MOST women starting treatment with assisted reproductive technology (ART) will eventually take home a baby, according to research that has estimated the rate of live births across a full course of treatment and including both fresh and frozen embryo transfers.
The research, published in the MJA, estimates the cumulative live birth rate (CLBR) for up to eight cycles, stratified by a woman’s age on commencing ART treatment.
The prospective follow-up of more than 56 652 women commencing ART in Australia and New Zealand between 2009 and 2012, found an overall CLBR of 32.7% in the first cycle, increasing to between 54.3% and 77.2% by the eighth cycle.
The authors found that while the cycle-specific rate declined in line with age and the number of complete cycles, the CLBR increased with each consecutive cycle.
For example, women starting treatment at age 30–34 years had a 43.4% of having a baby after the first complete cycle, and a 69.4% (conservative estimate) to 91% (optimal estimate) chance of taking home a baby after eight cycles. Women starting treatment aged 40–44 years had a 10.7% chance of having a baby after the first cycle, and a 21% (conservative) to 37.9% chance after eight cycles.
Lead author Associate Professor Georgina Chambers, Director of the National Perinatal Epidemiology and Statistics Unit at the University of NSW, said that the data should be reassuring for women commencing ART.
“We hope that providing data in this more meaningful way is reassuring for women,” Professor Chambers told MJA InSight. “If you look at the success rate over a course of treatment, most women will take home at least one baby.”
Professor Chambers said that the CLBR data provided success rates across consecutive rounds of complete ART treatment cycles, including fresh and frozen embryos associated with each ovarian stimulation, reflecting a change in contemporary clinical practice that had occurred over the past decade.
“[The data analysis] reflects the increasing central role of cryopreservation programs in ART clinical practice, whereby in an increasing number of cycles, all embryos are frozen and transferred in a frozen cycle.”
Professor Chambers said that presenting the data in this way would also further encourage single embryo transfer because the data did not focus on the result of each individual embryo transfer, but an entire course of treatment. Single embryo transfer is important in order to minimise the risks associated with multiple pregnancies.
Professor Chambers said that the conservative estimate assumed that all women who dropped out had zero chance of having a live birth, and the optimal estimate assumed that all women who discontinued treatment had the same chance as those who continued with treatment.
She said that the conservative rate was likely to be too pessimistic, and the optimal rate was overly optimistic, so the true estimate would lie somewhere between these two figures.
Professor Gab Kovacs, professor of obstetrics and gynaecology at Monash University and a pioneer of in vitro fertilisation (IVF) in Australia, welcomed the findings. He said such an approach – also called a life table analysis — was the most appropriate way to describe the true pregnancy rate using ART.
Also, he said, the inclusion of frozen transfers was important in presenting the most accurate estimates for patients.
Professor Kovacs said that the data would help to inform discussions between patients and doctors regarding their chances of taking home a baby after a course of IVF. But, he added, these discussions would always be challenging.
“No matter how you present the figures – and I think this is much better than the per cycle pregnancy rate – it’s really difficult to explain it to patients,” Professor Kovacs said. “Patients still don’t believe it. They put on their rose-coloured glasses, and they say I feel really young for my years, I’m really fit, I’m really healthy – I don’t care what the chances are, I have a much better chance because I am a better prospect.”
Professor Kovacs noted that the data reflected only the first baby resulting from an egg collection, so even the optimal rates would underestimate the chances of success.
“It’s not uncommon to have embryos frozen and have more than one baby from one attempt, and this type of analysis – because you can’t get a bonus for having two pregnancies — actually underestimates the overall chances. I would probably give my patients the optimal rate,” he said.
Professor Chambers said that the data did reflect only the first baby born to a woman using ART treatment and was a conservative estimate. She added that the estimate CLBR range reflected the high discontinuation rate in ART.
“The discontinuation rate after an unsuccessful ART cycle is around 30%, but we don’t know the prognoses for the women who dropped out,” she said, adding that patients may discontinue treatment for a range of reasons. “It may be physical, emotional, it may be a change of relationship, or due to the cost.”
In an accompanying editorial, to be published on 7 August, Professors Stephen Robson and Caroline de Costa also welcomed the CLBR data, noting that it “breaks new ground” in improving the clarity on the likelihood of conceiving with IVF treatment and how this is affected by age and the number of cycles required.
The MJA authors noted that the findings will also help to inform public policy.
Professor Chambers said that it was important for policymakers to look at IVF over a course of treatments. “This sort of data allows policymakers to look at the success of treatment over multiple cycles, which is more realistic of clinical practice than individual cycles’ success rates,” she said.
An ART Working Group, established last year as part of the Medicare Benefits Schedule Review Taskforce, is evaluating 14 assisted reproductive services.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert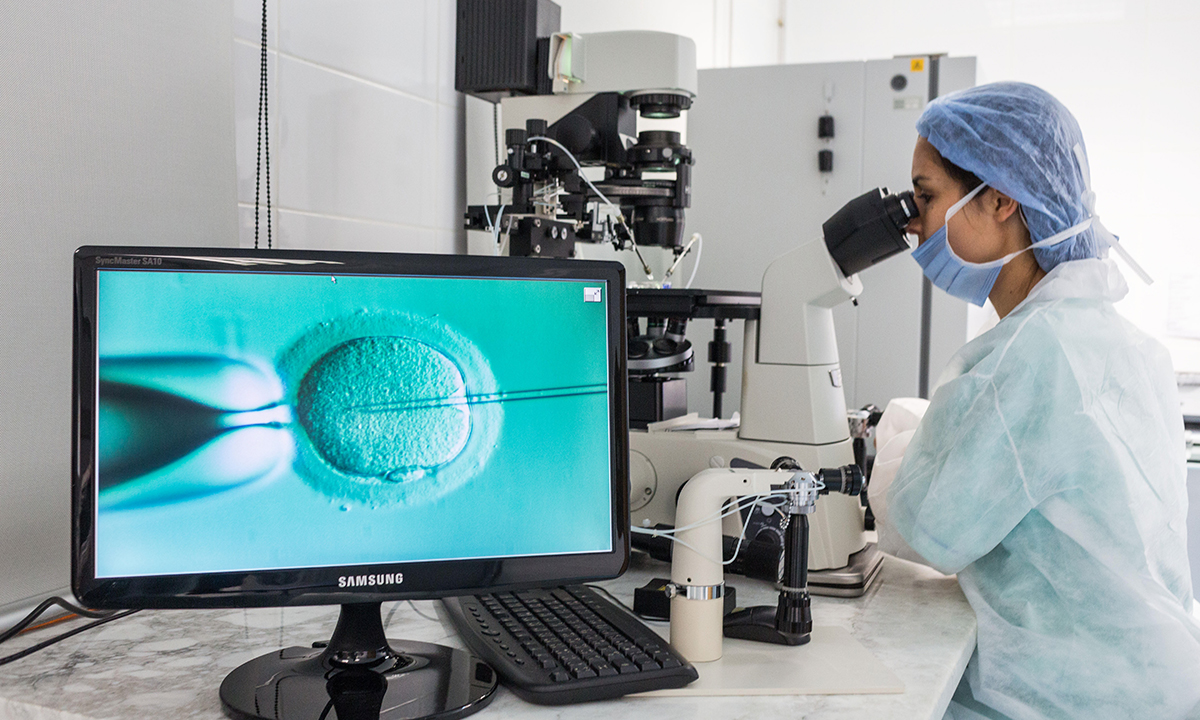
To add to the response to Andrew’s question:
-should Medicare stop funding psycho/geriatricians for treating dementia – it is a life limiting illness after all
-what about stopping treatment for people with cancer – it is a life limiting illness while you’re there
-how about we stop overprescribing antibiotics for colds – it only build resistance and harder to treat conditions down the line
-another thing, why are we treating alcohol dependence with medications – people just return to drinking
-people with mental health conditions – aren’t they just lazy or precious?
-why have a Medicare system in the first place – people eat junk food, don’t exercise or engage in preventative measures to look after their health
We must remove the stigma associated with infertility treatment.
Infertility is a medical condition. There is inequity of services because of the financial cost involved. Couples miss out who are unable to meet the costs. The data presented in the article is to help work out treatment dose for infertile couples in brining a healthy child home.
Children ultimately are an asset to our country.
In reference to Andrew’s questions I might add one. Women have been encouraged by society and governments to gain qualifications and develop careers so that they can make a longer and more significant contribution to GDP and taxation collections. This has resulted in an average decade delay for today’s mothers-to-be in their age at birth of first child over the past fifty years. It is no surprise as the fertility curve descends (for both men and women) that we are seeing greater numbers of women (and men) presenting in the years of their declining fertility unable to secure a natural pregnancy and to have a family. And no profession better demonstrates this situation better than our own.
Given the very significant increase to GDP through this increased female contribution and consequently the government taxation collections is there not a reciprocal obligation for governments to provide assistance when this change in social behaviour results in an increasing number of couples finding it difficult to secure a pregnancy and need to seek treatment?
It is easy to get caught up in the either or trap in the health funding argument instead of where the real focus should be which is whether treatment is indicated and appropriate.
What is the cost to Medicare (and the taxpayer) for each cycle of unsuccessful IVF?
What is the total cost to Medicare (and the taxpayer) from the IVF industry each year?
How fast is the cost of IVF growing year on year?
What other health priorities are being underfunded due to the expense of offering unlimited IVF cycles?
Surely these are all very relevant questions. What a disappointment that the author of this piece hasn’t addressed any of them.