THERE is an abundance of evidence that people with positive social health – where “social health” is defined as a person’s ability to adapt in social situations and form satisfying meaningful relationships, including how they interact with and are supported by other people – are at lower risk of developing serious chronic diseases and death.
Social isolation is an objective measure of the lack of social relationships or infrequent social contact with others. Social support is a subjective measure of how social contacts are used; it is the actual or perceived availability of resources from others. When discussed, “low” social support is preferential, as “lack” is a subjective interpretation by the researcher. Loneliness is a subjective negative feeling of being isolated or lacking support.
There are a range of systematic reviews demonstrating that people with positive social health are at lower risk of developing coronary heart disease and stroke by around 30%, dementia by between 28% and 59%, depending on the measure (here, and here), and death by between 26% and 32%, depending on the individual measure. The World Health Organization recognises that “social isolation and loneliness dramatically affect older adults’ mental and physical health”.
We know that positive social health, using a range of different measures, predicts better health and greater survival. The challenge now lies in determining which social health construct has the greatest implications for health and wellbeing.
Do you see or hear from at least four friends and relatives in a month? Do you have at least four relatives or friends that you feel close to or can rely on? Do you participate in community or group activities at least once a month? Do you feel lonely never or only sometimes (one or two days per week)?
These are examples of questions to measure social health, and it is shockingly dismal how many people answer “no”. I found that in a large sample of Australians aged 70 years and over, who were healthy and living in the community, 8% (n = 919) reported having poor social health. As the Australian Institute of Health and Welfare reported, before COVID-19 restrictions, one in four Australians were experiencing an episode of loneliness and one in 10 had low social support (page 47).
Historically, it has been somewhat acceptable to use the social health constructs interchangeably. More recently, social isolation, low social support and loneliness are being distinguished as distinct yet interconnected concepts, which should be assessed simultaneously (here, and here). Studies that do not distinguish between these concepts may not detect the effect on health (here, and here).
Furthermore, the combination of social health measures may have implications for health and wellbeing. It would make sense that someone who is not socially isolated, has high social support and is not lonely may have better mental and physical outcomes than someone who reports being negative on all three concepts (Figure 1).
Figure 1: A Venn diagram of social health combinations
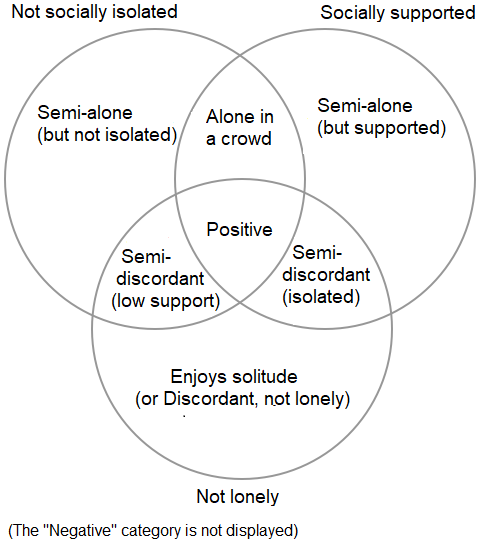
Information originally presented in Freak-Poli et al 2021
But what about different combinations of social health measures? For example, how about if someone with introvert tendencies enjoys their solitude, reports being socially isolated, and having low social support, but not being lonely? Or the reverse, when someone is surrounded by disconnected and unfulfilling relationships and feels lonely? The latter has been termed “alone in a crowd” and I often think of older people in nursing homes with few visitors; however, there are plenty of people of all ages who feel disconnected from those around them. Very little literature has assessed all three social health concepts simultaneously or in combination.
My colleagues and I tested the separation of social health concepts among 10 517 women aged 70–75 years from the Australian Longitudinal Study on Women’s Health in relation to health-related quality of life, which is defined as an individual’s self-perceived health status in relation to the social, cultural and environmental context.
We found that social isolation, low social support and loneliness were each independently associated with worse mental and physical quality of life. Loneliness had the strongest association with mental quality of life (– 10 units), followed by low social support (– 5) and social isolation (– 2). For physical quality of life, loneliness (– 2), low social support (– 2) and social isolation (– 1) were similar in their strength of association. As expected, we found that being positive on all three constructs was best, and being negative on all three was worst, for both mental and physical quality of life (Figure 2).
