WHEN Professor Colleen Loo, a University of NSW psychiatrist based at the Black Dog Institute, first heard about the astonishing effects of ketamine in treatment-resistant depression, she was sceptical.
“I was hearing these stories from overseas but I didn’t believe them, which is why we started our own research around 6 years ago. And pretty much immediately, we started seeing the same thing. People went from being in a state of severe depression to being completely well after a dose of ketamine, in a matter of hours. In 25 years of clinical practice, I’d never seen anything like it. I was just completely astounded.”
Professor Loo and her colleagues have just published results from a small trial of ketamine in elderly patients with treatment-resistant depression. It involved 16 patients over the age of 60 years who were given up to five doses of ketamine a week apart, with a dose of midazolam randomly inserted.
Ketamine – a Therapeutic Goods Administration-approved anaesthetic and a well known party drug – was well tolerated, and seven of 14 trial completers achieved remission. Doses of 0.2 mg/kg or above were found to be significantly more effective than midazolam.
Professor Loo said that more than 10 proof-of-concept trials have now looked at ketamine’s antidepressant effects.
“What they have shown very clearly and consistently is that there is a very big effect on improving mood after ketamine, compared with placebo. And the difference is much greater than what you typically see for antidepressant medication.”
She said that another difference with conventional antidepressants is the speed at which ketamine has its effect.
“With other antidepressants, you’re looking at weeks before you see an effect, but with ketamine the peak effect is at 24 hours.”
So, have we reached a tipping point at which doctors can safely start prescribing the drug to their treatment-resistant patients? The short answer is no, Professor Loo says.
A key drawback is that the antidepressant effect of ketamine lasts only a few days. And that opens up a real can of worms, because little to no research has been done on the long term effects of repeated doses of therapeutic ketamine.
Professor Loo said that the side effects of ketamine – dizziness, dissociation, blurred vision and high blood pressure – are generally well tolerated with a single dose, and resolve within an hour. But in frequent users, the effects might be quite different.
“With repeated treatments you might get cumulative effects, and we know very little about that as there are hardly any data. What we do have comes from recreational users, where we don’t know what their dose was, how they’ve used the drug or how frequently. But there are potentially quite serious effects, such as inflammation of the bladder wall, abnormal liver function and cognitive deficits.”
And there are plenty of other reasons to be cautious about using ketamine to treat depression until more is known, Professor Loo added.
“I’ve had practitioners tell me about patients where the response to ketamine is initially fantastic, but with repeated doses it fades. So, they ramp up the dose and the frequency, but the effect keeps declining and they find themselves in a vicious circle. In the end, their depression is the same, but now they have an addiction problem as well, so they’re worse off than when they started.”
Dr Kym Jenkins, President of the Royal Australian and New Zealand College of Psychiatrists, agreed that clinicians have to remain very cautious about prescribing ketamine for depression.
“The college does have a clinical memorandum on the use of ketamine in depression. We’re not necessarily against it being prescribed, but we strongly recommend that it be used under research and trial conditions. We do know that it’s being prescribed outside that, but at the moment it’s only got Therapeutic Goods Administration approval as an anaesthetic, so people need to have a clear understanding that it’s a novel treatment and not approved for depression.”
Dr Jenkins said there were still many things we don’t know about ketamine for depression, such as optimal dosing and optimal administration method, what treatment protocols should be, and the longer term side effects.
“There are a lot of unknowns, but a lot of hope as well,” she told MJA InSight.
A major trial, currently recruiting in Australia and New Zealand, may answer some of those questions. Professor Loo, who is the trial leader, said it would be the largest to date to look at ketamine and depression, testing the effect of twice-weekly doses over 4 weeks in 200 patients.
Professor Loo said that recruitment should finish in 2018, with preliminary results coming out in 2019.
She said that she was very hopeful that ketamine would play a role in the treatment of depression, but at the moment it wasn’t yet clear what that role would be.
“It could be an early treatment – a quick initial boost to kickstart people out of their depression, so they can get on to another, safer treatment. Or it could be used for treatment-resistant patients who have failed multiple medications. Or it could be a first line treatment. We just don’t know at the moment.”
But she cautioned that with high efficacy, high impact treatments such as ketamine, there is a smaller window of optimal dosing than for conventional medications.
“There’s a small margin for error, so it’s not going to be a straightforward tool to use. I’m hopeful that it will transfer to mainstream clinical practice, but we need to do it carefully. If we don’t do the careful studies beforehand, we could have some bad results that could derail the field completely.”
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert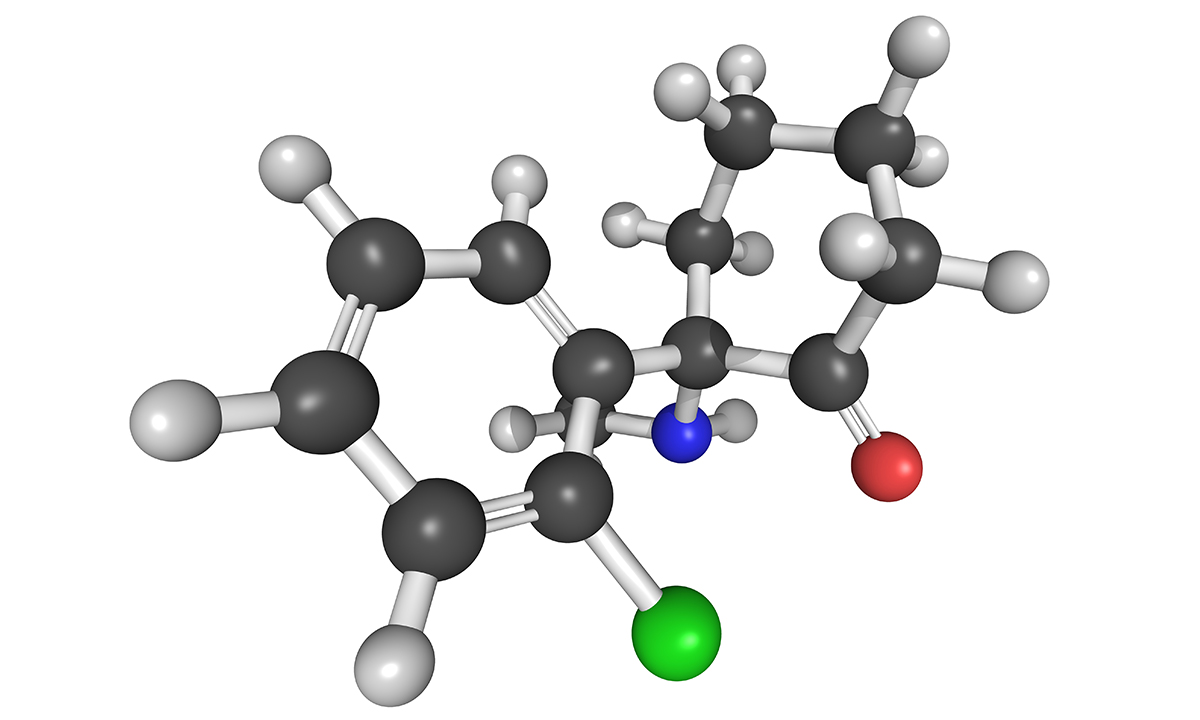
Frankly after over a year of relief from depression using low dose oral ketamine regularly, no kidney, liver or urinary issues, I am prepared to accept that there might be side effects in the long term I am not yet aware of. I will take those effects over the slow suicide that was my life trying ECT, TMS, neurofeedback, anti-depressant after anti-depressant, major tranq after major tranq (most with one or two bad to hideous side effects) and very difficult to come off without nasty side effects. How about the long term side effects of the SSRI’s and other newer generation anti-d’s? We don’t here ppl making a fuss about that like with the dreaded ketamine.
KETAMINE SAVED MY LIFE.
Having used ketamine many times for treating chronic pain , I have used it once on an acutely suicidal patient. The response can only be described as miraculous. There are a number of published studies showing it’s benefit for reducing acute suicidal ideation. Is it ready for routine management of depression – no. Is it ready for acute crisis intervention – I would argue yes. Having worked as a CMO in hospital A&E for many years I had arguments with psychiatrists about sending acutely suicidal patients home because there were no beds (there are never enough psych beds). The parents would be terrified and such actions placed the burden on them. CAT teams are effective for the time they are present, but there is a lot of MH issues in the community and the teams have to move on to the next crisis. Administering a 40 min infusion (as per published protocols) in the emergency department can dissolve crises and save lives. I think the time has come to adopt bold approaches in acute suicidal crises, and I suspect there would be no shortage of emergency departments wanting to participate in a trial.
Hopefully Anonymous is aware that Ketamine can cause a very nasty cystitis (as seen when it has been used in the longer term in Palliative Medicine)
Dr Loo continues to ignore the evidence from pain physicians e.g Varun Jaitly and Lucinda Grande who have demonstrated that ketamine can be safely used in low regular daily doses over many years.
Those patients with severe treatment-resistant disorders deserve the opportunity to evaluate the evidence and make considered choices based not just on clinical trials on highly selected atypical patients, but also taking into account the experience of doctors treating “real” patients with multiple co-morbidities.
The College’s current approach ensures ongoing suffering and premature mortality to the 30% of people who do not respond to our current therapies.
When I used Ketamine as an anaesthetic agent many years ago, quite a few of the patients experienced hallucinations upon arousal and this was ameliorated by the use of valium or midazolam.
Many of the older practitioners can remember the positioning of the big Blue “K” left on the patient’s bedside until they had recovered. The unexpected side effects of Ketamine including pain relief and relaxation have been known for many years, but continued use has never been recommended and care in prescribing it for depression needs long term study.