PATIENTS with uncomplicated diverticulitis can be effectively and safely managed in an outpatient setting and, in most cases, without antibiotics, say experts.
A new narrative review in the MJA reported that most international guidelines now recommended antibiotic use on a selective case-by-case basis only.
The review of international guidelines published between 2007 and 2017 also found that a key shift in the past decade was towards outpatient management of afebrile patients with clinically stable, uncomplicated diverticulitis and no other reason for admission.
In an exclusive InSight+ podcast, co-author Ms Amy Sweeny, Research Development Manager and Research Nurse at Gold Coast Health, affiliated with Griffith University, said her group’s review findings mirrored those published in the New England Journal of Medicine in 2018, which found “insufficient evidence to defend routine antibiotic use in this setting”.
The authors pointed to an outpatient management strategy set out in 2018:
- clear liquid diet for 2–3 days;
- low fibre diet until pain improves;
- acetaminophen (paracetamol) plus antispasmodics for pain; and
- use of antibiotics on a case-by-case basis.
Ms Sweeny said, historically, uncomplicated diverticulitis had been treated “quite aggressively”.
“Patients who came in with even mild symptoms would get admitted to hospital and put on intravenous antibiotics for 2–3 days, put on bowel rest … and that was still commonplace when we did our audit of our local practice,” she said.
“This is too aggressive … there are risks, of course, with antibiotics; there are social risks to patients who are kept in hospital for days when they could be back at home being managed conservatively. Hospitalisation isn’t necessarily a good thing, especially as we age.”
The MJA review also reported that computed tomography was the gold standard for initial diagnosis – with high sensitivity and specificity (94% and 99%, respectively) – and evaluation of severity. Uncomplicated diverticulitis is diagnosed when there is evidence of inflammation without abscess, perforation or peritonitis, the researchers wrote. Complicated diverticulitis is diagnosed when an abscess, perforation and/or peritonitis is found.
Dr Katie Ellard, Sydney gastroenterologist and spokesperson for the Gastroenterological Society of Australia, said a key shift in management was in the higher threshold for the use of antibiotics in uncomplicated diverticulitis.
“It’s certainly well recognised now that you don’t necessarily default to antibiotics in mild episodes of uncomplicated diverticulitis.”
Dr Ellard said that patients were often anxious about the possible complications of repeated episodes of diverticulitis and didn’t understand that antibiotics were not always necessary.
“It’s also important to emphasise that not all abdominal pain is diverticulitis,” she said. “It can be irritable bowel syndrome or constipation.”
Dr Ellard suggested that patients keep a thermometer on hand so they can tell the GP if they have a temperature, which may help confirm the diagnosis.
She said the lack of evidence around how to prevent recurrences was frustrating for patients.
The MJA authors noted that only general lifestyle advice – a body mass index under 30, vigorous exercise, avoiding smoking, and limiting red meat consumption – was backed by evidence.
But Dr Ellard said clinicians could not guarantee that any preventive strategies would be effective.
“A lot of people are still told that they need to change their diet and give up foods containing seeds and avoid multigrain bread, but there really is no evidence of that because it is the little bits of [stool] that get stuck in the diverticula pocket,” she said.
“I tell people that they should have a good diet, but they should eat what they like. They should do their best to avoid constipation, but that’s not absolutely borne out [by the evidence]. They should have 6–8 glasses of non-caffeinated fluid a day, and I do tell people they should walk.”
Dr Ellard said many years ago, surgical resection was offered to patients who had experienced three episodes of diverticulitis.
“Now, surgeons are quite reluctant to do this,” she said.
The authors noted that surgical intervention with either Hartmann procedure or primary anastomosis, with or without diverting loop ileostomy, was indicated for peritonitis or after the failure of non-operative management.
Dr Ellard said for some patients, episodes of diverticulitis became less frequent over time. However, some subgroups seemed to be particularly vulnerable to continued episodes.
“Young men who start getting diverticulitis in their 30s or 40s, will often end up having surgery,” she said. “But surgery is by no means a definite outcome.”
Ms Sweeny said she hoped the review would prompt professional bodies to revisit their websites to ensure patient information provided was in line with the latest guidelines and evidence.
“Changing expectations of our patients is also important and I am hoping that this review … will not just give impetus to GPs and emergency department doctors to change practice, but also for our professional bodies to look at [their patient information],” she said.

