MULTI-parametric magnetic resonance imaging (mpMRI) promises to be an effective second-line diagnostic tool for men with elevated prostate-specific antigen (PSA) levels or an abnormal digital rectal examination, say Australian experts, after a UK study found that the additional screening measure improved the detection of clinically important disease and reduced the detection of insignificant tumours.
In a commentary published in The Lancet, Dr James Thompson and Dr Philip Stricker of the St Vincent’s Prostate Cancer Centre, Garvan Institute of Medical Research and the Kinghorn Cancer Centre, said that in the wake of disappointing results of recent randomised controlled trials of PSA screening, “novel diagnostic tests with higher discriminative abilities for aggressive prostate cancer” were urgently needed.
“Multi-parametric MRI might be used as a second-line diagnostic tool in men with abnormal PSA or digital rectal examination to improve selection for biopsy,” they wrote.
Their commentary was in response to findings from the PROMIS study, a prospective, multicentre, paired-cohort, confirmatory study of the diagnostic accuracy of mpMRI and transrectal ultrasound-guided (TRUS) biopsy in prostate cancer, published in the same journal in January 2017.
The PROMIS study analysed the accuracy of mpMRI in 576 men, using a 5 mm grid-template transperineal biopsy (TTMB) with 60–70 cores and 12-core TRUS biopsy reference tests. The researchers reported a high sensitivity (93%) and moderate specificity (41%) for mpMRI.
“Using mpMRI to triage men might allow 27% of patients avoid a primary biopsy and diagnosis of 5% fewer clinically insignificant cancers,” they wrote.
Dr Thompson and Dr Stricker wrote that PROMIS results reflected their own findings, which were published in the Journal of Urology in 2016. Their study of 338 men, which used 30-core TTMB as the reference test, found that mpMRI had sensitivity of 96%, specificity of 36%, negative predictive value of 92% and positive predictive value of 52%.
“The high sensitivities reported in both PROMIS and our study (the two largest studies to date) suggest that the lower estimates in previous meta-analyses might be influenced by confounding factors such as small sample size, use of radical prostatectomy as the reference test, and use of any cancer as the endpoint definition,” they wrote.
Speaking to MJA InSight, Dr Stricker said that the PROMIS study showed that mpMRI added “quite significantly” to the accuracy of a simple PSA test.
“PSA testing has unquestionably found cancers at an early stage so that we can cure them, but the problem has been overdetection and overtreatment,” he said. “Based on the findings of this study, mpMRI goes a long way towards avoiding overdetection, by missing out those Gleason 6s [the lowest grade prostate cancer].”
Dr Stricker said that the move to active surveillance of low grade tumours was also addressing the problem of over-trestment.
“Now, when they do find these low grade tumours, we are not treating them, just monitoring them,” he said.
Associate Professor David Smith, senior research fellow at the Cancer Council NSW’ Cancer Research Division, said the PROMIS findings suggested that mpMRI was a step forward in improving the accuracy of prostate cancer diagnosis.
“Ever since PSA testing became common, we have known that we needed better tests to accurately diagnose men who need treatment and differentiate those who do not need treatment, or could be put on active surveillance,” he told MJA InSight.
Professor Smith said that mpMRI testing prior to prostate biopsy was not assessed in the 2016 release of the Prostate Cancer guidelines, and that a 2016 Griffith University analysis showed that mpMRI was cost-effective in men with low-risk disease who were subsequently managed with active surveillance.
“I think the dial may be changing and the results of PROMIS are certainly indicative of a move towards supporting this,” Professor Smith said. “Anything that can reduce the number of biopsies and the risk of infection that accompanies those and the number of men who can be safely managed on active surveillance is of benefit in the overall picture of reducing the harms associated with prostate cancer.”
Dr Stricker said that there were two key barriers to mpMRI prostate diagnostic scans being rolled out more widely: accuracy and cost.
“The accuracy is dependent on the radiologist’s experience. There is a learning curve, and some upskilling of the radiologist may be required,” Dr Stricker said, adding that in specialist units, such as his own and those participating in the PROMIS study, the negative predictive value was about 93%.
