THE care of individuals with rare diseases has traditionally been challenging, owing to the large numbers of complex, undiagnosed patients with no treatment available. Rare diseases are undergoing a genomics-driven revolution, with opportunities for early diagnosis, clinical trials and, in some instances, treatment now changing the landscape.
We examine some of the changing concepts in the field of rare diseases, illustrating the importance of general practitioners and specialists gaining awareness of the impact of genomics on rare disease care.
Not so rare
Rare Voices Australia, the peak body representing Australians with rare diseases, defines a rare disease as any condition that is life-threatening or chronically debilitating, is statistically rare (with an estimated prevalence of one in 2000), or whose complexity demands special combined efforts to manage the disorder.
There are approximately 6000–8000 different rare diseases, with most having a genetic origin. Some examples of rare disease include cystic fibrosis, spinal muscular atrophy, and fragile X syndrome. While each disease is individually rare, collectively they are common, affecting one in 12 Australians. A small number of rare diseases are identifiable on newborn heel-prick testing, however, the majority have remained undiagnosed prior to the advent of genomic testing.
Diagnosis impacts lives
The early days of genetic testing involved the study of whole or substantially large segments of chromosomes, with Down syndrome being the most recognisable of these aneuploidy conditions. Since the completion of the Human Genome Project in 2003, there has been an explosion of technological advancement that now allows for the sequencing of an individual’s whole exome (protein-coding DNA sequence only) or genome (coding and non-coding DNA sequence).
Genomic testing currently enables a diagnosis in 30–50% of patients with a suspected rare genetic disease (here and here). While genetic conditions generally cannot be cured, a diagnosis can facilitate optimisation of medical care, for example, by rationalising anti-epileptic medication in the setting of some epilepsy syndromes, or instituting surveillance for disorders with a predisposition to malignancy. A prospective study of exome sequencing in infants with a suspected rare genetic disease has demonstrated a change in clinical management for 30% of those who received a diagnosis. In the intensive care setting, diagnosis of critically ill children can save lives by instituting appropriate care, such as the provision of lifesaving treatment and avoidance of invasive biopsies. Multiple studies have shown that despite the modestly high up-front cost of genomic testing, initiation of these tests early in the diagnostic trajectory is cost-effective and has high clinical utility (here and here).
The number of diseases for which treatment improves prognosis is growing. One such example is the metabolic condition biotin-thiamine-responsive basal ganglia disease (BTBGD). BTBGD is characterised by recurrent subacute encephalopathy often triggered by febrile illness, mild trauma or surgery. If left untreated, BTBGD can eventually lead to coma and even death.
The prompt administration early in the disease course of two readily available vitamins, biotin and thiamine, results in partial or complete improvement within days. There is no biochemical test to diagnose this condition, and a secure diagnosis requires the identification of pathogenic (disease-causing) variants in both copies of an individual’s SLC19A3 gene. Timely diagnosis of BTBGD via genomic testing can ensure this vital treatment is not only initiated but continued lifelong.
The once ambitious pursuit of gene replacement therapy has also now been realised. One of the first gene therapies to receive approval from the Food and Drug Administration in the US is voretigene neparvovec, a gene therapy for mutations in the RPE65 gene. Individuals with RPE65-related retinal disease can present with a variety of abnormalities, including pigmentary retinopathy, vascular attenuation, or pseudopapilloedema and macular atrophy. The therapy uses a neutralised virus as a delivery vector to transport a functional gene into the affected tissue in the eye. Once administered by subretinal injection, the new genetic material enables patients to produce the protein that is lacking as a result of their RPE65 mutations.
Following on from this success, there are currently more than 2600 gene therapy clinical trials that are either completed, ongoing or approved worldwide. In addition to gene therapy, there are other ways to treat genetic conditions. A hugely successful example is nusinersen, an antisense oligonucleotide medication that increases the level of functional survival motor neuron (SMN) protein for individuals with spinal muscular atrophy (SMA). One in 10 000 live births in Australia are affected by SMA, and until recently, there have been no effective treatments or a cure for this often life-limiting condition.
