In part one of this series on health system reform, Associate Professors Cate Kelly and Doug Johnson from the Department of Medicine at the University of Melbourne discuss the need for a person-centred health care system …
After many years of working in the Australian health care system, we believe more can be done to implement meaningful, sustainable health care reform.
In this article, we propose ways in which health system reform could be approached that deliver integrated, person-centred care.
Although some principles of a person-centred system are already in place, or partially or fully agreed in the National Health Reform Agreement, a number of principles are not in place. These should be further considered along with mechanisms to deliberately integrate processes across the system to reduce fragmentation – a source of clinical risk, frustration and delays to care delivery.
Much has been written in the past 12 months about the challenges currently facing the Australian health system (here and here). We believe the outstanding, and widely supported, model of universal health care is wobbling, despite 10% of Australia’s gross domestic product being spent on health care services.

The system is facing pressure from multiple issues including:
- increasing workforce and capacity challenges;
- an ageing, multimorbid population; and
- fragmented and poorly coordinated health care (here, here and here).
Across Australia, it seems there is appetite for reform. Significant reform proposals and activities are under way at both a state and federal level (such as the Strengthening Medicare Taskforce).
The Taskforce is critical, but much of it is focused on individual sectors (eg, disability, aged care or primary care), which we believe creates the risk of perpetuating fragmentation. This in turn creates additional clinical risk, workforce and user frustration, additional costs, and delays to accessing timely care (see here, here, here and here).
What is less evident is an overarching vision and plan for the Australian health system as a whole which considers the challenges and opportunities of these different sectors, the experience of their users, and the interfaces between the different sectors.

The deeply interconnected nature of our health system and related sectors demands an overarching, integrated vision of how these components work effectively together to:
- ensure clinical risks driven by system fragmentation are optimally identified and managed;
- minimise the chance of competing activity or activity that pulls in different directions, and as a result is less effective; and
- avoid creating health system “whack-a-mole” where one component of the system is improved, only for it to have downstream impacts on other sectors.
An overarching approach and vision are important: in the absence of a map, how will we know where we are going or when we get there? In addition, how will we ensure we are successfully achieving improvements without agreement on what that success looks like?
The authors propose that the health system vision and strategy, as well as key underpinning processes and documents are reviewed to ensure they:
- overtly address fragmentation;
- consider common and high risk interface challenges and ways to address these; and
- are both person- and workforce-centred.
What would a truly person-centred health system look like?
A person-centred health system
Person-centred care is an essential element for the delivery of high quality care.
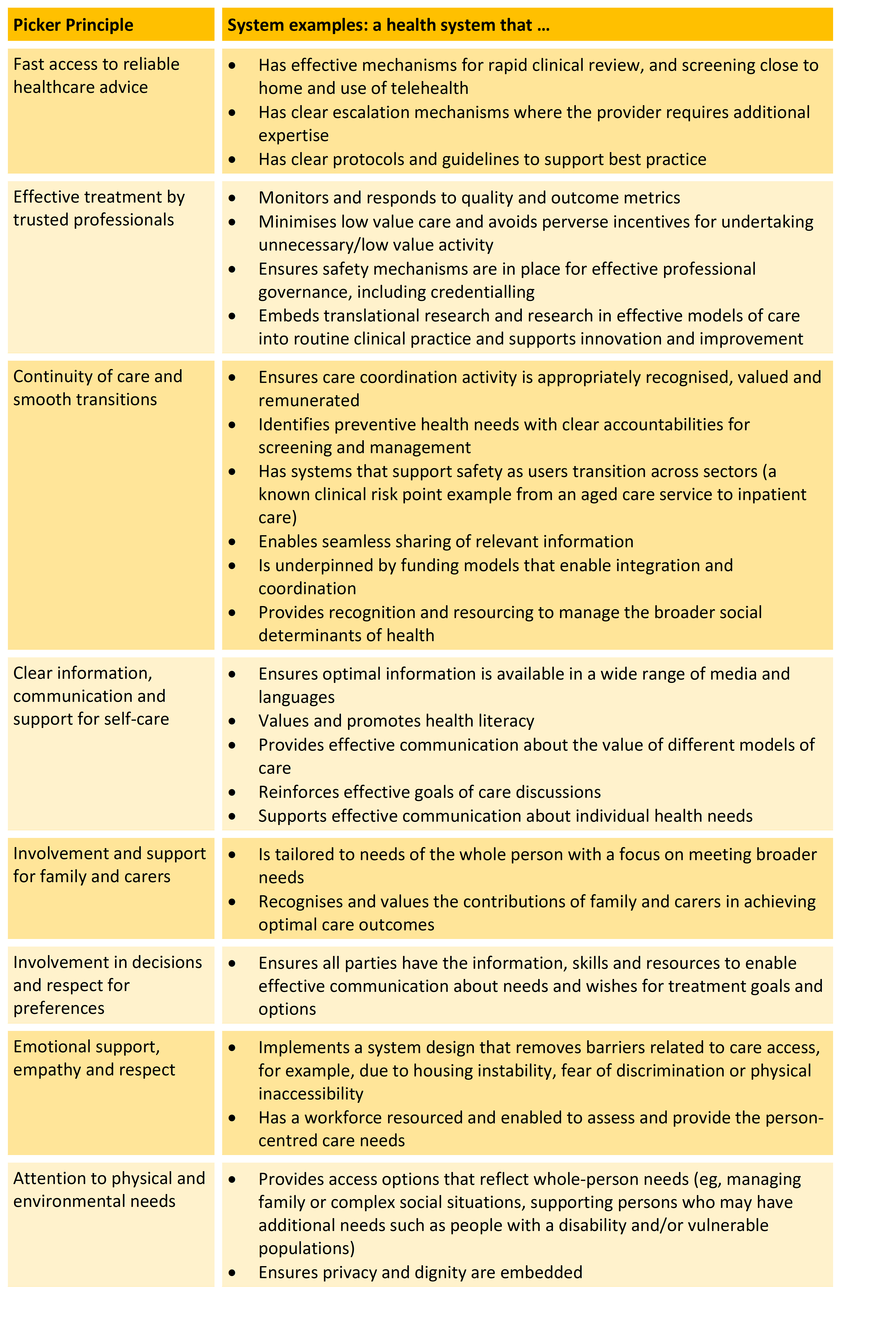
The Picker Principles have been widely adopted as supporting meaningful person-centred care and we support the adoption of these principles when considering health system reform.
The National Health Reform Agreement articulates action on a number of these points, but we believe more could be done to ensure a shared, person-centred vision for our health care system.
Using the Picker Principles, we have developed the following possible system examples.
We believe ongoing health care reform is required to deliver an integrated health system that spans preventive health, primary care, hospital medicine as well as related sectors such as disability, community health, public health and residential aged care.
A person-centered approach to reform, that also explicitly addresses fragmentation, is essential to ensure patients and their families remain our primary focus.
However, reform cannot be achieved without also considering the most essential aspect of health care service delivery: our workforce, which we will discuss next week in part two of this series.
Associate Professor Cate Kelly is a Board Director, Health Care Consultant and an Honorary Clinical Associate Professor at the Department of Medicine at The University of Melbourne.
Associate Professor Douglas Johnson is the Director of General Medicine, Medical Services at the Royal Melbourne Hospital and an infectious diseases and general medical physician.
Read InSight+ next week when Associate Professors Kelly and Johnson will discuss the what considerations are required to deliver workforce-centered reform of our health care system.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
One of the major problems we face with medical care in Australia is that Medicare subsidises almost every medical consultation and procedure.
Medicare is a monopoly. Until the Monopoly is broken down the system will never improve.
Thank you for this crucial article. I was pleased to read that one of the co-authors is a general physician – a rare breed in many hospitals. Having spent my life in a generalist hospital specialty (emergency medicine), I have been increasingly frustrated on behalf of patients by the worsening sub-specialisation and silo-ing of hospital departments – especially inpatient medicine. It is paradoxical that, as patients become more complex and have more and more multi-system issues, medical departments are becoming more narrow and risk-averse. This is the inverse of what patients need – instead of designing services to suit the needs of patients, we are trying to shoe-horn patients into unsuitable services, who control their walls tightly and do their best to exclude risk from their service.
This is highly frustrating – and demeaning – for ED clinicians who have to battle with various teams trying not to admit the 74 yr old with COPD, heart failure and a chest infection – too young for Aged Care, too respiratory for Cardiology, too Cardiology for respiratory, “have you excluded PE”, “have you done a CT?”
Hospital silos are not only professional in nature – they are risk silos. Each team wants to exclude the patients who need the most complex thinking and planning, or just good general care.
And the loud, aggressive elderly patient with dementia who hit another resident so the RACF “won’t take them back”, delirium screen negative, where are they to go? Just let ED hang on to them, shouting, while, around them, children are crying and frail elderly are dying? Do we only care if it is our own relative being treated like this?
Thanks for an excellent article. The table develop based on the “Picker Principles” is spot on. It is also lamentable how far we are from what is optimal. Wide ranging reform, not just trimming around the edges is required. And while considering reform let’s tackle root causes of multimorbidity and strengthen population based strategies to optimise health and reduce chronic disease burden. This needs to include strategies to foster optimal health literacy, health competence, and capacity for self management. Social determinants of chronic disease disparities also need to be addressed.
A lot of money is spent on chronic care plan development with, to my knowledge, no good evidence the lead to better outcomes. The ones I have read are woeful for the most part, and generic rather than person centred.
Maybe it’s time for a much broader conversation about delivery of cost effective primary care, however confronting that may be.
There is no doubt that the current fear of AHPRA is detrimentally affecting the ability to deliver healthcare to patients. Whilst it is reasonable to expect doctors to have the intelligence not to behave indiscriminately, the fear of being falsely accused of sexual misconduct is a very significant deterrent to performing a proper examination. Vexatious complaints are encouraged. Doctors rights as patients hold no place in AHPRA’s persecutions.
Unfortunately, whilst medical indemnity insurance is compulsory, medical indemnity businesses are more interested in profit than protecting the reputation of their members against AHPRA.
Similarly, it is difficult to stop lawyers from pursuing a medical negligence case when they get a sniff of victory, knowing that medical indemnity businesses will settle out of court!
Where AHPRA is again caught out, they use their unlawful activities as an excuse to grab for more power!
For the sake of medicine, something has to change.
The first step is for the powers that be to acknowledge that AHPRA, lawyers, and medical indemnity businesses are not operating in the best interests of healthcare.