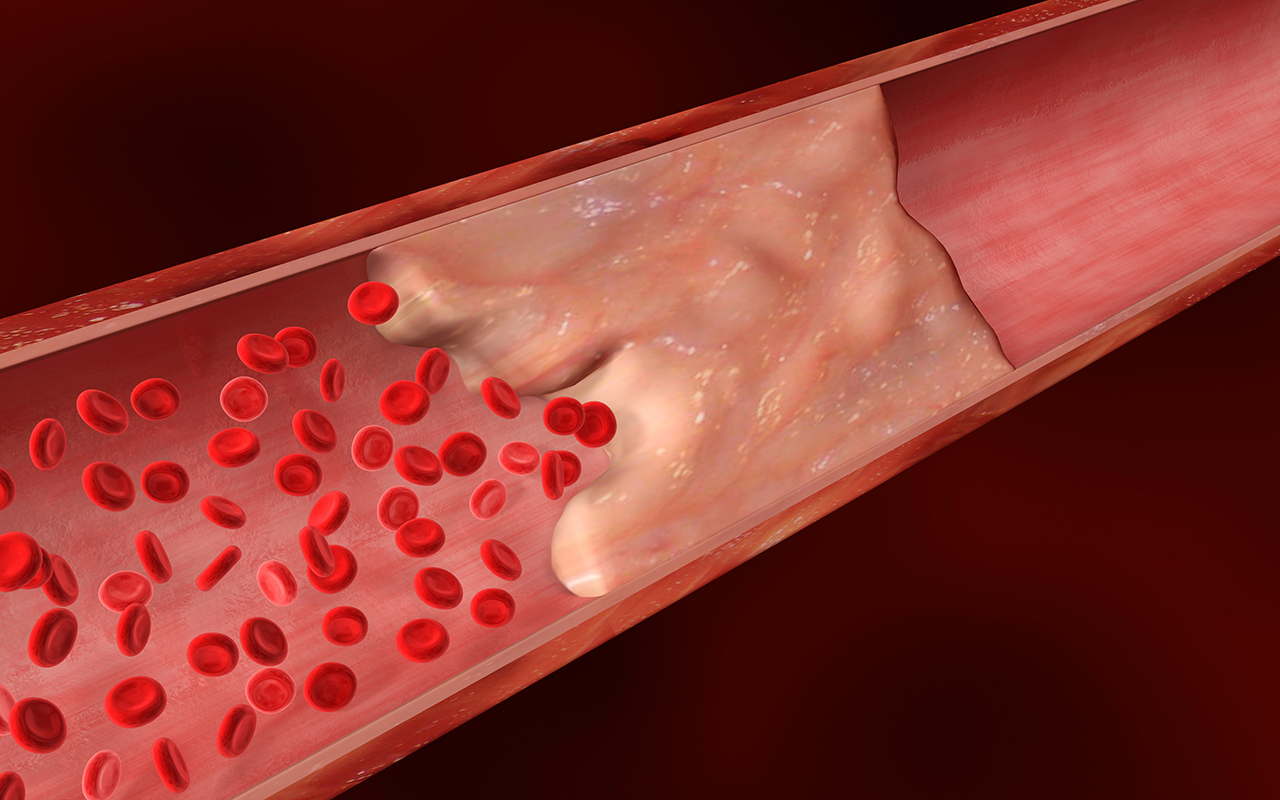
I am in early 60s with some family history of heart disease and three brothers who have had stents inserted or open heart surgery. around 12 months ago had a stress test (tread mill) with exemplary results. Then had a CR test done with a score of mid 700s. I am taking rasuvastatin and aspirin daily now. My LDL score is going down. I walk mist days but am otherwise not overly active. Have gained weight and recently experience episodes of breathlessness. Should I ask my doctor to consider a different statin?
I have been offering CTCA / CCS to patients in their 50s and 60s with either a family history, or risky lipid profiles as a decision making aid with regard to statins. I have been surprised at the number of zero or near-zero scores that have come out. In fact very few have come out with a score that encourages statin use.
