Urgent action is required to address the systemic barriers deterring access to eye health care in Australia, write Dr Gifar Hassan and Clinical Professor Leanne Rowe AM.
For many years, the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) and other eye health organisations have highlighted the massive scale of preventable blindness in Australia, including increasing diabetic retinopathy, glaucoma, cataracts, macular degeneration, and uncorrected refractive error.
After three years of reduced patient access to preventive eye care and elective eye surgery due to the coronavirus disease 2019 (COVID-19) pandemic, medical practitioners at the front line of health care are increasingly recognising the dire impact of undiagnosed and untreated visual impairment.
This includes falls, motor vehicle and other accidents and injuries, medication error, deterioration of other comorbid disorders due to inactivity, mental health problems, loss of independence and prolonged hospitalisation to name a few.
Based on what is known about the increasing prevalence of diabetes and diabetic retinopathy, cataracts, glaucoma and macular degeneration in our aging population, it is likely millions of Australians are missing out on routine eye screening, follow-up and treatment, particularly in regional and rural areas.
As many disadvantaged people continue to have inadequate access to health care as we emerge from the COVID-19 pandemic, it is also impossible to estimate the true extent of undiagnosed eye disease in vulnerable groups, including Aboriginal and Torres Strait Islander peoples, ethnic minorities, and those with lower incomes.

Current workforce
The current eye health care workforce is not equipped to address the massive scale of undiagnosed and established eye disease.
There are only about 1000 full-time equivalent ophthalmologists in Australia, and only 13% of specialist ophthalmology care occurs in the public sector.
There are only 174 ophthalmology trainees spread across the five years of the program.
About 4800 full-time optometrists work mainly in private eye clinics in Australia, but the cost of retinal imaging deters patient access, and, as with all health professionals, there are increasing workforce shortages in rural and regional areas.
Practitioners under pressure
Eye specialists have long considered how best to increase routine eye examinations in patients at risk of blindness by general and other practitioners.
Unfortunately, the acute chronic clinical workforce shortage is putting many practitioners under extreme pressure at a time of increasing patient morbidity and mortality related to the neglect of many non-COVID-19 conditions during the pandemic.
Eye health is only one of a large list of priorities, including cardiovascular disease, stroke, diabetes, renal disease and cancer – all of which may predispose patients to impaired vision.
Asking practitioners to do more and more with less and less in this situation is fraught, particularly at a time when many are reducing bulk billing due to the lack of private practice viability.
For all these reasons, the uptake of Medicare incentives (12325 and 12326) for retinal screening by medical practitioners other than an optometrists or ophthalmologists has been poor across Australia, with only 1730 services claimed between July 2021 and June 2022.
Our first-hand experience
At the front line of rural hospital medicine and general practice, we are currently confronting all these barriers firsthand as we attempt to establish an eye health pilot to help upskill general practitioners in rural areas with acute health workforce shortages and disadvantaged populations with poor access to primary care eye screening and specialist services.
In this environment, it is challenging to overcome the systemic barriers in primary care for the following reasons:
- Medicare funding for eye health screening is restricted. The criteria for claiming Medicare items 12325 and 12326 are limited to “the medical practitioner (other than an optometrist or ophthalmologist) providing the primary glycaemic management of the patient’s diabetes … and the patient does not have i) an existing diagnosis of diabetic retinopathy; or ii) visual acuity of less than 6/12 in either eye; or iii) a difference of more than 2 lines of vision between the 2 eyes at the time of presentation”.
- There is also no source of funding for upskilling in eye health and retinal imaging, or to set up the necessary patient recall systems, access previous screening to detect deterioration in retinal conditions, integrate eye care with care of other comorbid disorders or purchase expensive retinal cameras.
- If eye health checks including retinal screening are successfully implemented, there are limited options for referral of patients with diabetic retinopathy, cataracts, macular degeneration and glaucoma to specialist care in the public system due to the severe shortage of ophthalmologists.
Recent studies have suggested these barriers are Australia-wide.
What are the solutions?
We believe there needs to be a whole-of-government approach to reform the health system and to boost the ophthalmologist, optometrist, GP and other primary care workforces, which will take time.
However, the severe workforce shortage and the massive scale of preventable blindness in vulnerable groups and in those living in rural and remote areas are so acute, urgent action is required to address the systemic funding and other barriers (listed above) deterring access to eye health care — a fundamental human right.
Ophthalmologists in the RANZCO Vision 2030 and Beyond, have built a powerful case for equitable, comprehensive and affordable screening and treatment for common causes of preventable blindness.
The Vision outlines practical ways to improve collaborative service delivery and preventive eye health care, workforce maldistribution, training, sustainability and a comprehensive approach to addressing inequity in eye health in Aboriginal and Torres Strait Islander peoples.
Importantly, RANZCO recommends “the Commonwealth work with the Australian Indigenous Doctors’ Association (AIDA), the Coalition of Peaks, National Aboriginal Community Controlled Health Organisation (NACCHO), the jurisdictions, the Colleges, and other stakeholders to develop special measures that facilitate access to healthcare services (not just ophthalmology) for Aboriginal and Torres Strait Islander peoples”.