He said that the current cost of an mpMRI was $600, but this could be reduced to $200.
“We don’t believe that the contrast scan – the third component of the mpMRI, where you inject gadolinium – will be necessary, and that will reduce the cost to about $200,” he said. “Finding unnecessary cancers and doing unnecessary biopsies is expensive, and so if you do a cost analysis of that, it’s very much in favour of doing an MRI.”
The Medical Services Advisory Committee is currently considering an application to list mpMRI prostate diagnostic scans on the Medicare Benefits Schedule.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert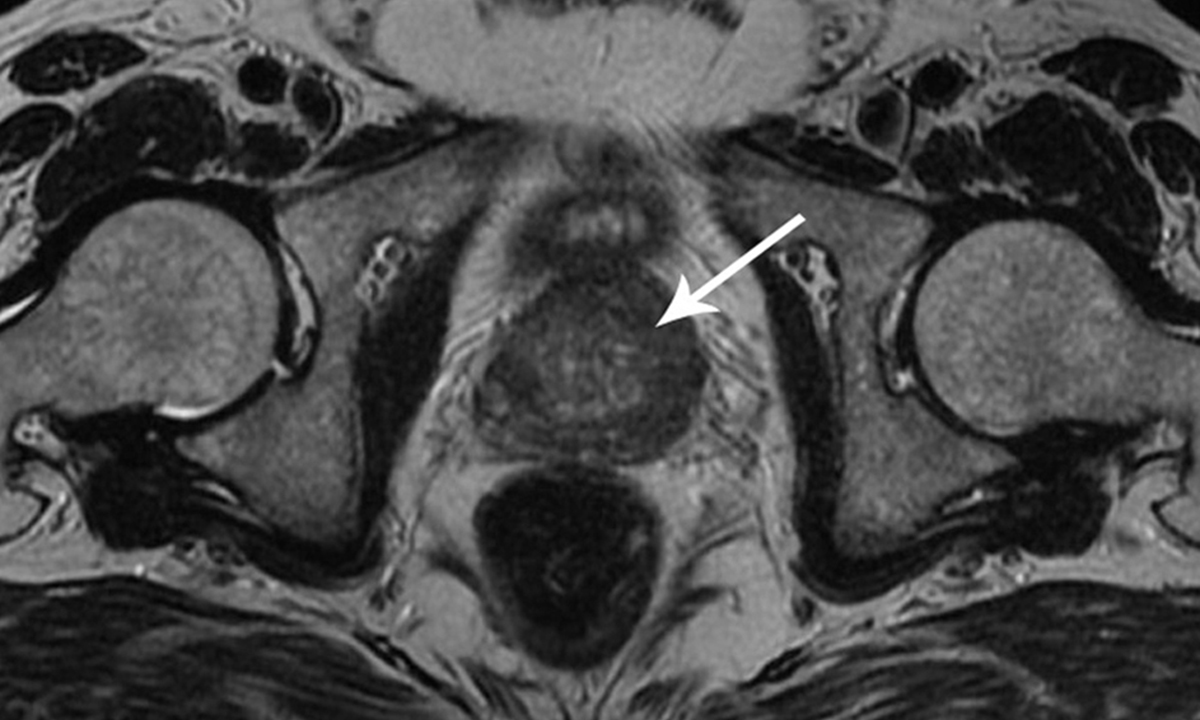
If only I had known the low grade accidentally PSA discovered would not have effected me in 15 years , or if ever , then I never would have had treatment at 60. PSA consistently around 4 over a fifteen month time frame except for the first reading of 9.7 , (elevated).
I faced the deepest concerning groans from urologists , that concerned glare over the glasses , “where there’s smoke there’s fire you know” !
My GP and a second GP didn’t know what to do. The second urologist pushed the same sales spin.
Nothing will change on overservicing until some clinicians face serious charges for overservicing.
The average punter off the street cannot deal with the ocean of information and emotional freight train this is , so they turn to specialists who stand to make many thousands of $$$$$$ unchallenged.
THAT’S WHY IT CONTINUES TO HAPPEN.