Another benefit of identifying the genetic cause of rare diseases will be the ability to undertake natural history studies for conditions that have to date been poorly understood. This will provide prognostic and management information for patients, their families and treating physicians. It will also inform reproductive choice by enabling accurate recurrence risk counselling. In a follow-up study of infants with a suspected rare genetic disease who underwent exome sequencing, the parents of diagnosed children had more subsequent pregnancies than those without a diagnosis. All pregnant couples at increased risk of recurrence utilised either pre-implantation genetic diagnosis (PGD) or prenatal diagnosis (PND). One couple continued with an affected pregnancy, as there was a treatment available for the condition. This pattern of reproductive choice corresponds with previous observations of couples either postponing or avoiding having more children when PND for a genetic condition was not available. Whether or not to use PGD and/or PND is a very personal choice for families. What remains important is affording families with rare disease the opportunity to pursue this option if they wish.
What does a rare disease diagnosis mean to families? While there is clear evidence for the diagnostic and clinical utility of genomic sequencing in rare disease, the psychosocial impact remains relatively unexplored in an Australian context. The “diagnostic odyssey” has been described as the time between when concerns are first raised regarding an individual’s health and when a diagnosis is reached. Anecdotally, undiagnosed adults and parents of undiagnosed children report that they value a rare disease diagnosis for its capacity to link them with similarly affected individuals, facilitate connection with researchers into their condition, and help them navigate support systems such as the National Disability Insurance Scheme (NDIS) and social security. Small-scale qualitative studies in North America show parents value genomic sequencing, even when results are non-diagnostic.
Parents of undiagnosed children are thought to have high rates of anxiety and depression, and that maintaining a positive outlook for their child’s future comes at a high emotional cost. Frustration remains for some parents and affected adults who receive a diagnosis of a newly described condition when there is minimal prognostic information, or a rare diagnosis that does not provide access to peer support (here and here). Parents value recognition of their role as expert carer for their child, as well as the high emotional and financial cost of the diagnostic odyssey (here and here).
Embracing genomics
A rare disease diagnosis can have an impact on every aspect of an individual’s life.
Early access to genomic testing for undiagnosed patients not only improves diagnosis rates but also ensures access to personalised care and the avoidance of a lengthy and exhausting journey of diagnostic uncertainty.
It will not be long before genomic testing becomes part of everyday clinical practice for many Australian doctors. As such, all health practitioners will need genomic literacy in order to provide excellent care to individuals with rare diseases. It is an exciting time to be curious about rare diseases and to challenge traditional thinking around the need for diagnosis and its impact on patients and families.
Useful rare diseases links:
- https://www.rarevoices.org.au/
- https://swanaus.org.au/
- https://www.stevewaughfoundation.com.au/about/rare-diseases/
- https://www.rarediseaseday.org/country/au/australia
- https://www.australiangenomics.org.au/our-research/disease-flagships/rare-disease-flagships/
- www.geneticalliance.org.au
- www.swanaus.org.au
Dr Natalie B Tan is a consultant clinical geneticist and genetic pathology trainee with Victorian Clinical Genetics Services, Murdoch Children’s Research Institute. Her PhD research aims to “solve the unsolved” cases in rare disease, utilising the latest in next generation sequencing technologies and applying functional genomics in the elucidation of novel disease genes.
Lyndon Gallacher is a Human Genetics Society of Australasia-certified genetic counsellor with Victorian Clinical Genetics Services, Murdoch Children’s Research Institute. He is project manager for the Victorian Undiagnosed Diseases Program and has a special interest in the psychological impact of genomic technologies on families.