 more_vert
more_vert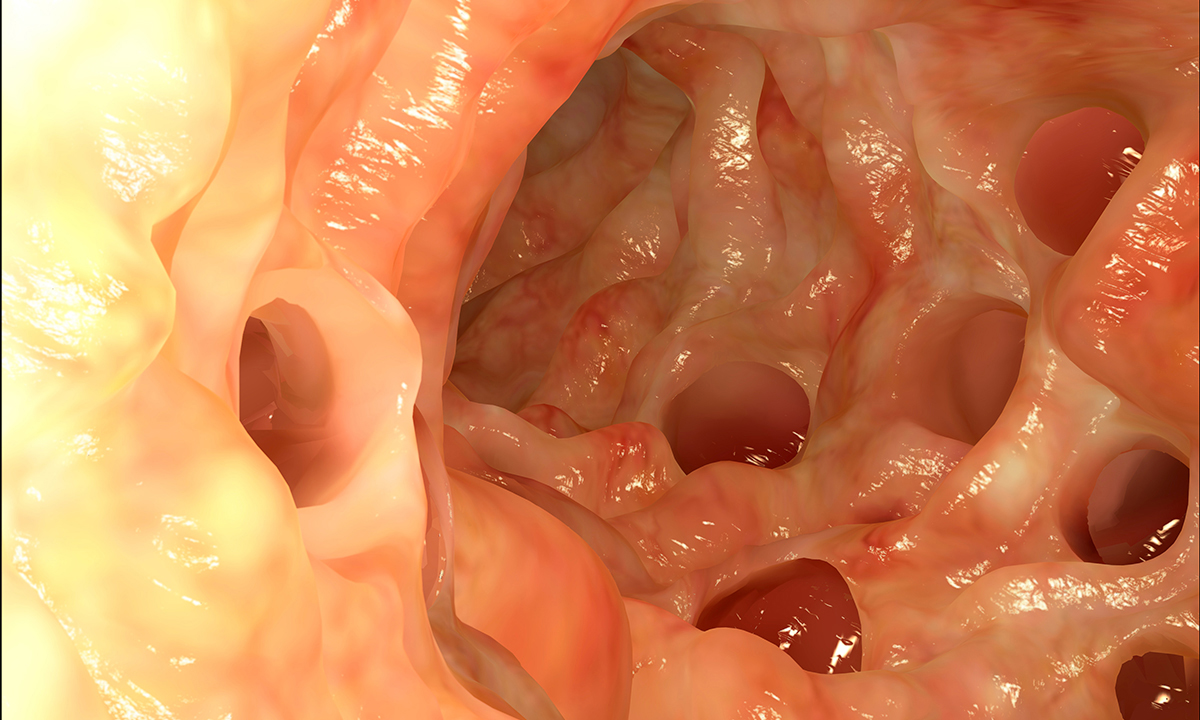
I am a registered nurse who normally nurses patients in hospital diagnosed with complicated Diverticulitis, not as many in Newcastle as I did down in the Windsor/Nepean district which TBH I found quite interesting. Six days ago I suddenly became the patient. I am a 50yr F, I had rapid and spontaneous onset of RUQ pain on movement, especially palpation. I finally presented to ED. I was febrile and tachycardic with a pain score of 10, nausea no vomiting, normal bowel habits for me, anorexia, and insatiable thirst.
I was finally seen by a Dr. seven hours after presenting. Nine hours after I had an abdominal ultrasound. Twelve hours after presenting I was admitted. First on clear fluids then NBM awaiting an ERCP or MRCP. Neither eventuated. Thirty two hrs later I had a CT scan. Thirty six hrs later and only 15mg Endone for pain the entire time, I was put on IV Ampicillin 2g QID, and IV Metronindazole 2g BD. I was told that I had a diverticula and a contained perforated ascending colon which explained the severe RUQ pain. I was discharged today after 4 days of IVAB treatment. I remained on a free fluid diet after the commencement of treatment.
I am booked for a colonoscopy in 6 weeks. Reading the CT report was alarming – it said that this could be Diverticulitis however, considering the atypical location of the perforation colorectal cancer cannot be excluded so visionary exploration is highly recommended.
Needless to say I’m now very concerned as I wait for my colonoscopy. I am hugging my kids a lot more and getting my affairs in order. I’ll know what to expect in 6 weeks.
Interesting; As a general surgeon I treated hundreds of cases over the years, and all but the mildest cases were admitted to hospital for body rest, gut rest, and either oral or IV antibiotics. I agree that many could have been managed at home. Initially , diagnosis was clinical or by barium enema X ray, the latter made obsolete by CT scanning and colonoscopy. As medical students we were taught that fruit skins, nuts and seeds should be avoided long term in diverticulitis patients, but there has never been any evidence to support this and I stopped giving this advice a couple of decades ago. My impression was that episodes of diverticulitis were more likely in overweight males and smokers.
It should be added that all patients should get a follow up colonoscopy ( 6-8 weeks later) to confirm the presence of diverticula and exclude malignancy.