GPs will be the target of a new education campaign on identifying the symptoms of vaginal mesh implant complications, amid reports that many patients’ pleas for help were not taken seriously by their doctors.
Dr Robert Herkes, clinical director at the Australian Commission on Safety and Quality in Health Care, said that the commission was preparing educational materials for GPs in response to feedback from patients, clinicians and health system representatives.
Women with mesh complications frequently reported that “their GPs wouldn’t associate any of their symptomatology with the mesh, and sometimes didn’t even know it had been inserted,” Dr Herkes told MJA InSight.
“Often, they sought advice from a gynaecologist, who also doubted the severity of their symptoms,” he added.
Around 151 000 urogynaecological mesh devices have been supplied in Australia since 1998, according to the Therapeutic Goods Administration (TGA), including 31 805 intended for the now controversial pelvic organ prolapse procedures.
The TGA says it has received adverse event reports from 249 women who received mesh implants, but that’s likely to be the tip of the iceberg. About 1000 Australian women with mesh implants are involved in two separate class actions against manufacturers Johnson and Johnson and American Medical Systems. According to Shine Lawyers, up to 8000 women are thought to have been impacted by the Johnson and Johnson pelvic floor repair systems alone.
Dr Herkes said that the commission had met around 45 women suffering complications from mesh implants at public hearings in Brisbane, Melbourne, Sydney and Perth.
“These women had extensive symptomatology; pain, not just pelvic but often sciatic too; infections and mesh migration,” he said.
“About 25 minutes after our meeting with the women had started, half of the women were standing up walking around the room because it was too painful to sit. Some were unable to come in on public transport because they were so uncomfortable.
“Almost all the women we met were divorced and believed that was secondary to having pain during intercourse, which may have led to their partner leaving. Many of them had lost jobs because they were unable to work due to sickness or incontinence.”
The delay between mesh insertion and symptoms of complications varied between women appearing at the hearings.
“Frequently, women brought their concerns to GPs a year or two after mesh insertion,” Dr Herkes said. “However, some women got pain immediately, and for some, the mesh problems started 10 years after insertion.”
To ban or to regulate?
A growing number of victims are calling for a ban on gynaecological mesh, but doctors have countered that not all uses of mesh are unsafe.
According to the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), synthetic mesh mid-urethral slings (also called tension-free vaginal tape) are the gold standard surgical treatment for stress urinary incontinence.
RANZCOG president Dr Steve Robson explained that most of the problems with mesh have occurred where it has been placed across the vagina – predominantly for the repair of pelvic organ prolapse.
“Initially, surgeons were enthusiastic about using mesh to reduce the prolapse recurrence rates seen with native tissue repair – after all, mesh had been used safely for a long time in abdominal wounds with good success,” Dr Robson told MJA InSight.
“What wasn’t appreciated at the time was that the thinner and more delicate tissues of the vagina – especially in post-menopausal women – may not fully heal over the surface of the mesh,” he said. “The skin can break down over the top of the mesh.
“The recommendation now is that if you’re going to use mesh for prolapse, you should only do so in the context of a clinical trial, and of course, thoroughly inform patients of the potential risks,” he added.
A Cochrane review found that 8% of women treated with mesh for pelvic organ prolapse required repeat surgery for mesh exposure. The review concluded that even though recurrent prolapse was less common when mesh was used, the risk–benefit profile meant it had limited utility in primary surgery.
It has been claimed that lightweight transvaginal meshes are associated with a lower risk of complications; however, the Cochrane reviewers warned that this claim has not been tested in a randomised controlled trial.
The TGA is proposing to make all surgical mesh devices “high risk” (Class III), in line with recent European amendments, meaning that each device would need “design examination certification” in order to be supplied in Australia.
Patients would also be given an “implant card” containing detailed information about their specific device and its associated risks.
Dr Herkes said that a more rigorous system of post-marketing surveillance for implanted devices needed to be developed, possibly including a registry similar to that in place for joint replacements.
He also supported credentialing surgeons to use transvaginal mesh, given evidence that complication rates were lower with more experienced surgeons.
“It’s probable that the commission’s expert committee will recommend that mesh should only be used as a third-line therapy for pelvic organ prolapse after the failure of non-surgical treatments and native tissue repair,” he said. “Some surgeons were using surgical mesh as a first-line treatment.”
Should the mesh be removed?
Professor Peter Dwyer, clinical professor of obstetrics and gynaecology at the University of Melbourne and at the Mercy Hospital for Women, told MJA InSight that he had removed gynaecological mesh products and infected sutures from more than 100 patients in his more than 30 years’ experience in urogynaecology.
While some women required surgical removal of the mesh due to pain, he claimed that others were requesting it when it was unnecessary.
