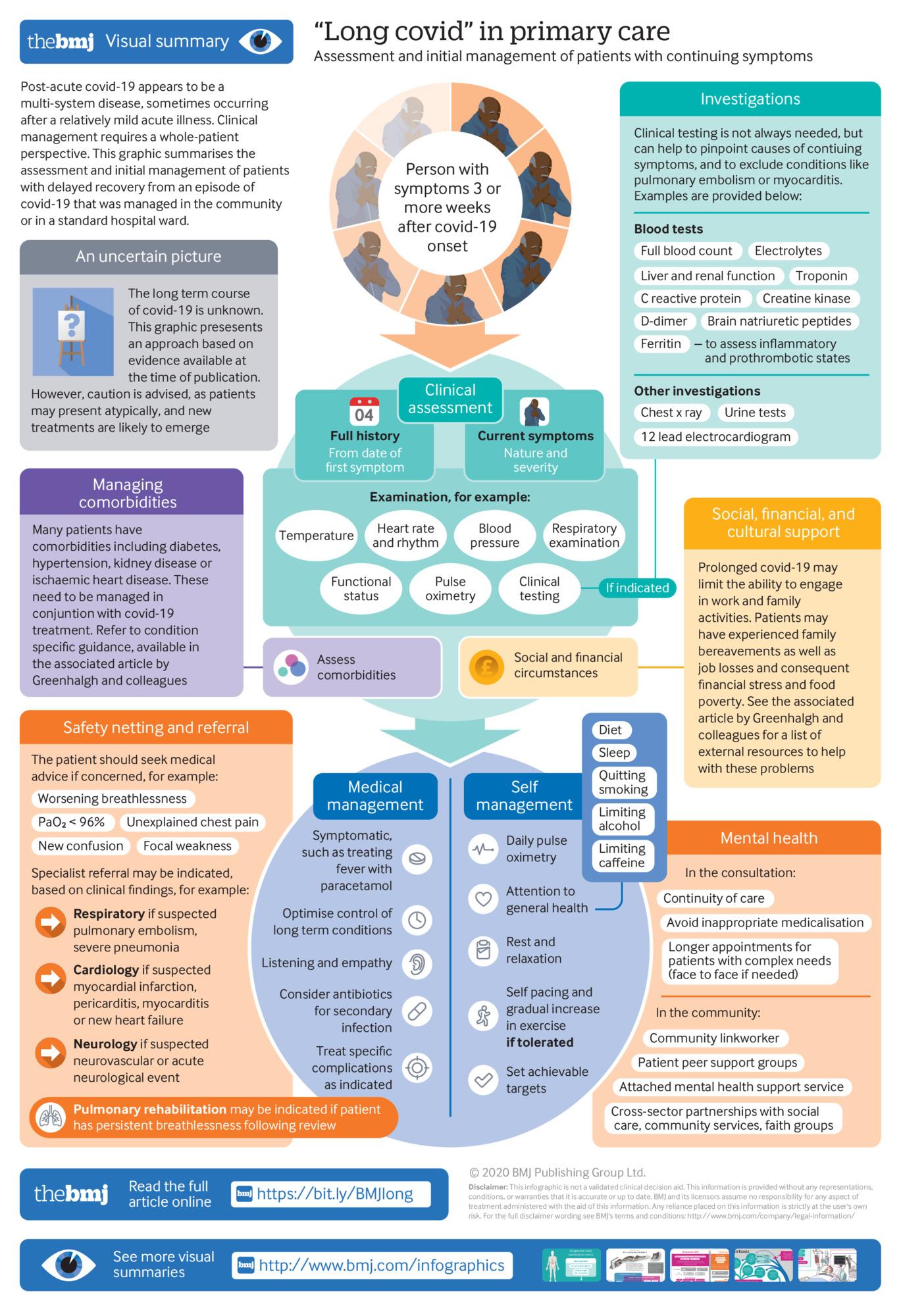
A TEAM led by Professor Trish Greenhalgh, Professor of Primary Care Health Sciences at the Nuffield Department of Primary Care Health Sciences at the University of Oxford, has produced a guide for primary care practitioners on the care of patients with long COVID, published in the BMJ.
The article includes definitions, case studies, testing requirements, recommendations for respiratory symptoms and support, pulse oximetry, fatigue, cardiovascular complications, assessment and management, social and cultural considerations, and a long list of resources for GPs with patients with long COVID.
There is also a podcast with Professor Greenhalgh available here.
Good news for LiveLighter obesity prevention campaign
A cost-effectiveness analysis of the Western Australian LiveLighter program, published in PLOS ONE, has found it is “likely to represent very good value-for-money as an obesity prevention intervention in [WA] and should be included as part of an evidence-based obesity prevention strategy”. LiveLighter in WA has implemented a series of mass media advertising campaigns aiming to change adult behaviour around achieving and maintaining a healthy weight. “From 2012–2019, seven television-led phases of the LiveLighter campaign, each targeting different aspects of unhealthy behaviour and the associated health impact, have aired over 22 campaign periods in WA,” wrote the authors from Deakin University, Cancer Council WA, and Cancer Council Victoria. “The LiveLighter mass media campaign has also been licensed for use in other Australian states. Studies that evaluated the effectiveness of the Sugary Drinks phase of the LiveLighter campaign in the states of Victoria and WA showed significant reductions in the frequency of sugary drinks consumption after the campaign.” The 12-month intervention was estimated to cost approximately $2.46 million. The meta-analysis indicated post-campaign weekly reduction in sugary drinks consumption of 0.78 serves (95% uncertainty interval [UI], 0.57–1.0) and sweet food of 0.28 serves (95% UI, 0.07–0.48), which was modelled to result in average weight reduction of 0.58 kg (95%UI, 0.31–0.92), 204 health-adjusted life years (HALYs) gained (95%UI, 103–334), and health care cost-savings of $3.17 million (95%UI, $1.66 million to $5.03 million). The mean incremental cost-effectiveness ratio showed that LiveLighter was dominant (cost-saving and health promoting; 95%UI, dominant; $7703 per HALY gained). The intervention remained cost-effective in all sensitivity analyses conducted.
Pregnancy and perinatal guidelines from National COVID-19 Taskforce
The National COVID-19 Clinical Evidence Taskforce has updated its pregnancy and perinatal guidelines, with a summary published in the MJA. “As of May 2022, the Taskforce has made seven specific recommendations on care for pregnant women and those who have recently given birth. This includes supporting usual practices for the mode of birth, umbilical cord clamping, skin-to-skin contact, breastfeeding, rooming-in, and using antenatal corticosteroids and magnesium sulfate as clinically indicated. There are 11 recommendations for COVID-19-specific treatments, including conditional recommendations for using remdesivir, tocilizumab and sotrovimab. Finally, there are recommendations not to use several disease-modifying treatments for the treatment of COVID-19, including hydroxychloroquine and ivermectin. The recommendations are continually updated to reflect new evidence, and the most up-to-date guidance is available online.”
COVID-19-related distress in Australian rural settings
Western Sydney University research published on the preprint server MedRxiv reports links between high rates of distress among rural Australians during the COVID-19 pandemic, worsening lifestyles as measured by the Global Lifestyle Score (GLS) and loss of income. The research, which has not yet been peer-reviewed, involved a cross-sectional anonymous online survey that was distributed among adults in the Western New South Wales Primary Health Network in August 2020. The survey included measures of psychological distress, income, disposition, lifestyle factors and behaviour during the pandemic, as well as changes in lifestyle due to COVID-19. A novel GLS was generated as a holistic assessment of lifestyle across multiple domains. The survey was completed by 308 individuals (modal age group, 45–54 years old; 86.4% female). High distress on the K5 scale was present in over one-third of respondents (n = 98, 34.3%). Negative change was reported for sleep (24.4%), nutrition (14.3%), alcohol use (17.8%), physical exercise (33.8%), and smoking (26.6%) since the onset of the pandemic. Additionally, changes in sleep, nutrition, physical activity, and smoking were associated with distress. Respondents with a poor lifestyle (GLS) during the pandemic were significantly more distressed. Perceived COVID-19 impact was associated with high distress, level of drought impact, and loss of income.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert