Australian research into new biomarkers to detect skin cancer has been welcomed by the Australasian College of Dermatologists, but the shortage of dermatologists means some early skin cancer diagnosis work is currently falling to general practitioners.
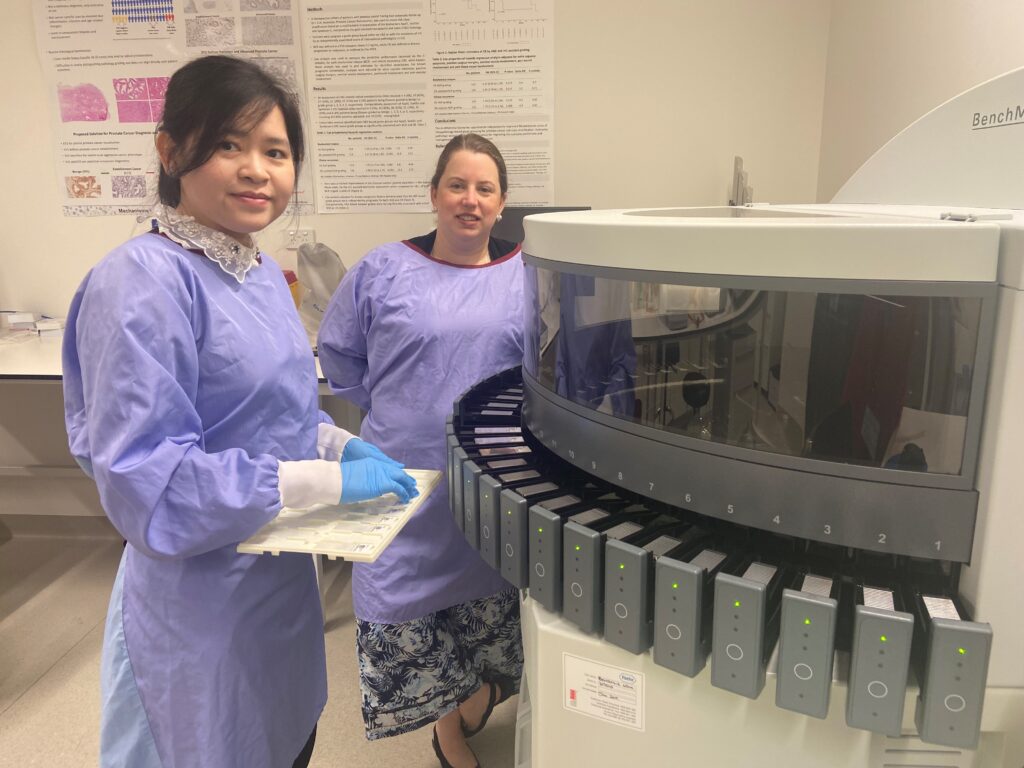
Two Adelaide researchers are fast-tracking research into new biomarkers for melanoma detection to improve early diagnosis, telling InSight+ current biomarkers used by clinicians are “less than perfect”.
The research, being conducted at the University of South Australia, aims to develop more effective biomarkers for melanoma and increase understanding of how the disease progresses.
“The ultimate aim of our biomarker program is to develop sensitive and specific biomarkers that can reliably inform the primary pathogenesis of the disease,” University of South Australia Research Fellow Dr Jessica Logan and PhD Candidate Giang Thuy Lam told InSight+.
“We hope that our biomarkers can be widely adopted in clinical settings not only to aid in diagnosis/prognosis, but also to assist clinicians on decisions for therapeutic intervention to enhance patient outcomes.”
Dr Logan and Ms Lam said many current biomarkers used to diagnose skin cancer can be ineffective, leading to skin cancers being missed.
“Alarmingly, most research discovery programs are not focused on the underlying pathophysiology of the cancer and only yield cell differentiation, inflammatory or other biomarkers that report on secondary mechanisms and not the primary pathogenesis of the cancer,” they said.
“Consequently, biomarkers currently being utilised in clinic for skin cancer are less than perfect. Some of the common markers SOX10, HMB-45, Melan-A and MITF are unable to achieve consistency, thus still suffer limitations.
“None of the immunohistochemistry markers currently used in regular pathology practice can consistently differentiate melanomas from benign melanocytic lesions, thus their adoption across pathology practice is not standardised.”
The researchers hope that new biomarkers can be in use within three years, ultimately helping doctors provide a quicker diagnosis for their patients.
“We will be translating a panel of biomarkers into clinical practice over the next few years,” they said.
“These biomarkers aim to assist in the accurate diagnosis of melanoma, distinguishing this cancer from other benign lesions. This will ensure we provide clinicians with the tools and knowledge to affect a timely, accurate diagnosis which will then facilitate personalised medicine approaches for melanoma patients.”
The new research has been welcomed by the Australasian College of Dermatologists, which told InSight+ there are no biomarkers that are in common clinical use for diagnosing melanoma.
“Additional measures to help in the accurate diagnosis of early melanoma are of great interest and importance,” College President Dr Clare Tait said in an interview.
“Despite advances in clinical and laboratory methods, [detecting melanoma] remains a constant challenge.”
Dr Tait said GPs in Australia are under increasing pressure to detect skin cancers in patients due to the shortage of dermatologists at public and private dermatology clinics.
“There is a nationwide shortage of dermatologists and, [along] with all medical workforce challenges, this affects rural remote and regional areas the most,” Dr Tait said. “[The shortage] will also have a disproportionate effect on our First Nations communities.”
She said long waiting lists in public and private dermatology services have had a negative effect on patient care, resulting in later diagnoses.
“This puts pressure on all doctors involved in the diagnosis and treatment of melanoma, including GPs,” she said.
A Canberra patient with melanoma, John Paine, gave InSight+ permission to share his difficulty in trying to find a local dermatologist.
“I have been diagnosed with several melanomas, but I have had to travel to Sydney for melanoma treatment and removal,” Mr Paine said in an interview.
“My local GP has told me there is no point trying to refer me to a dermatologist in Canberra because the wait times are dangerously long.
“Therefore, many Canberra patients including me have to make the 300 km journey to Sydney to see a specialist.
“My local GP is concerned that he may miss a melanoma on my skin, so they need that specialist input to avoid the cancer metastasising and taking hold.”
The Australasian College of Dermatologists’ White Paper, published in November 2022, explains a number of strategies to address the shortage of dermatologists, including a specialist training program being piloted in Townsville and Darwin.
The Australian Government is funding the pilot, which was awarded under the Flexible Approach to Training in Expanded Setting program. It involves teaching dermatology trainees while also providing local communities with access to specialist care.
The College said in a statement it had also been successful in gaining funding for five additional registrar positions through the Australian Government-funded Specialist Training Program from 2024.
“Specifically, this funding must support training in regional and rural areas,” the College said.
“This is a step in the right direction to address capacity and is the largest single increase to our allocation since the inception of the Specialist Training Program a decade ago.
“While we still have a long way to go to solve the workforce shortage, this will contribute to the dermatologist pipeline in the coming years and help to build training and services outside of metropolitan centres,” the College said.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert
I think it would be better to train GPs to be more confident in diagnosing and treating early skin cancer, rather than relying on specialist dermatologists, who, as the authors state, are thin on the ground.