Really the case ought to be made that the cost of the test is insignificant compared to the cost of 30 years or more of unecessary statin treatment that these patients would have undoubtedly received.
I am 55 & began having chest pain/discomfort so went to my cardiologist & he gave me a script for a quick CT calcium scoring scan. Score was 364! Of the 4 main cardiac arteries…3 scored 0 and 1 scored 364. My cardiologist immediately increased my Atorvastatin from a 10mg daily to an 80mg daily and also added a chewable 81mg aspirin. I also take Metoprolol Tartrate 25mg twice daily to control blood pressure. I do not regret getting the quick CT calcium scan (paid $75.00) & hope to one day see it offered as a preventative test to those who want it. Very important to know those numbers!!
I had a coronary artery calcium scan nearly two years ago, and had a score of around 160. My father died of heart disease at 49. I had eaten a lowish fat diet for many years.
I was at the time of the test aged 68 and weighed 140kgs. I went keto and there were a few keto sites that promoted the cac test, and so I paid for the test. I have been keto now for over two years and am now 112kg. I have switched to a high saturated fat version of keto. My blood results are the best that I have ever had, Im not even qualified to be prescibed statins. My doctor tells me ” Im dying of good health “!! I plan to have another cac test at the end of this year, as there are strong indicators that the score can be stopped increasing or reversed by diet alone.
My research shows that for my age the cac was actually fine, but nether the less, I would prefer it to be lower.
( I was a person who took part in the original statin trials, and suffered servere side effects, the testing lab instructed me to stop taking them )
Totally agree. I recently had a Coronary calcium scan arranged by my GP after I had an angiogram and scans and ultrasounds after a heart attack. I am 62 consider myself to be fit and healthy, eat well, always exercising with no underlying other health issues, ie.e diabetes, high blood pressure etc.
my scan score was very high showing I had a blocked artery and am now on statins.
No rebate for the cost of this test, and had it been done before the angiogram (which showed inconclusive), I wouldn’t have had to go through all the other tests and a 5 day hospital stay waiting for the angiogram.
My doctor agrees that everyone over 50 should have this test every year, there probably wouldn’t be so many people having heart attacks if this can be prevented.
Attention to WHY calcium builds up in the first place. Eg. High protein diets can displace calcium.
I have been delighted to STOP statins in a number of my healthy patients with abnormal lipids but a ZERO calcium score. CT angiography is not justified in asymptomatic patients with Calcium score <100.
Questions:
1. If every Australian with a 5 year CV risk of 5-15% receive a CT calcium score, then how many people will be scanned each year? What is the estimated number of malignancies that are likely to be caused from exposure to radiation?
2. Does the cardiac society have a plan for ensuring that people living in regional, rural and remote areas, including Aboriginal and Torres Strait Islander peoples, have equal access to this technology? Do we as doctors have a duty to ensure that new medical technologies do not widen the gap between the ‘haves’ and the ‘have nots’?
3. By lowering the threshold for starting statins and aspirin for primary prevention, we are going to substantially increase the number of people taking life-long medications. What proportion of patients over the age of 40, 50, or 60 will now qualify for these medications?
4. Do we want to use the US as the benchmark for best care? According to the Commonwealth Fund, the US spends more proportion of their GPD in their health care than any other country – nearly twice that of an average OECD country, yet has the lowest life expectancy; they also have the highest chronic disease burden. The Commonwealth Fund also notes that Americans use expensive technologies such as MRIs and other specialised procedures much more than our peers. It is clear from the US example that the widespread use of technology and the level of excellence of care provided to individual patients (especially in well funded academic health centres affiliated with prestigious universities) do not correlate with good outcomes.
Just to be clear, I am neither for or against coronary calcium scoring – I think that this issue requires careful thinking and debate especially from a population health perspective.
If you are going to perform a CT scan why do you not make it a CT coronary angiogram. A significant number of people with a calcium score of < 100 do have minor plaque which puts them at risk and surely this group of people also requires statin therapy.
It will also very likely cut down the significant number of unnecessary invasive coronary angiograms currently being performed. The only consideration to be made is whether they have an allergy to contrast. This test should be eligible for Medicare rebate if ordered by a GP.