There is a compelling case for other medical colleges, including GP colleges, to support RANZCO in their vision and to include eye health in any submissions to the May federal Budget 2023–24 to make “the right to sight” in disadvantaged communities a reality.
In the meantime, as a rural hospital medical officer and GP, we are determined to partner with others to overcome the systemic funding and other barriers deterring basic eye screening in rural and remote primary care.
We also determined to assist patients with heightened risk of eye disease, such as Aboriginal and Torres Strait Islander peoples and those with diabetes, access basic primary and tertiary eye care.
Overcoming the limitations in Medicare and other funding, engagement with existing services to build sustainable rural models and adoption of new technologies including artificial intelligence are the keys to overcoming the barriers.
The status quo is not acceptable. It’s time to overcome our medical and other silos because our whole health system is under extreme pressure. The only way to tackle the massive scale of preventable blindness is with united advocacy and a groundswell of community action.
Dr Gifar Hassan is a hospital medical officer, having recently worked in metropolitan Melbourne at Austin Health and Peninsula Health, and the rural Murrindindi Shire. She also has a Master of Public Health and a Biomedical Science Degree.
Clinical Professor Leanne Rowe AM is a rural GP, co-author of Every doctor and past Chairman of the Royal Australian College of General Practitioners and Deputy Chancellor of Monash University.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert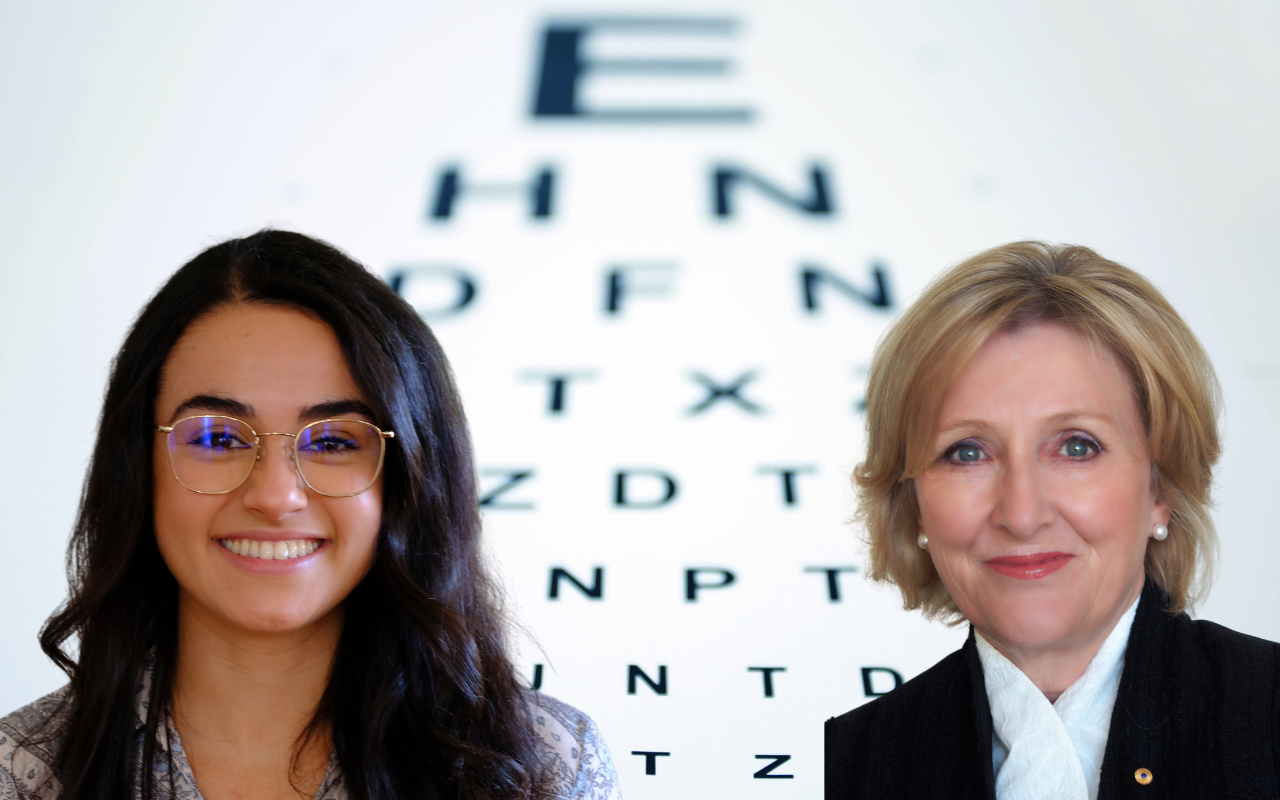
I support the increased use of optometrists in eye health screening. Here we have a reliable and widespread group of health professionals who are likely to be able to afford the capital cost of equipment, and have sufficiently educated staff used to looking in peoples eyes to perform more complex eye screening tests than most GPs. As an occupational physician practicing in a MMM7 area, I perform health screening on workplace candidates on a day to day basis, at the cost of the potential employer. The vast majority of candidates do not have a local doctor – they either haven’t had the need for a doctor, or can’t get onto a local doctor’s books, or fell out of the book because they hadn’t seen their GP in a year. Therefore, if I find something that needs following up as a result of my visual screening examinations, I refer first to an optometrist, and then to a GP, armed with extra or confirmatory information. In this way, I can minimise the time to diagnosis and management for many conditions, and provide the beleaguered GP with as much information as possible to manage their patient’s care if needed. If the optometrist has the ability to refer to a specialist with respect to urgent findings, so much the better. If there were outpatient departments in rural hospitals with community rural GP registrar terms on offer, wouldn’t it be wonderful to have them trained in the use of such equipment, and its usefulness to their population health. Surely this is something we can make work?
