EXPECTATIONS, needs and demands in health care are evolving rapidly and health leaders are facing more challenges than ever before. This includes more complex care, pressure on health budgets, reform agendas, new digital and data challenges, increasing regulation, commercial influences, more demands with regards to clinical and organisational governance, and burnout and suicide among health professionals.
This is complicated by a health care sector with many different voices and players, which makes a unified response to these challenges difficult. There is clearly room to improve coordination and planning within the sector.
Professional culture
Most of us have a deep-seated desire to belong, to find our lot, the ones who look like us, think like us, the ones who believe in the same things we believe in. There is a great sense of comfort when we are among our own, but this does not always challenge or extend us, and may lead to silos, fragmentation and division.
As a result of the disunity, the health care sector is often ignored in policy development and reform. Neatly divided into “us” and “them” it becomes easy for policy makers to separate the sector, playing one off against the other, accentuating the differences and ignoring the common ground.
An overly competitive culture can also be unhealthy. Our junior doctors are struggling under the burden of competition, the need to fight to prove their worth, that they are “better” than one another. Physician burnout, stress and suicide have never been as confronting as they are now.
Better together
Of course, there is much more that unites us than divides. While our thought processes may differ, our aspirations are often closely aligned.
We need healing in our profession; healing that encompasses the breadth of generalist and specialist medicine, and of nursing and allied colleagues. It is past time that our leaders broke bread together, listening to each other and respecting the differences that define us, while embracing our common hopes and aspirations.
We need to stop fighting each other and instead work together to defeat the common foe, be it turf wars, egocentric and sector-centric protocols, damaging workplace cultures and so on. We need to build purposeful partnerships.
More professional collaboration is priceless. Each party can bring their unique constituencies to bear on complex problems. By harnessing the true power and wisdom of the collective it is possible to overcome the artificial barriers that hold us back and more effectively manage today’s health care challenges together.
Finding common ground
How do we reach more unity and collaboration in the health care sector? Even though we all say we want more unity, our desire for unity is not absolute. Sometimes what we really mean is “unity around the positions I hold”, meaning that we want others to accept our viewpoints.
Unity and collaboration are only comfortable in the abstract. The process of finding common ground involves compromise and discomfort. It is as if we are all in separate little dinghies on the sea, and we need to get in the same boat. If there is no rocking the boat, we will get nowhere, but if there is too much rocking, we get thrown overboard.
Collaboration is more than simply working side by side or getting the technical skills mix right; it is also about building relationships.
Building bridges
There is always a better way to do something; ways that have yet to be dreamed or imagined. The recently commenced BridgeBuilders project aims to start conversations about collaboration and encourages health care professionals, especially those in leadership positions, to reach out across organisational boundaries.
The project was initiated by a group of Australian GPs who believe that more collaboration between different health groups and organisations is much needed. BridgeBuilders does not claim to have the answers to today’s challenges and it is apolitical and non-denominational.
The passionate blog posts by doctors, nurses, consumers and others are a reminder that the sum of the whole is greater than its parts. Building bridges in health care is a bit like building links for the future: connecting people, building trust and facilitating relationships. These foundational components of successful collaboration are a basic requirement for our future health care leaders to lead together more often.
Everyone is invited to post their views on building bridges on the blog, and we especially want to encourage colleagues to sit down and chat over a cup of tea with someone from a different organisation or profession, focus on the common ground and discover new ways to improve collaboration.
Building bridges from foundations of understanding, respect and our shared passion as health care professionals is critical to complete ourselves and to inspire generations to come. More collaboration between health groups is needed to tackle the challenges our leaders are facing today and in the future.
For more information visit https://bridgebuilders.vision. Twitter: @Bridg3Builders.
Dr Wendy Burton is a Brisbane GP, whose specific interests are maternity and paediatric care, but she provides personalised care to all ages and genders.
Dr Ewen McPhee is a GP practising in Emerald in central Queensland. He is immediate past president of the Rural Doctors Association of Australia.
Dr Tim Senior is a Sydney GP who works in Aboriginal and Torres Strait Islander health.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or MJA InSight unless that is so stated.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert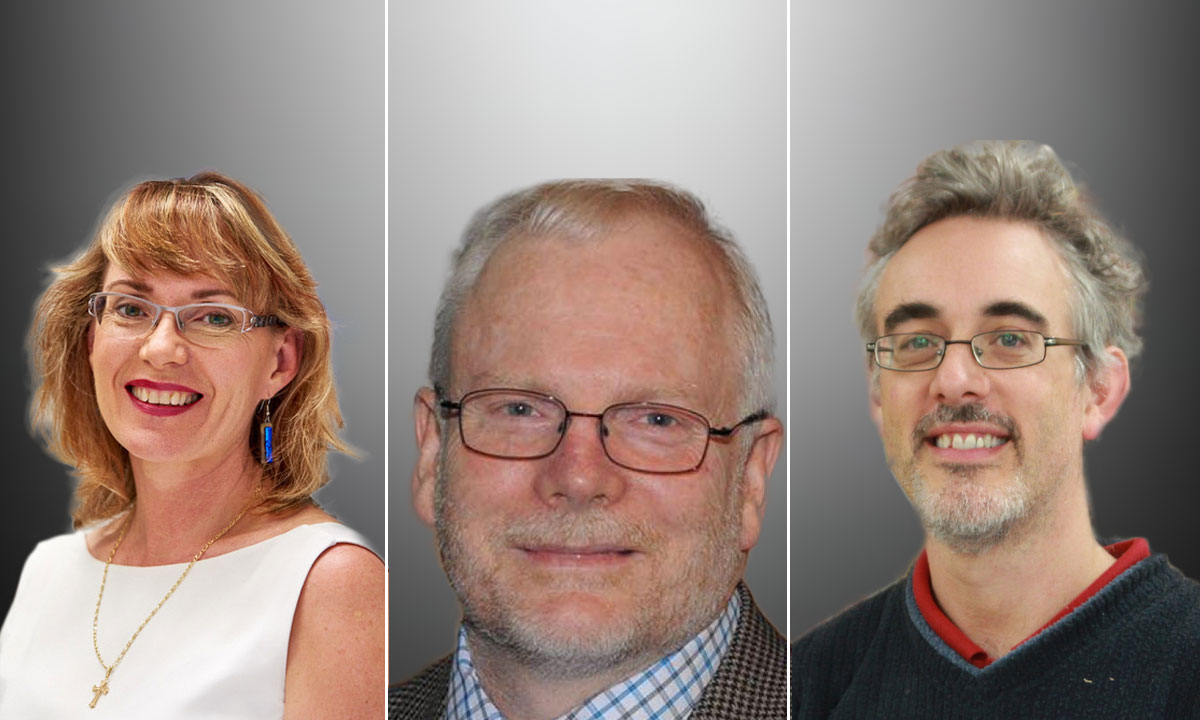
Agreed – ‘More collaboration between health groups is needed to tackle the challenges our leaders are facing today and in the future’, but I would unequivocally added – more collaboration and communication with patients.
In the Health System there are policies, processes and systems that do not meet the needs, wants and desires of patients.
A submission has been made to the Parliament of Australia, Select Committee – see ‘Sub244_Bourne and Associates Replacement.pdf’. The matters raised in this paper are focused on, but not exclusive to, ‘Who Matters and Who Doesn’t’ – our ‘Whole-of-Person’ approach ie we approach the problem from different, but complementary perspectives ‘ Words Matter’ and ‘Silo mentality’.