A LEADING Sydney GP is calling for the relaxation of restrictions around access to human papillomavirus (HPV) swab self-collection after the MJA reported the case of a woman who was diagnosed with cervical adenocarcinoma after being screened using a self-collected sample.
The authors outlined the case of an asymptomatic 39-year-old woman, who had a female partner, and was many years overdue for cervical cancer screening.
After testing positive for HPV16 infection using a self-collected swab, the woman was referred for colposcopy and was subsequently found to have cervical adenocarcinoma with a depth of invasion of 3 mm. The woman underwent radical hysterectomy, bilateral salpingectomy and bilateral pelvic lymphadenectomy for the removal of stage 1b1 cervical adenocarcinoma. The authors reported that there were no signs of cancer recurrence after 6 months of follow-up.
The Australian National Cervical Screening Program introduced HPV testing in 2017. Self-collected samples are available as part of the program for women aged over 30 years who have never been screened or who are 2 or more years overdue for screening. Samples must be collected in a practitioner-supervised setting, not at home.
Dr Linda Mann, principal of an LGBTQI-friendly general practice in Sydney’s Inner West, said these restrictions were preventing many people from accessing screening.
“I have never successfully done [a self-collected screening test] because I have fallen foul of the bureaucracy every single time,” she said, adding that she continues to offer the test because she “wants it to work”.
“For me, as an ordinary GP, the rules make it such a difficult thing to collect. I do not understand that if a woman requests self-collection – whatever her circumstances – and she had a test that was okay 5 years ago, she is denied the opportunity.”
Dr Mann said the restrictions were initially introduced due to the uncertainty around the accuracy of specimens, but the MJA authors reported that the accuracy self-collected samples had been shown to be comparable to clinician-collected samples.
“So, what’s the problem?” Dr Mann asked. “They don’t want to screen people? Are they being prejudiced here? I just don’t get it.”
She cited one case in which a pathology service rejected a patient’s sample because the patient was just days shy of being 2 years overdue for screening.
“Of course, I have never screened that person since. She refuses,” Dr Mann said.
Dr Viv McGregor, LGBTIQ+ Sexual Health Clinic Co-ordinator at ACON, said GPs should be given more discretion to respond to the specific needs of their patients.
“Giving GPs the discretion to pick up on patients’ unique needs would be amazing for under-screened and never-screened people, and for people who keep up with regular screening but who find it incredibly difficult to do so. I think that would result in an incredible increase in people testing,” she said.
Dr McGregor welcomed the MJA case study, saying that it was important for such stories to be told in medical journals.
She said some people were still incorrectly being told by health professionals that they were not at risk of HPV and did not require screening.
“We have evidence that a lot of medical professionals have – either in the past or even now – told women who have sex with women or trans men who have sex with women and non-binary people who have sex with women that they don’t need cervical screening,” Dr McGregor said, noting that HPV testing was also relatively new in Australia.
She said that many members of the LGBTQI community also relied on each other, rather than mainstream public health messaging, for health information, so misinformation could quickly be spread through the community.
Dr McGregor, who also co-ordinates ACON’s Digital Engagement & LGBTIQ Health programs, said there were also a range of barriers to cisgender lesbian women and trans and gender diverse people accessing cervical screening.
“A lot of people in our community have had very negative experiences with health care,” she said.
“It can [come in the form of microaggressions] – like accidental misgendering or not being called [their preferred] name in a medical setting – all the way up to people who have experienced outright transphobia, homophobia, or poor treatment when they disclose things like sex work.”
And for some people, Dr McGregor said, a speculum examination was “just too much”. People who had experienced sexual trauma could find the examination “incredibly traumatic”, and trans men could find such an invasive examination dysphoria-inducing, she said.
“If we can offer them HPV swab self-collection and then they are going to be fine for 5 years because it comes back negative, I think that’s an incredible thing to do for people,” she said.
Both Drs Mann and McGregor applauded the MJA authors’ inclusion of trans men and non-binary people in the discussion about cervical screening.
Dr Mann said there was still some way to go in general practice in broaching issues of screening with gender diverse people.
“There is a huge amount of confusion in the minds of [practitioners] who come across transgender people about what screening they ought to be doing. Even the ability to ask the question to someone who has a beard ‘do you have a vagina and a cervix?’ is important,” said Dr Mann, who welcomed the recent position statement on the hormonal management of adult transgender and gender diverse people.