Figure 2: The association between social health combinations and health related quality of life
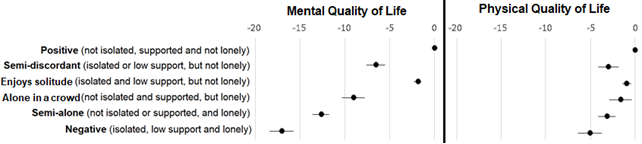
Information originally presented in Freak-Poli et al 2021. Magnitude of effects reported in unit coefficient. Adjusted for age, demographics, socio-economic position and comorbidity
What was interesting is that someone who might enjoy their solitude (socially isolated, low social support, but not lonely) had similar mental and physical quality of life scores to those who were positive on all three social health concepts. Also, I was surprised that people who were alone in a crowd (not socially isolated, high social support, but lonely) were disparate from people who reported being negative on all three concepts. This latter finding highlights the importance of the three social health concepts being assessed simultaneously, rather than loneliness by itself. While people in the negative and alone-in-a-crowd groups were both lonely, an intervention to improve social contacts and support may be more beneficial to the negative group.
Knowing the importance of assessing the social health concepts independently, we then wanted to have an in-depth look at chronic disease risk factors.
Among 11 498 healthy, Australians, aged 70 years and older, living in the community, and enrolled in the ASPirin in Reducing Events in the Elderly (ASPREE) clinical trial and the ASPREE Longitudinal Study of Older Persons (ALSOP) substudy, we assessed 12 cardiovascular disease risk factors outlined by the Heart Foundation of Australia. We found that those with positive social health were less likely to have multiple risk factors for heart disease, lowering their risk of having a heart attack or stroke within 10 years.
There was a slight difference by gender; loneliness (regardless of social isolation or social support) was more strongly associated with cardiovascular risk among women, whereas among men, being socially isolated or having low social support, in addition to loneliness, also mattered.
When looking at the 12 risk factors separately, those with positive social health (on any construct) tended to be more physically active and less likely to have depressive symptoms. There were additional associations with individual social health constructs. Among men and women, being aged closer to 70 years, rather than being older, was associated with lower loneliness. Not being a current smoker was associated with not being socially isolated or lonely among women, and high social support among men. Lower blood pressure was associated with not being social isolated among men and women, as well as high social support among women. Being a healthy weight was associated with not being social isolated among women, and not being lonely among men.
We have also found that social health plays a role in recovery after a cardiovascular disease event. We demonstrated through a thematic systematic review of 29 studies that positive social health measures were consistently associated with better mental health outcomes (lower depressive symptoms, anxiety symptoms and psychological distress) among cardiac patients. Two findings from this review surprised me – first, the limited studies devoted to women or gender-disaggregated findings, and second, that partner status and living status did not align with social isolation and social support findings. We recommend they may not be suitable as social health proxies.
Our findings are particularly concerning given that COVID-19 restrictions limit people’s interactions. Regardless of where you live, the COVID-19 disease pandemic has had a profound impact on society over a substantial amount of time. In Australia, COVID-19 restrictions have included enforced social distancing, quarantine, closure of recreation centres, and reduced activities for many people who would otherwise choose greater social engagement.
We know that poor social health is a precursor to mental ill-health and that COVID-19 restrictions have had adverse mental health implications.
Health professionals are placed in a position to intervene by identifying patients who have poor social health and offering community support programs (termed “social prescribing”). In fact, health professionals may already be, unconsciously or informally, incorporating social health into their decisions. However, asking about someone’s living situation and partner status is not enough. What matters is having regular social contact and whether someone feels connected and supported by their contacts. Even if health professionals cannot change their patients’ social circumstances, they could concentrate more on these high risk individuals’ chronic disease risk factors such as physical inactivity, smoking, and high blood pressure.
Dr Rosanne Freak-Poli is a life-course epidemiologist, and Heart Foundation Senior Research Fellow at Monash University.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert