The health system needs to take an ‘all hands on deck’ approach to ensure at-risk people in aged care communities have prompt access to vaccination, testing and treatment for COVID-19.
In 2024, hundreds of Australians are still dying from COVID-19, especially at-risk vulnerable elderly people in aged care facilities (ACFs). Indeed, in the three month periods leading up to July 2023 and July 2024, there were very similar numbers of deaths in ACFs from COVID-19: the total for 3 May to 26 July 2024 was 442 deaths, compared to the similar period, 5 May to 27 July 2023, with 439 deaths.
Looking at the wider graph of COVID-19 deaths in aged care facilities (below), we see the ongoing issue of deaths in aged care facilities, while deaths in the broader community have declined considerably.
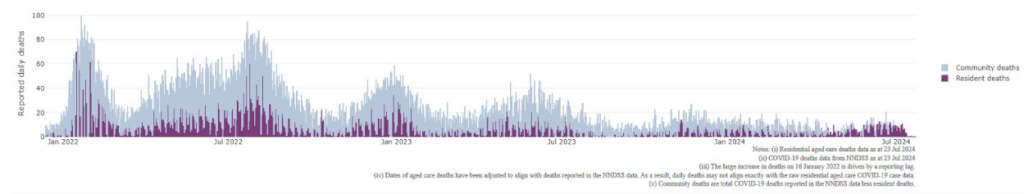
Covid deaths in residential aged care overlaid with community deaths (source).
In Australia, around 1000 COVID-19 deaths were recorded each year in 2020 and 2021, but, after opening up, at least 12 000 perished during 2022. Several thousand died in 2023, when the “milder” Omicron strains dominated in a new period of increased mixing and much-reduced social distancing.
In 2023, when the Public Health Emergency of International Concern (PHEIC) was rescinded, the WHO director stated that there remained significant ongoing concerns regarding COVID 19 deaths and disease.
So, what is going wrong in our aged care facilities? Why aren’t we winning the war on COVID-19? In one recent July week, there were about 400 active outbreaks, with 2000 infected residents.
Once again, we need closer attention to infection control. High quality non-pharmaceutical interventions make a difference and are essential in aged care and other closed community settings to ameliorate virus spread. In addition, disappointedly, only about 44% of aged care residents (aged 75+ years) have had the recommended COVID booster in the past 6 months and many infected people are not getting a COVID anti-viral drug early enough.
We have a near perfect storm creating an ongoing high death rate in ACFs.

Molnupiravir (Lagevrio) — named after the hammer of the Norse god, Thor — has been most prescribed (around 128 000 times), while Paxlovid has been prescribed 10 times fewer.
But following the declarations of the National Clinical Evidence Taskforce, molnupiravir is now considered second-line (albeit still useful). In short, it is deemed less effective than Paxlovid (Nirmatrelvir/ritonavir) — what might be called the “peace and love” drug — in preventing severe disease.
GPs face the difficult task of determining if a COVID-test-positive vulnerable ACF resident, with multiple medical problems, should take Molnupiravir or Paxlovid while also being treated with other essential medications. It requires skill, but we believe it is time well spent to ensure the at-risk have optimal treatment to reduce the risk of complications further down the line. Research suggests a high level of protection from use of Paxlovid in preventing severe COVID-19.
The major impediment to widespread use of Paxlovid has been concern over drug–drug interactions where the body’s blood level of other important drugs (for example, antidepressants, antipsychotics, anti-arrhythmics, some statins, and anticoagulants) may be seriously altered by taking Paxlovid, but not impaired by using Molnupiravir.
Paxlovid is widely available in Australia but has been used sparingly. The health system needs, again, to take an “all hands on deck” approach to ensure at-risk people in aged care communities have prompt access to vaccination, testing and treatment and that non-pharmaceutical interventions, including rapid antigen tests (RATs) for staff and visitors, are effectively implemented; that means better supporting GPs and better educating patients, relatives and aged care staff on the recommended approaches.
While we have been generally successful in the war on COVID-19 in Australia, doctors on the ground know that the war on COVID-19 is not over yet. A brief survey of six GPs revealed all have ongoing concerns and all endeavour to prescribe the most effective anti-viral treatment based on online guides like the Liverpool Tracker. The war on COVID-19 continues and we need to break the stalemate of so many vulnerable elderly still perishing.
We also know we must now prepare for the next pandemic, which is likely to be a novel influenza or coronavirus.
As Winston Churchill said: “If you wish for peace, prepare for war.”
Professor Booy is a clinical epidemiologist and an honorary professor at the University of Sydney. Professor Gary Grohmann is a consultant virologist and adjunct professor at the University of Sydney. Prof Booy wishes to pay tribute to the PhD student Christian Jones who worked diligently and intelligently on the prevention of respiratory outbreaks in aged care facilities. We are grateful to Jennifer Watts for epidemiological assistance.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
It would be great if there was more public health awareness in the community as well. Surely keeping levels of COVID (as with the same precautions a number of respiratory diseases including influenza and RSV) down in the community would have a flow on of less getting into aged care as well? It seems that everything we learned during COVID has been thrown out the window. We know that wearing masks in some situations are beneficial for everyone. We know the importance of hand and respiratory hygiene. We know that it’s important people who are sick stay home as much as possible and wear a mask if they have to go out. I’m not sure why encouraging the general public to take an active role in protecting themselves and everyone else has become a dirty concept now.