New best practice guidance will support Australia’s national clinical quality registries to provide more timely and meaningful feedback to clinicians and health service organisations.
There is a wealth of data to monitor health care outcomes in Australia, but some of it lacks the detail and timeliness that clinicians and health service organisations need to improve the care they deliver.
National clinical quality registries (CQRs) have been the main way to fill this gap in clinical quality outcomes data.
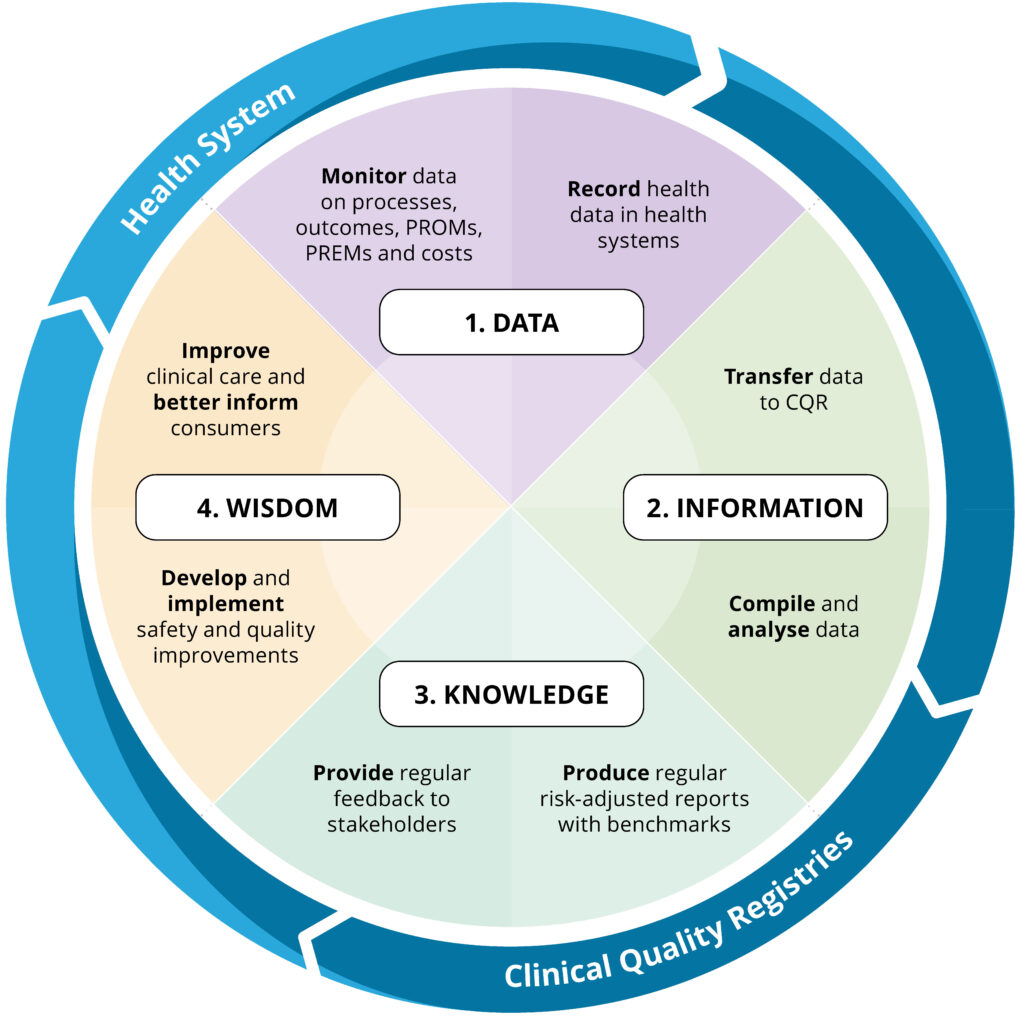
CQRs systematically monitor and report on the appropriateness and effectiveness of health care for people with a particular health condition. They provide clinicians and health service organisations with evidence-based feedback on clinical outcomes and unwarranted variation in care, allowing them to benchmark their local data against peer hospitals and state and national data to see where they can improve care.
The number of CQRs in Australia has increased over recent years. While high-functioning and mature CQRs, such as those covering hip fracture, diabetes, stroke and dementia, routinely provide data back to clinicians and health service organisations to support timely improvements in care, others are yet to reach that level of functioning.
A new framework provides a strategic roadmap and pragmatic directions for all CQRs, particularly developing registries, to provide timely feedback so that clinicians and health service organisations can improve care.
The Australian Framework for National Clinical Quality Registries 2024 (the Framework) is a principles-based document that was produced by the Australian Commission on Safety and Quality in Health Care (the Commission). It is an update to the Framework for Australian Clinical Quality Registries 2014. The Framework is part of a national body of work to help established and aspiring registries contribute to a learning health system that achieves better health care and patient outcomes.

The Framework was revised in response to significant changes in the landscape for CQRs. In Australia, traditionally CQRs have been bottom-up, clinician-led research initiatives to identify issues and improve outcomes in specific clinical areas. The focus for CQRs is no longer only on collecting process and outcome data. While this is still important, CQRs are moving to the next level — using data for quality improvement.
There is also increasing recognition that for CQRs to effectively drive improvements in care, coordination at the highest possible level (state or national) is needed to avoid duplication, improve participation rates, enable benchmarking and provide meaningful feedback to stakeholders.
How was the Framework revised?
The Commission led a robust process to revise the Framework, including working with an expert advisory group of CQR operators, clinicians, a consumer advocate and Commonwealth, state and territory health department representatives. A national public consultation on the revised draft Framework included a national online survey, virtual workshops and written submissions. The Commission also reviewed CQR best practice nationally and internationally.
What is in the Framework?
The Framework includes a new quality standard for establishing and operating CQRs, which aligns with the National Safety and Quality Health Service Standards and guides CQRs towards best practice.
It supports CQRs to establish appropriate governance, including data governance, and collect the right data in the most efficient way (from electronic records where possible) that informs quality improvement.
The Framework also guides CQRs to:
- analyse data appropriately and use data quality assurance processes that ensure the data accurately reflect practice;
- generate timely risk-adjusted reports;
- identify and report on unwarranted health care variation; and
- provide access to data for research.
How will the Framework benefit clinicians and health service organisations?
The major benefit for clinicians and health service organisations is that the Framework guides CQRs to provide timely and meaningful reports that can be used to improve care.
The Framework supports CQRs to establish systems, such as data dashboards, that will allow clinicians and health service organisations to see a tangible output from the data they input into registries and to receive real-time feedback on local quality improvement activities.
An example is the Australian Stroke Clinical Registry (AuSCR), which provides a dashboard for clinicians and health service organisations to extract data and supports local and statewide quality improvement initiatives.
The Framework also focuses on sound data governance that will reduce risks associated with data collection and management, increasing clinicians and health service organisations’ confidence that the reports are based on good quality data.
Working in partnership to improve care
CQRs are not enough on their own to improve care. The Framework emphasises that collaboration and partnership between CQRs, clinicians and health service organisations can achieve better patient outcomes. It encourages clinicians to become involved in CQR governance and to collaborate on quality improvement activities.
The Framework will help clinicians and health service organisations to see the value of the CQRs and to measure the maturity of their own registries. When clinicians contribute to a CQR, they drive better patient outcomes through robust and modern data collection analysis and reporting, contributing to the learning health system nationally. Clinicians who participate in a CQR are able to influence what data it collects.
The Framework also emphasises the need to include patients, carers and consumers in registry data governance and design. Consumer participation in CQRs has been shown to lead to better health outcomes and improve services for patients and the community. The Framework includes an increased focus on consumer participation, especially vulnerable groups, and on including consumers in data governance.
Find out more
- Download the Framework and fast facts for clinicians and health service organisations.
- Find out which health services in your area are contributing data to clinical registries. Search the Australian Register of Clinical Registries, which lists more than 120 clinical registries, audits and databases that collect health information and participating sites.
Professor Sandy Middleton is Chair of the Clinical Quality Registries Framework Review Advisory Group; Director of the Nursing Research Institute, St Vincent’s Health Network; and Chair of the Australian Stroke Clinical Registry.
Suchit Handa is the Director of Measurement for Improvement, Australian Commission on Safety and Quality in Health Care.
Kass Adams is a Senior Project Officer of Measurement for Improvement, Australian Commission on Safety and Quality in Health Care.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Hear! Hear! Dr Chalmers.
Dilktats from 9am to 3 pm armchair bureaucrats rarely help frontline workers, no matter how many glossy brochures and posters are placed in the lifts (never in stairwells) and on patients room walls and no matter how many compulsory modules they institute.
Talk about re-arranging the deck chairs on the Titanic.
Vital sectors of the healthcare system, two front-line ones being general practice and all medicos employed by State Health institutions are crumbling around us from ageing without replacement and exploitation and over-control and ivory tower theorists are planning yet another layer of theoretical perfectionism.
The practice of medicine is not a science and never has been, it is a craft for want of a better word.
For centuries, craftsmen have started as apprentices who learned on the job actually confronting the task particular to their craft.
Hand-on participation under the eye and guidance of the master craftsman is the core of the development of skill and excellence.
In the course of the interaction, much teaching about fundamentals occurs which is vital and the theory and the practice go hand in hand.
During my lifetime, step by step, the practice of medicine has been encroached upon by rules, regulations, restrictions and bureaucracies distorting the practice out of all recognition.
The procedures may be much more complicated, the equipment much more elaborate and the medications available answers to old doctors dreams but our humanity has not changed.
Now, the young do not want to join us and the committed are collapsing under the strain and the politicians are selling the fable of infinite progress and totalitarian patient rights without heeding the human toll on the doctors and diminishing both their financial rewards and their satisfaction at their accomplishments.
What a mess!