Melioidosis is endemic in Cairns, with the number of cases increasing since 2015 (here and here). This year, however, there has been an extraordinary season, with more than four times the number of cases in Cairns already than in any prior year. One hundred cases of melioidosis have been reported in the Cairns and Hinterland Hospital and Health Service from 1 January to 13 April 2025.
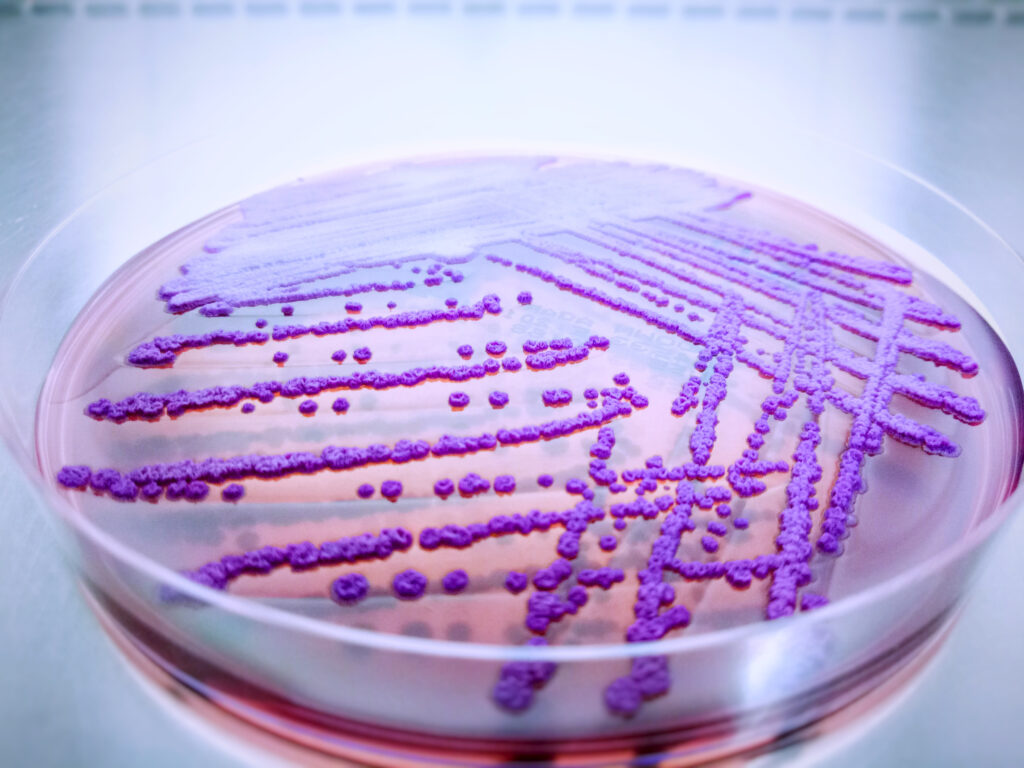
Melioidosis is a life-threatening infectious disease caused by Burkholderia pseudomallei, a bacterium that lives in the soil and surface water in northern Australia. Most cases of melioidosis in northern Australia occur during the wet season when the water table rises, bringing the bacterium to the surface. The predominant mode of transmission is percutaneous, although inhalation also occurs; it is not transmitted from person to person. Most Australians with melioidosis present with pneumonia, many are bacteraemic and about 25% present in septic shock. Even in Australia’s well-resourced health system, approximately 10% of people with melioidosis will die from their infection (here and here).
As almost everyone who develops melioidosis will require hospitalisation and prolonged antibiotic treatment, this year’s surge in case numbers has placed enormous pressure on local health services. Sadly, 11% have died from their infection.
What could be driving this season’s increase?
Over 90% of the cases have occurred in residents of central or southern Cairns, but an absence of distinct clustering has made investigation challenging. A complex interplay of population, pathogen and environmental factors is likely to be contributing.
The population
Between 2016 and 2024, the population of Cairns has grown by 10% and much of this growth has been in the southern suburbs of Cairns. This population growth would not, by itself, be sufficient to explain the disproportionate rise in cases this season. However, previous research has linked melioidosis increases to land disturbance, including the construction of a motorway in southern Cairns (here and here). It is possible that ongoing expansion of the rural–urban fringe in Cairns to accommodate this population growth isleading to increased human exposure to B. pseudomallei.
About 85% of melioidosis cases in Australia occur in individuals who have a predisposing health condition, most commonly diabetes mellitus, hazardous alcohol use, chronic lung disease, chronic kidney disease, immunosuppression or malignancy (here and here). Aboriginal and Torres Strait Islander people are disproportionately affected due to the social determinants of health. This season, the proportion of cases with a predisposing risk factor has been similar to previous years, although underlying chronic lung disease has been present in more cases (35% versus 22% in prior wet seasons). Pneumonia has been a more frequent presentation (92% versus 77% in prior wet seasons), suggesting that inhalation has been a more common mode of infection this season.
Occupational and recreational activities such as pressure hosing, gardening and walking barefoot are thought to increase the risk of infection. However, only around a fifth of cases this year can recall a clear exposure event suggesting that changes in human activity and behaviour are unlikely to explain the current increase in cases.
The pathogen
B. pseudomallei has a variety of virulence factors that are linked to tissue invasion and which play an important role in pathogenesis (here and here). Whole genome sequencing (WGS) has been used to define the sequence types (STs) in investigations of outbreaks of melioidosis and to analyse the geographic distribution of the organism (here and here). In one recent outbreak affecting seven children at a school in Cairns, three distinct STs were identified in the children and six other STs were identified in the local environment. It is therefore notable that 26/53 (49%) of the isolates to be sequenced from the 2024–25 wet season so far have been identified as a single ST (ST 70). The significance of this finding is uncertain, as previous Australian research has not demonstrated any differences in the virulence of different STs, but it is an ongoing area of investigation.
The environment
Heavier rainfall is linked to a greater number of cases of melioidosis (here and here). However, while the presentation of cases of melioidosis in Cairns this year is correlated with recent rainfall, the total cumulative rainfall in the December 2024 to March 2025 period has not been exceptional (1147 mm versus a historical mean of 1454 mm), and unlike Townsville, Cairns has not experienced flooding this wet season. It may be that other characteristics of the rainfall (such as the intervals between downpours) or the interaction with other climatic factors (such as windspeed) are contributing. Another hypothesis is that the rainfall and flooding associated with Cyclones Jasper and Kirrily in the previous 2023–24 wet season may have brought B. pseudomallei closer to the surface, increasing the likelihood of exposure this season. The interplay between environmental factors and the presence of B. pseudomallei in the local soils is also a focus of ongoing research. Many anticipate that climate change will increase the future incidence of melioidosis, but its contribution to the current spike in cases in Cairns is uncertain.
Will this be the new normal?
It is uncertain if this spike in cases is a unique event or whether this will be the new normal. The current case reporting system is being enhanced to ask additional questions about behaviours and environmental exposures. Ensuring that Aboriginal and Torres Strait Islander communities who are disproportionately affected have input into data collection methods is crucial to understanding and addressing disparities in disease burden. WGS of all the isolates will help identify any correlation between the different STs in this outbreak and the cases’ location and clinical presentation. WGS of stored isolates is also planned to determine the temporospatial epidemiology of STs in the region. Detailed analysis of the distribution of B. pseudomallei in the different soils in the region, particularly in areas with a higher incidence is important. Determining the impact of climatic factors on bacterial proliferation and local dissemination is also essential.
The future
Public health messaging needs to target those at most risk, particularly individuals with predisposing comorbidities in central and southern Cairns, to ensure that they can put prevention measures in place and recognise the manifestations of melioidosis to present for early medical review. The much higher incidence of melioidosis in First Nations peoples highlights the need for culturally considered, co-designed prevention and education campaigns. Local hospitals and health services must anticipate and plan for a greater number of cases, including for the effects on local sepsis pathways and the seasonal increased demand for outpatient antibiotic therapy programs. With the Cairns population expected to grow by 70 000 people by 2050, strategies to mitigate soil disruption should be incorporated into plans for urban development.
Conclusion
The steep increase in the number of cases of melioidosis in Cairns this wet season highlights the complex interplay between population, pathogen and environment that drives the incidence of many infectious diseases. Ongoing multidisciplinary investigations will determine whether this striking spike in cases of this potentially fatal infection represents an anomaly or an ominous sign of things to come.
Jacqueline Murdoch is a public health physician and GP, and the Director of Tropical Public Health Services in the Cairns and Hinterland Hospital and Health Service.
Josh Hanson is a general and infectious diseases physician based in Cairns, Australia. He is interested in the clinical management of infectious diseases in resource poor and remote settings.
Simon Smith is an infectious diseases and general medicine physician at Cairns Hospital.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Apologies for the late response but being UK-based these days I have only just stumbled aross this! The thing that would concern me about this dramatic increase is the possibility of a single source outbreak such as that which occurred in the USA in 2021 and was linked to an imported aromatherapy spray (https://www.nejm.org/doi/full/10.1056/NEJMoa2116130), particularly as almost half of these cases have been caused by a single sequence type. It would be very difficult to pick this up in an area that is already melioidosis-endemic (unlike most of the USA), especially if it was linked to a product that is very widely used. I have no doubt that the public health authorities in Cairns will have investigated this but just thought the possibility worth raising.
Great question! Primary care, especially continuity-of-care, could make a tremendous difference to vulnerability.
Indeed, it seems like an obvious question and as these patients come to diagnosis and management in the public hospital system, access to their MyHealthRecord in the process of providing that care can easily support identification of their GP and the existence (or absence) of GP Management Plans, Team Care Arrangements, Health Assessments and so on.
https://jamanetwork.com/journals/jama/article-abstract/2806025
https://www.health.nsw.gov.au/lumos/Pages/lumos-high-connectivity-cba.aspx
My thanks to the authors for raising this question. As 85% of melioidosis cases in Australia occur in individuals who have a predisposing health condition, most commonly diabetes mellitus, hazardous alcohol use, chronic lung disease, chronic kidney disease, immunosuppression or malignancy, it is curious that no-one has asked how many had current GP Management Plans. No-one has asked whether the primary care services in ever-expanding suburbs are adequate for need. No-one has asked if those individuals with predisposing health conditions had secured the continuity of primary care necessary to reduce their physical vulnerability to B. pseudomallei stirred up in their environment. Why not?