Associate Professor Susan M White is a consultant Clinical Geneticist and Deputy Medical Director of Victorian Clinical Genetics Services, Murdoch Children’s Research Institute. She has a clinical and research interest in syndromes of childhood. Her genomic-focused research highlights the advantages of genomic testing, including demonstrating that genomic testing brings five times the diagnosis at half the cost of traditional diagnostic testing for children with undiagnosed syndromes. She worked with a team to implement clinical genomics on the Melbourne Children’s campus. She also worked with the Melbourne Genomics Health Alliance, whose work addressing the cost-effectiveness and clinical utility of genomic testing in clinical care led to an increase in Victorian genomics funding in 2017.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert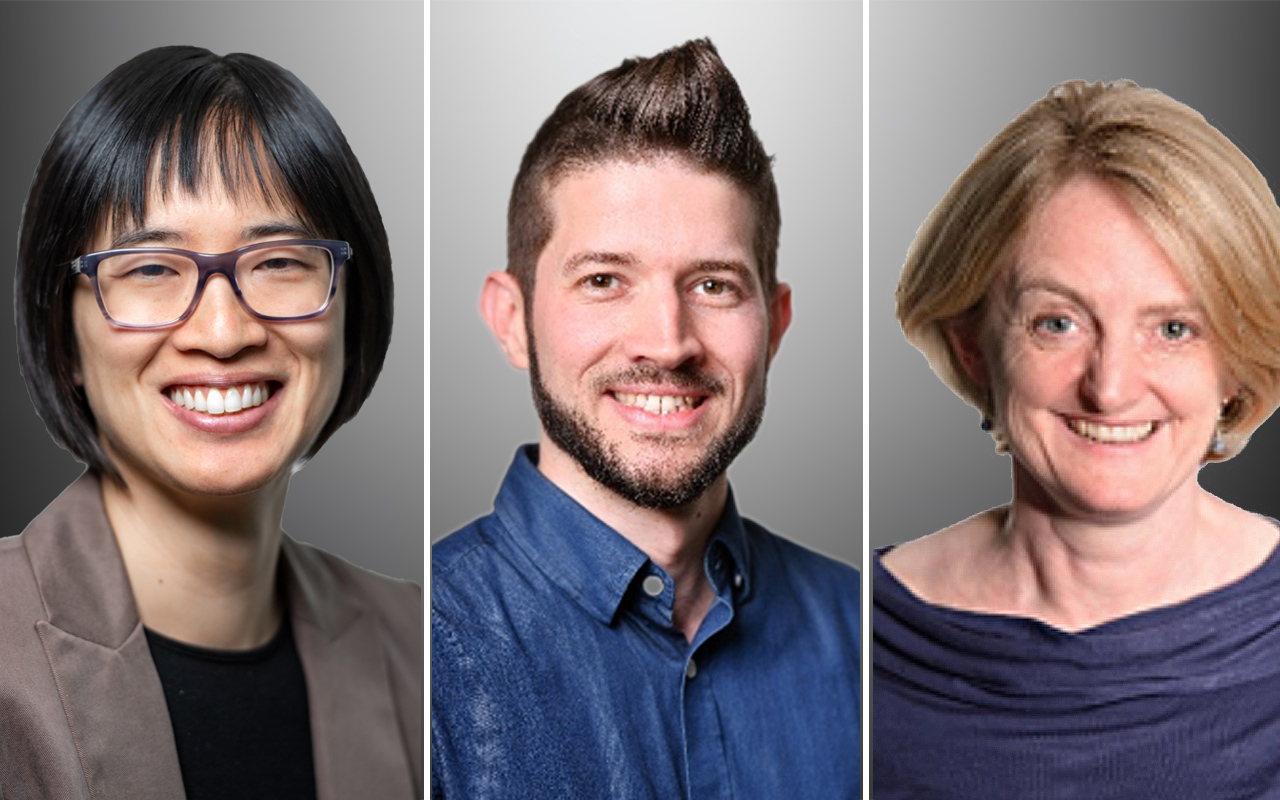
Dr Ronald Davis pioneered technology that fueled the Human Genome Project.
Now his greatest challenge is curing his own son.
https://edition.cnn.com/2019/05/12/health/stanford-geneticist-chronic-fatigue-syndrome-trnd/index.html
And an illness not so rare, and written about for over 70 years, but still ignored by many.