Thank you for the insightful comments. It is clear that doctors of different specialties are concerned about the lack of government funding for eye health despite strong advocacy from many groups for decades.
It is important to note the work of Professor Mingguang He, an ophthalmologist, who is a Professor of Ophthalmic Epidemiology at the University of Melbourne and CERA. He is also the Chief Medical Officer for Eyetelligence which has developed a software (TGA approved) that uses the latest AI technology to analyse retinal images for features of glaucoma, referrable diabetic retinopathy, and neovascular AMD within seconds.
The authors believe that the adoption of new technologies such as Eyetelligence may be part of the solution to break down current systemic barriers deterring the widespread adoption of eye screening, particularly in rural areas of Australia. (No we do not have any vested interest in this company!)
Emeritus Professor Hugh Taylor AC raises an interesting point about past submissions suggesting pathology services perform eye screening to reach greater numbers of patients. Perhaps time to revisit this?
Emeritus Professor Max Kamien AM also raises an important point about properly training and funding GPs. However, Dr Gihan de Mel has shared a number of common barriers deterring eye screening in general practice including the cost of cameras.
The authors note it is now possible to lease high quality but lower cost portable eye cameras that could be funded by rural communities and shared across health services.
Also an interesting comment from anaesthetist Dr Ken Sleeman who notes that frailty is a common problem in patients undergoing surgery and an ophthalmic consultation may be necessary as part of a pre-op workup.
Wouldn’t it be wonderful if AI advances in eye screening made eye checks as easy, routine and fast as taking a patient’s vital signs?
Thanks Dr Gifar Hassan and Professor Leanne Rowe for such a thoughtful piece outlining a problem that is not sufficiently publicised and also making very practical suggestions. As we know avoidable and treatable eye disease has a massive impact on people’s lives, so it makes sense from a humanitarian and health system point of you to invest properly. Thanks for raising this issue in your article- Great work!
Great expose of current barriers in rural eye heath and suggested solutions including HMOs and GPs taking part in screening.
This is a very timely and excellent description of the short falls we face in eye care and some of the measurers that need to be taken to address these.
With reference to the screening of diabetic retinopathy, the original submission included have pathology services also perform screening. This was not adopted by the Department. Although the Commonwealth has funded retinal cameras for some 150 Aboriginal Health Services, the purchasing of a camera for most GP practices is not financially viable. However, to have cameras in pathology services would make sense as they service a much greater number of patients and the photos could be taken as bloods are collected and other testing done.
Fred Hollows will be turning in his grave in Bourke. All these problems could be fixed by properly training and funding GPs and the teams that they need to work with. and by freeing up time by getting rid of our annoying and wasteful bureaucracy. Not rocket science except for sickness bureaucrats.
I am in full agreement with your assessment of the situation. The lack of access to eye health care is a serious problem in Australia, and it is only getting worse.
In 2016, I presented at the RACGP Perth conference on the barriers and enablers to diabetic retinopathy screening in Australia. At the time, I had high expectations for newly introduced MBS items 12325 and 12326.
However, there are a number of issues that we face, including:
1- The cost of retinography. Even handheld retinal cameras are quite expensive.
2- The interpretation of retinal images (AI vs I – and its additional costs).
3- The possibility of missed diagnoses due to the technical limitations of handheld retinography, such as missed early macular degeneration (MD), glaucoma, and early neuromuscular changes.
4- Potential medico-legal issues related to the above limitations or missed diagnoses.
5- An ethical dilemma: Apart from remote and rural regions, most of us in metropolitan, suburban, and regional areas have access to very high-quality retinal imaging solutions directly through our local optometrists. Therefore, why not simply refer the patient to the optometrist for a comprehensive assessment. Why “scope-creep”?
6- Although co-claimable – extremely poor remuneration/rebate for the amount of clinical, cognitive and administrative burden in utilising this item number.
I hope your paper will help to raise awareness of the barriers to diabetic retinopathy screening, and solutions.
As an anaesthetist, frailty is an almost common problem in patients undergoing invasive surgery these days. It would seem that we should always include an ophthalmic consultation in our workup if the patient has not had a recent check