 more_vert
more_vert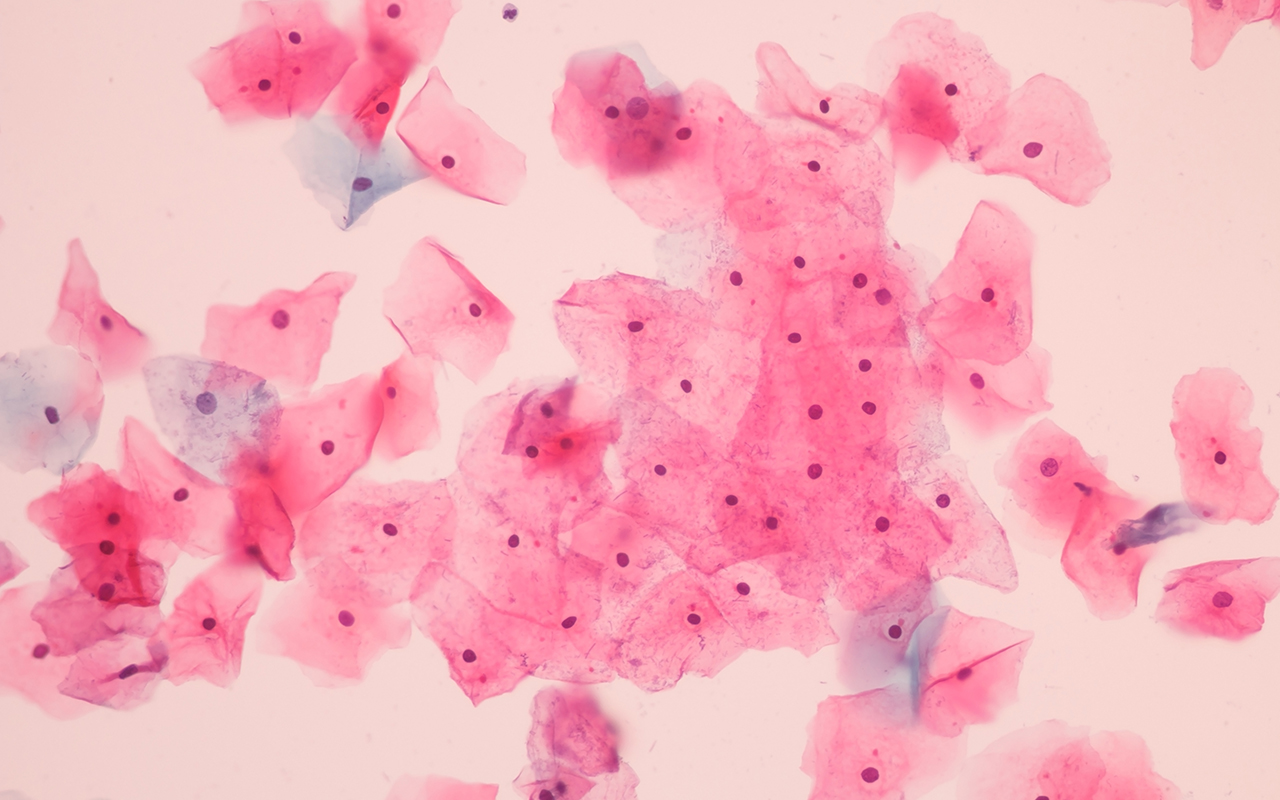
Self collection would be really helpful for women with last history of sexual abuse/trauma. I have patients who stoically come for usual screening tests but it is obviously painful for them and difficult physically and emotionally for me to do. Also as it is difficult to do, I have never been certain of the quality of the collection and would be much happier in this situation for self collection.
This is great, for all the reasons they mention, but why the focus on LGBT individuals? There’s plenty of cis-het women that would benefit as well.
I have had similar frustrations of being unable to opportunistically screen underscreened women , especially those who have never had the newer HPV test I had one person agree to do self collection and pathology was not done due to technically not quite 4 years.Self collection needs to be available at 2 years after last screen until everyone has had at least one HPV screen.
Sensible and pragmatic,thanks
Barriers are not needed
i AGREE
i HAVE RECNTLY PUBLISHED AN ARTICLE STATING THE SELF COLLECTED SAMPLES ARE ACCEPTABLE AND SHOULD NOT BE WITHHELD
Essential for the marginalised populations described in this article, as well as women with histories of sexual abuse & other sexual trauma.
Who wants another speculum examination if that can be avoided?
It would be interesting to know if the rejected specimen Dr Mann describes was collected in the correct manner. From a laboratory perspective, the majority of self-collected specimens submitted (9/10) have been unsuitable, that is, not taken with a dry flocked swab. It is important to note that the laboratory is bound by the Medicare rules; if that lady was not overdue for her smear yet, Medicare WILL NOT pay the lab to perform the test. They are a brick wall in these regards. Then if we process the test and issue an invoice we get into trouble. Damned if we do, damned if we don’t.