Trauma-informed preventative care (TIPC) is a framework for the delivery of care that involves realising the high prevalence of psychological trauma, recognising and addressing its impact on patients, their families and staff and preventing traumatisation during episodes of care. Implementing TIPC in a hospital setting requires an organisation-wide approach based on a shared understanding and a shared language of trauma and trauma-informed care. Leadership support is essential for driving organisational change.
In hospitals, trauma is often thought of as physical injury. The Substance Abuse and Mental Health Administration provides a broader definition of trauma that is widely accepted: Trauma results from an event, series of events, or set of circumstances an individual experiences as physically or emotionally harmful that can have lasting adverse effects on the person’s functioning and mental, physical, emotional, or spiritual wellbeing.
Trauma-informed care (TIC) is an organisational framework oriented to deliver care that recognises and responds to the effects of psychological trauma. It incorporates the principles of choice, safety, collaboration, empowerment and trust. TIC aims to mitigate the impact of trauma by recognising how past experiences could impact safety and care and by finding ways to prevent re-traumatisation. TIC applies to children as much as adults. Research has shown that children, families, carers and kin are more likely to experience positive interactions and lower re-traumatisation when health care providers use TIC.
TIC also promotes staff wellbeing for those who bring their lived and living experiences of trauma or vicarious trauma to the workplace. Indeed, Dr Joceyln Lowinger wrote in InSight+ about the need to address underlying trauma in the medical workplace by using trauma-informed education.

Trauma-informed care in Australia
In Australia, an estimated half to two-thirds of young people are exposed to at least one traumatic event by the time they turn 16 years old. Medical care can also be experienced as traumatic, with up to 80% of ill or injured children and their families experiencing traumatic stress reactions following life-threatening illness, injury or painful medical procedures. There is growing awareness of the importance of a trauma-informed approach, especially for supporting Aboriginal and/or Torres Strait Islander children who have an elevated risk of trauma due to experiences such as intergenerational trauma related to colonisation and racism. Children who live in out-of-home care, are at high risk due to histories of abuse or neglect.
Varying definitions of TIC and inconsistencies in terminology between policies, guidelines and frameworks pose barriers to the implementation of TIC. Other implementation challenges include a limited evidence base for translating TIC to specific practice and service settings and a lack of specific guidance for the implementation of TIC in paediatric health care, especially in the paediatric hospital context.
A national framework by the Australian Institute of Family studies (2013) outlines interventions for Aboriginal and/or Torres Strait Islander children who have experienced trauma. This framework also recognises the importance of trauma-informed services focusing on the developmental needs of all children. The 2020 – 2030 National Action Plan for the Health of Children and Young People outlines the need to implement an overarching framework for TIC in Australia.
Resources are being developed to help organisations identify how to implement TIC. Recommendations from the Trauma-Informed Care and Practice Organisational Toolkit and Orygen’s clinical practice report highlight the need to increase trauma-informed training for all staff; to align TIC principles across organisational policies and procedures; and to use the influence of TIC champions to drive change implementation.
Implementing a trauma-informed preventative care approach: a case study
Implementing TIC in a hospital setting requires a whole-of-organisation approach including shared understanding, implementation support and consistent measures of outcomes. Leadership buy-in is essential for successful implementation. At the Melbourne Children’s Campus, with the aid of lived experience advisors from our network of 1700 participants, we are designing, testing and evaluating a range of trauma-informed approaches.
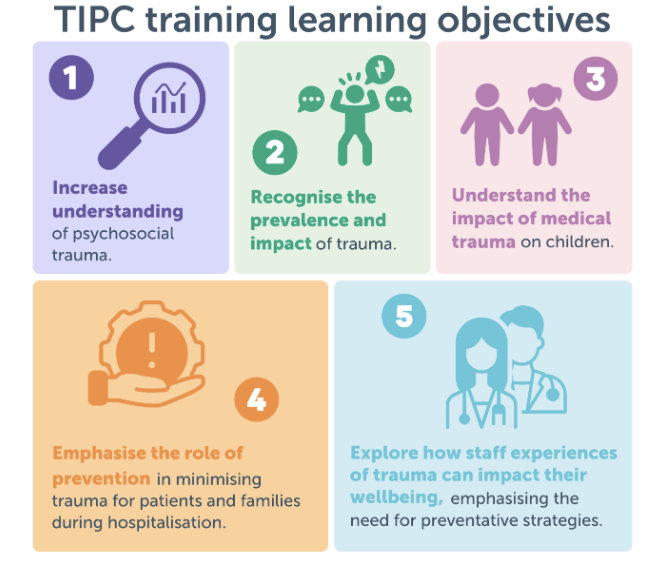
As a more novel approach, we have introduced the preventative concept into our definition of TIC. The TIPC foundational training was developed with input from a working group comprising staff across the Melbourne Children’s Campus and lived experience advisors. The learning objectives are presented in Figure 1. The training used a multi-method approach for engagement, utilising video, audio and infographic content along with reflective exercises. Our online foundational training is being piloted at the Royal Children’s Hospital Melbourne (the RCH).
We are also evaluating the Behaviour Support Profile (BSP), a trauma-informed tool integrated within the electronic medical record at the RCH. Information about patients’ psychosocial needs is often incomplete, scattered or absent. The BSP serves as a centralised platform to document the non-medical needs and preferences of children and young people coming into hospital. The BSP promotes a preventative approach to care and aims to reduce re-traumatisation in subsequent hospital visits. The evaluation assesses effectiveness, usability and acceptability of the BSP, using staff and family feedback to optimise the tool in the electronic medical record and business as usual workflows.
A look ahead
The ongoing implementation of TIPC foundational training and evaluation of the BSP at the RCH and the Melbourne Children’s Campus provides opportunities to test the implementation proof of concept. The following next steps support a way forward to implement and deliver TIPC.
Next steps
- Ensure that the TIPC foundational training can be accessed by all staff to increase trauma awareness and develop the foundational skills required to implement TIPC.
- Embed TIPC into organisational policies and procedures and into clinical care, research and education.
- Embed the preventative component of TIPC in paediatric hospital settings to complement existing trauma-informed national and state frameworks.
Conclusion
TIPC allows organisations to address the psychosocial needs of children and their families in hospitals, thereby supporting safety, wellbeing, healing and recovery. By shifting to a trauma-informed organisational approach, we can ensure paediatric hospitals are a place where all children, families, carers, supporters, and staff can thrive.
Dr Catherine Olweny is the Key Area Lead for Trauma Informed Preventative Care, Melbourne Children’s Campus Mental Health Strategy and Staff Anaesthetist at the Royal Children’s Hospital, Melbourne.
Kayla Elliott is a researcher with the Prevention Innovation Group at the Murdoch Children’s Research Institute.
Alma Giborski is a Senior Project Officer for Trauma Informed Preventative Care, Melbourne Children’s Campus Mental Health Strategy.
Anitha Thiraviarajah is an Advocacy Lead for the Melbourne’s Children’s Campus Mental Health Strategy.
Professor Sharon Goldfeld is a Steering Committee member for the Melbourne Children’s Campus Mental Health Strategy and paediatrician, public health physician, Theme Director of Population Health and Co-Group Leader of Policy and Equity at the Murdoch Children’s Research Institute and Director of the Centre for Community Child Health at MCRI and the Royal Children’s Hospital, Melbourne.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert