Emerging evidence suggests isotretinoin could cause permanent changes to the tear film of patients, even after stopping the medication.
Since the 1980s, Australian dermatologists have commonly prescribed isotretinoin for the treatment of acne and several skin conditions. Although literature for health professionals states that eye issues associated with isotretinoin use are uncommon, isotretinoin use frequently induces dry eye disease (DED), which can cause significant ocular morbidity and substantially reduce quality of life. Therefore, there is a need for increased awareness about isotretinoin-induced DED.
What is dry eye disease?
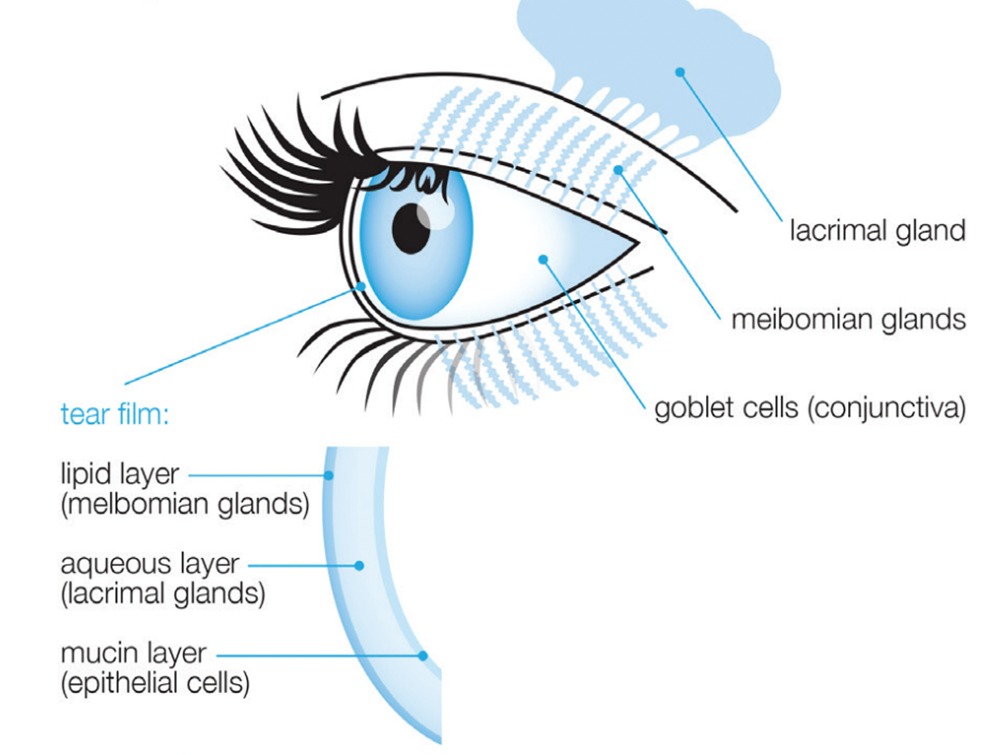
DED is a multifactorial disease affecting the ocular surface, typically involving tear film instability, lacrimal gland dysfunction, meibomian gland (MG) dysfunction, and/or inflammation of the eyelids (blepharitis). The tear film is composed of three layers: lipids produced by meibomian glands, the aqueous layer produced by lacrimal and accessory glands, and mucin (see Figure 1). DED commonly manifests as either a reduction in tear volume (aqueous dry eye), tear quality (evaporative dry eye) or both (mixed dry eye). In MG dysfunction, tear quality is reduced due to the relative reduction in the tear film lipid layer, which creates tear film instability and causes tears to evaporate too quickly.
What does dry eye disease look like?
DED may cause a wide range of ocular symptoms including fluctuating or blurred vision, redness, dryness, discomfort, itching, stinging, burning, pain, light sensitivity and foreign body sensation. These symptoms can significantly impact patients’ quality of life and are associated with depression and suicidal ideation.
85% of Australians reported experiencing symptoms of DED in 2022. With a high prevalence and severe adverse effects that threaten both sight and mental health, DED poses a significant health burden.
The effect of isotretinoin use on DED
A cross-sectional study found that 83% of isotretinoin users reported experiencing dry eye after commencing isotretinoin treatment.
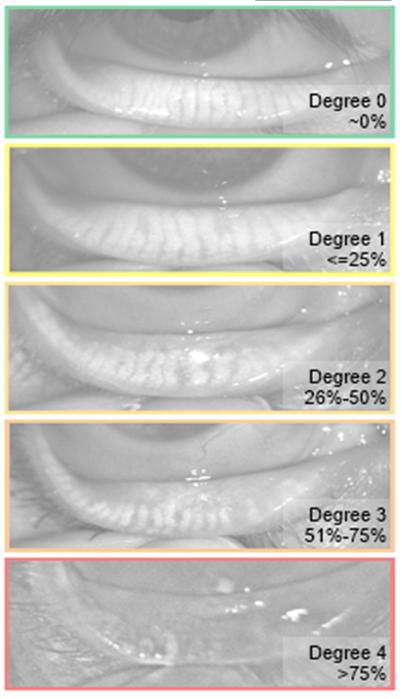
The most marked feature of isotretinoin associated dry eye is the reduction in function and atrophy of meibomian glands. An interventional study demonstrated that isotretinoin use led to a median meibomian gland loss of 34% during treatment (Figure 2). Translational research has demonstrated that isotretinoin decreases MG epithelial cell proliferation, inhibits lipid synthesis and induces MG cell death. The reduction in the tear film lipid layer leads to tear film instability and the development of evaporative DED.
While some studies suggest that the MG dysfunction in isotretinoin-induced DED is reversible on treatment cessation, in practice we are seeing an increasing number of dry eye patients presenting with permanent MG dysfunction several years after isotretinoin treatment cessation. Clinical cases have noted permanently decreased secretory function in the MGs of such patients, even in those with mild structural changes in their MG morphology.
In our practice, we have also observed a number of cases of permanent structural changes in MG morphology in patients presenting with dry eye several years after discontinuing isotretinoin therapy. Meibography imaging in Figures 3 and 4 demonstrate the permanent structural changes commonly seen in these patients relative to the scale provided in Figure 2.
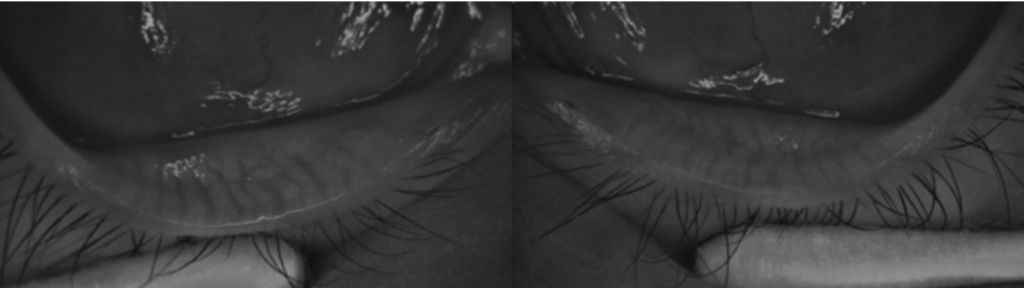
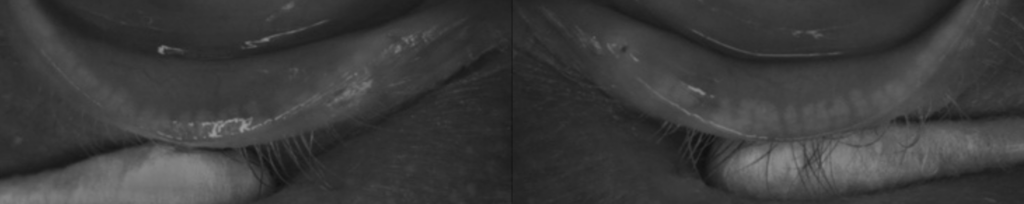
The discrepancy between research and practice suggests that MG changes in isotretinoin-induced DED are not reversible after treatment cessation. Information on isotretinoin’s long-term ocular effects is incomplete and further research is necessary to gain a better understanding of the reversibility of isotretinoin’s effects.
Key points in isotretinoin prescription
The prevalence of DED in Australians is continuing to rise. As isotretinoin has been on the market for several decades now, it is likely that we are now seeing the long-term effects of isotretinoin use beginning to emerge. The following recommendations intend to provide an interdisciplinary approach to minimising the burden of isotretinoin-induced DED:
- Medical practitioners should adequately inform isotretinoin users about the risk of DED.
- Key risk factors for DED to look out for before initiating isotretinoin: contact lens wearer, medications that reduce tear volume (antihistamines, antidepressants, diuretics), post-menopausal women, previously undergone/intend to undergo refractive surgery, connective tissue diseases (eg, Sjögren syndrome).
- Referring patients at risk of DED to a dry eye clinic or an optometrist with an interest in dry eye for baseline assessment including meibography prior to commencing isotretinoin therapy, with ongoing monitoring during treatment.
- Medical practitioners should consider a history of previous isotretinoin use in patients presenting with DED symptoms. Consider onwards referral to a dry eye clinic for treatment options targeting MG dysfunction such as intense pulsed light (IPL), and other topical therapies.
Beyas Basu is a first year medical student at Griffith University.
Dr Madeleine Adams is an experienced ophthalmologist specialising in cataract and lens surgery. She is the director of Insight Eye Surgery, located in Brisbane and Noosa.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
in 2022 85% of Australians experienced dry eye, yet only 83% of people using isotretinoin experience dry eyes – is it protective!
Really insightful article! Important to raise awareness about the potential complications of such a common medication.