THE Australian Health Research Alliance (AHRA) encompasses all seven National Health and Medical Research Council (NHMRC) accredited Advanced Health Research Translation Centres (AHRTCs) and Centres for Innovation in Regional Health (CIRH). These cover over 90% of health and medical researchers and 80% of hospitals, with extensive primary care, Indigenous (inclusive of both Aboriginal and Torres Strait Islander people) health, and geographical reach. The aim of AHRA and member centres is to deliver better health through integrating research, health care and education. We are supported by the Medical Research Future Fund (MRFF) in national collaborative delivery of rapid applied research and translation.
AHRA has prioritised women’s health and established the National Women’s Health Research, Translation and Impact Network (AHRA WHN), in the absence of a national collaborative body in women’s health research and translation. The AHRA WHN committee was nominated by the AHRTCs and CIRHs, considering diversity across discipline, geography, career stage and life stage research focus. We engaged key stakeholders including consumer groups, the Royal Australian College of General Practitioners, the Royal Australian and New Zealand College of Obstetricians and Gynaecologists, the Australian College of Midwives, the Australian Women’s Health Network and leaders in Indigenous and cultural and linguistically diverse women’s health. This group is integrally embedded in the extensive AHRA national network of health service-led centres, with members across hospitals (private and public) and primary care. Initially, we aimed to codevelop and implement strategic research and translation priorities, alongside the government’s new Women’s Health Strategy, to inform recently announced MRFF funding in women’s health.
The first National Women’s Health Policy was released in 1989 and updated in 2010. Australia has made headway in women’s health through the focus on chronic disease prevention, mental health and wellbeing, sexual and reproductive health, and healthy ageing.
However, gender inequity in mental and physical health persists, with women at greater risk of mental ill-health, and heart disease being under-recognised and suboptimally managed in women. In clinical and preclinical trials, insufficient representation of females and/or a lack of analysis of results by gender may limit the validity results for women. Biological, psychological and socio-economic impacts of gender adversely affect health across the life course, including through the pre-conception, pregnancy and post partum periods. It is also important to recognise gaps, with many women experiencing lower quality of life due to gender-specific and social factors affecting health, health seeking behaviour, access to information and health practices (here and here). Therefore, targeted strategies are needed in specific health issues for women and girls.
In 2018, the federal Minister for Health, the Honourable Greg Hunt MP, announced the development of an updated National Women’s Health Strategy 2020–2030. This builds on the existing National Women’s Health Policy 2010, with opportunities to address challenges including equitable access for appropriate care that is needs-based and culturally responsive; a clearer focus on priority populations; multidisciplinary, integrated and collaborative care approaches; integration of physical and mental health; and a prevention emphasis. Uniquely, a key goal of the strategy is investment for strategic prioritised research focused on Australian women’s health needs.
There are many national groups working to improve women’s health, including the professional colleges and societies and the Australian Women’s Health Network. However, a national coordinated approach to research and translation integrated into health care has been lacking. Our network aims to address this gap; as a large-scale national collaboration, accredited by the NHMRC and funded by the MRFF to integrate research, translation and education, we are well positioned for strategic high impact research and translation.
Here we describe the AHRA WHN network prioritisation activity. We aimed to engage stakeholders and codevelop national women’s health research and translation priorities, to inform policy and funding, strategies and to optimise national collaborative high impact research and translation. The priority setting methods and process are presented in Figure 1, and involved inputs from evidence synthesis (a comprehensive review, The current state of women’s health in Australia, prepared for Jean Hailes for Women’s Health to inform the development of the Women’s Health Strategy) and the draft for the Women’s Health Strategy, supplemented by expert and stakeholder input (electronic dissemination across the AHRA Centre’s and stakeholder groups nationally).
Figure 1. Priority setting process
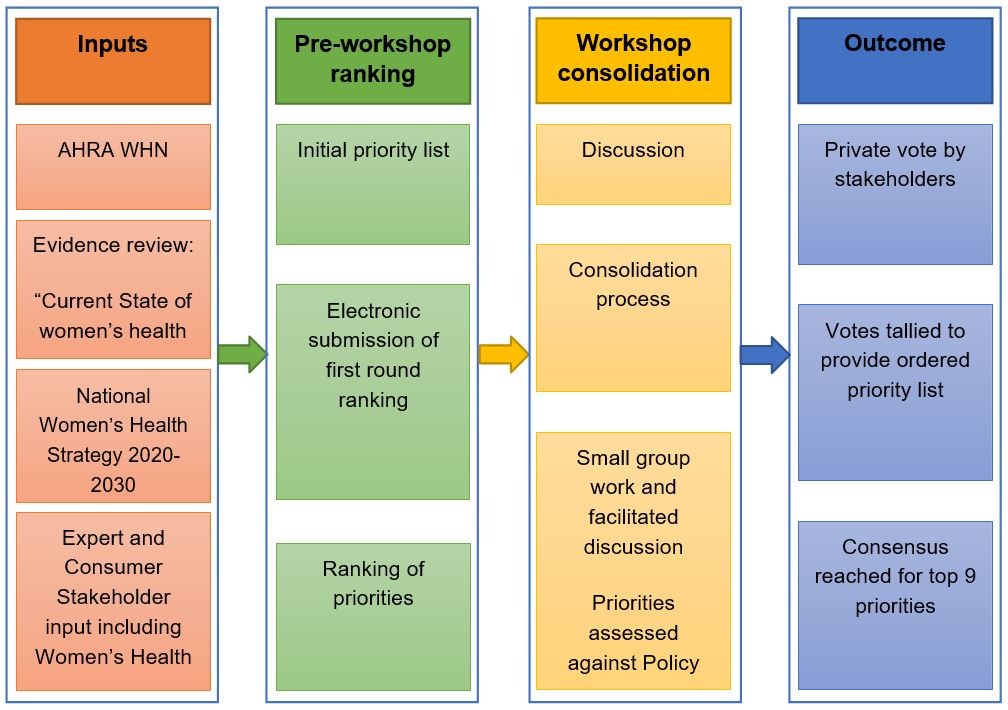
This was followed by a national workshop, applying a well established modified Delphi and Nominal Group Technique for consensus codevelopment. Nine women’s health research and translation priorities were agreed upon (Table 1).
| Table 1. | Women’s health research and translation priorities |
| 1 | Pre-conception, pregnancy, post partum and intrapartum health of women and babies |
| 2 | Mental health |
| 3 | Reproductive health* |
| 4 | Chronic disease and preventive health |
| 5 | Healthy lifestyle, nutrition, physical activity and the prevention of obesity |
| 6 | Violence and abuse |
| 7 | Indigenous health |
| 8 | Healthy ageing |
| 9 | Sexual health* |
| * The World Health Organization (WHO) definitions for reproductive health and sexual health were endorsed during this process |
Seven overarching principles were also codeveloped across all the priorities (Table 2).
| Table 2. | Overarching principles for research and translation in women’s health |
| 1 | Women in their lived environment, including social determinants of health |
| 2 | Responsibility for codesign, translation and impact |
| 3 | Community engagement and empowerment |
| 4 | Primary, secondary and tertiary prevention across all priorities |
| 5 | Health literacy and shared decision making |
| 6 | Equity for priority and vulnerable populations, including Indigenous Australians, culturally and linguistically diverse people, refugees, gender diverse individuals, and those in rural and regional areas |
| 7 | Research processes require partnership, transparency, governance, priority setting, stakeholder engagement and large-scale collaboration — hence, it requires sophisticated processes and organisations with the capacity, credibility and capability to undertake these processes |
Once consensus was reached on priorities, more detailed research and translation topics were workshopped under the nine priorities. These underwent consultation nationally across AHRA Centres and stakeholder groups, with high level consumer input.
The top ranked research and translation priority in women’s health was pre-conception, pregnancy, post partum and intrapartum health of the mother and infant. Within this, key areas were identified, including personalised, individualised care, diminishing variation in access to care and new models of care. Specific research and translation activities were identified, with lifestyle, obesity prevention and mental health being prioritised at all stages and for pre-conception (eg, reproductive planning, infertility and the role of partners), pregnancy (eg, nutrition, risk prediction and chronic disease), intrapartum (eg, induction of labour, mode of birth, perineal injury, analgesia, short and long term impacts of care decisions), and post partum life stages (eg, breastfeeding, environment, planning and contraception, and self-care). The development and implementation of evidence-based guidelines for pre-conception, childbirth and early parenting were recognised. Integration of care across the continuum of pre-conception through pregnancy and post partum was considered critical.
Women’s mental health was also prioritised. Accordingly, research and translation goals were focused across the life course including, fertility and infertility, adolescence, the reproductive years, maternal–child attachment, menopause, and older age, with a focus on mental health conditions more common in women, including anxiety and depression. Adversity and socio-economic disadvantage, development of resilience, minimising social isolation and poverty, guideline development and implementation, screening and improvements in care were all prioritised in future research.
The third ranked priority was reproductive health, recognised separately from sexual health. Evidence-based guidelines for infertility treatment, understanding links between high risk pregnancy and long term non-communicable diseases, alongside access to contraception, emergency contraception and safe abortion. Further research into services, monitoring of outcomes, interventions and prevention for endometriosis, polycystic ovary syndrome, infertility, early menopause, gynaecological cancers, prolapse, incontinence and hysterectomy were also highlighted.
With one in two Australian women affected, and major burden for individuals, families, carers and the health system, chronic diseases and preventive health were also prioritised. The main burden in Australia relates to cancer, musculoskeletal conditions, and cardiovascular disease, with cardiovascular disease, dementia and cancer leading the causes of death. Research into prevention, treatment and models of integrated, person-centred care were highlighted, and integration with other areas identified, including mental health, lifestyle, Indigenous health and healthy ageing. Healthy lifestyle, nutrition, physical activity and obesity prevention were deemed important. This reflects unhealthy lifestyle and the increasing burden of obesity, which underpins most chronic diseases and is the greatest public health threat facing Australian women.
Violence and abuse were clearly recognised as imperative to address for Australian women, especially with little impact of policy efforts to date, emphasising the vital need to develop and implement evidence to effectively tackle this challenging issue.
Indigenous health is relevant to all priorities and is encompassed in the principles; however, it was felt to be important enough to target independently, given the high disease burden and mortality in Indigenous women.
Healthy ageing is a culmination of all of these priorities and, while life expectancy is long, quality of life is adversely affected by comorbidities. AHRA has also established an Ageing Research and Translation Network in this high priority area. Sexual health was also deemed important for research and translation in women’s health. Detailed areas under each priority are under iterative development, with ongoing consumer and stakeholder engagement (monashpartners.org.au).
Seven overarching principles (Table 2) were identified, recognising factors relevant across all aspects of women’s health, including social determinants, community engagement and empowerment, health literacy, shared decision making, and equity for priority and vulnerable populations. As the Australian community is the funder and beneficiary of research and translation and of health care, stakeholder engagement and partnership, transparency, and large-scale collaboration with a strong focus on impact are vital. Training researchers in consumer and community involvement and cultural awareness was highlighted. The AHRA WHN is committed to these principles and to codesign and participatory research approaches.
In summary, considerable research and translation activities are needed to continue to improve the health of women and girls. The National Women’s Health Strategy, the Strategy for Medical Research and Innovation and the upcoming MRFF funding provide the impetus for national collaborative action. Here, as a peak national body for women’s health research, translation and impact across the lifespan, the national AHRA WHN network outlined our national priority setting process and discussed the resultant priorities and principles. We seek to support government policy and strategy, to inform future women’s health research, translation and impact funding and to catalyse national collaborative research, through transparent peer-reviewed mechanisms, across the AHRA network and stakeholders nationally.
Professor Helena Teede is Executive Director of Monash Partners Academic Health Research Translation Centre, Director of the Monash Centre for Health Research and Implementation, Monash University, and an endocrinologist at Monash Health.
Dr Briony Hill is a Research Fellow at the Monash Centre for Health Research and Implementation.
Associate Professor Jacqueline Boyle is an academic obstetrician/gynaecologist and is Deputy Director of the Monash Centre for Health Research and Implementation.
Ms Leslie Arnott is consumer participation officer at Health Issues Centre and co-director of Lamaze Australia.
Professor Rod Baber is an OB/GYN at North Shore Private Hospital in Sydney. He is president of the International Menopause Society and past president of the Australian Menopause Society.
Professor Julie Byles is the Global Innovation Chair in Responsive Transitions in Health and Ageing at the University of Newcastle.
Ms Rita Butera is Chief Executive Officer of safe steps Family Violence Response Centre in Melbourne.
Professor Anna DeFazio heads the Gynaecological Oncology Research Laboratory at the Centre for Cancer Research, the Westmead Institute for Medical Research in Sydney.
Professor Maralyn Foureur is Joint Chair and Professor in the School of Nursing and Midwifery at the University of Newcastle.
Dr Jacqueline Frayne is a Senior Lecturer in General Practice at the University of Western Australia Medical School.
Ms Karen Glover is a Mein:tnk and Wotjobaluk woman from south eastern SA and north western Victoria. She holds a joint appointment as Senior Research Fellow at the South Australian Health and Medical Research Institute and the Murdoch Children’s Research Institute, where she is Co-leader of Aboriginal health within the Healthy Mothers Healthy Families Group.
Professor Martha Hickey is an OB/GYN at the Royal Women’s Hospital in Melbourne. She is professor of Obstetrics and Gynaecology at the University of Melbourne.
Professor Deborah Loxton is Deputy Director of the Australian Longitudinal Study on Women’s Health and co-Director of the Priority Research Centre for Generational Health and Ageing at the University of Newcastle.
Professor Gita Mishra is Head of the Epidemiology and Biostatistics Division and Professor of Life Course Epidemiology at the School of Public Health, University of Queensland. She is also Director of the Australian Longitudinal Study of Women’s Health.
Professor Janette Perz is Director of the Translational Health Research Institute at Western Sydney University.
Professor Susan Walker the Head of the Department of Obstetrics and Gynecology at the University of Melbourne and also the Director of Perinatal Medicine at Mercy Hospital for Women.
Professor Maria Makrides is the Theme Leader for Healthy Mothers, Babies and Children at the University of Adelaide. She is also Director of the Child Nutrition Research Centre with its headquarters at the Women’s and Children’s Hospital.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert
Hello, I feel the time has come to create a greater profile in the community for Gynaecological health awareness (women’s conditions which are lifetime issues) i.e. PCOS Menopause, Fibroids, GYN Cancers, Prolapse, Hysterectomies, STI’s LS. Vulval issues – opposed to Reproductive health – (having babies).
Regards Kath Mazzella OAM