“Chronic pelvic pain affects 20% of all women and in many cases, no cause is found … people don’t appreciate what a common problem pelvic pain is,” he said.
“A lot of patients want the mesh removed, even though they have no symptoms, because they’ve read all the headlines,” he said. “I’ve had a lot of women present with concerns that they’ve got a foreign body eroding into their tissues, but when I’ve examined them, that’s not the case.”
Professor Dwyer stopped using transvaginal mesh a decade ago, concerned by growing reports of erosions. Nevertheless, he said: “I would hate to see mesh outlawed altogether, because sometimes you do need it and there’s nothing else”.
Mesh removals were usually straightforward and complete, he said. They could be more difficult when the mesh was implanted through the pelvic side wall – sometimes only 80% of the device could be retrieved in these cases.
Professor Dwyer said that women who are worried about their mesh implants should make an appointment with their surgeon to discuss their concerns and possibly have an examination.
“Regular follow-up is not necessary; the patient only needs to present to their doctor if they have symptoms,” he said.
Professor Dwyer will appear as an expert witness for Johnson and Johnson in the company’s class action defence.
Several manufacturers have withdrawn their gynaecological mesh products from the market, and the TGA delisted one Australian-manufactured device in 2006. However, 29 devices remain.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert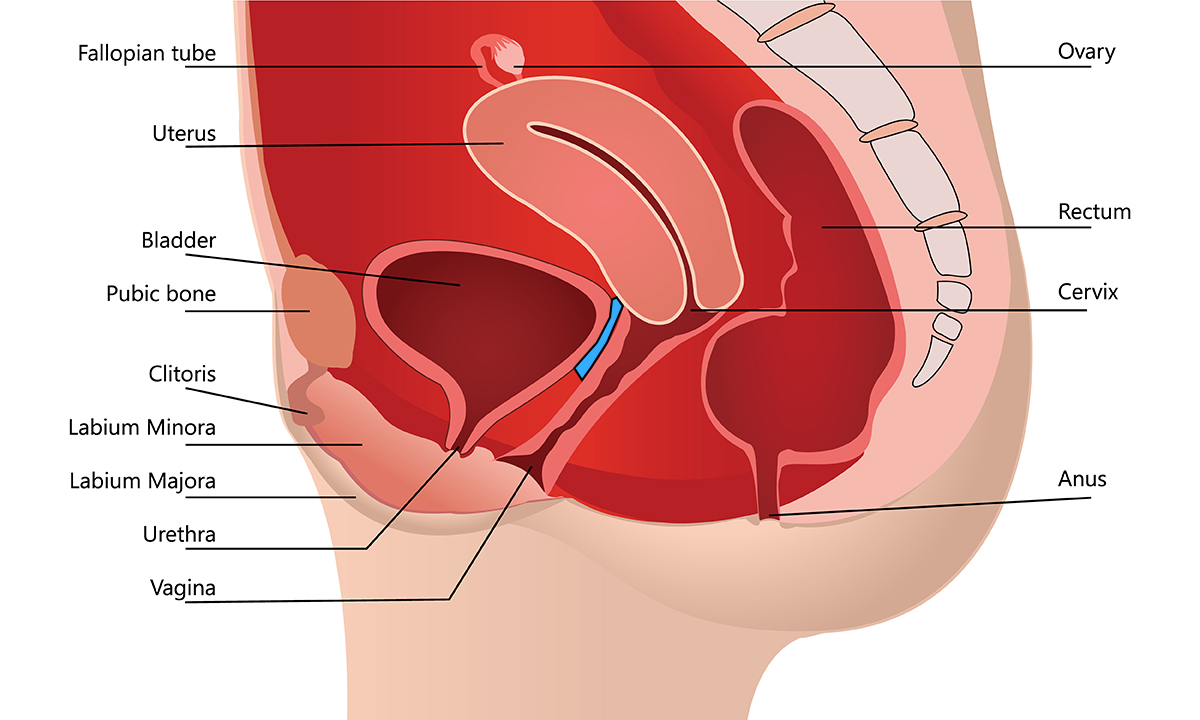
Professor Dwyer you are not that stupid. So why make a statement like most mesh removals are straightforward and complete. I have a letter from a leading Gyno in Australia stating my mesh cannot be removed in Australia. No one is qualified to remove it. Most removals in Australia are extremely difficult as described in our operating notes by the surgeon and are partial. You can count on one hand the surgeons in Australia capable of removing any mesh fully and even they are hit and miss. Even with the best removalist in the world it doesnt guarantee you will be any better. The nerve pain can be permanent. You can lose the use of your bowel and bladder. Stop sticking up for these companies. So many lives and families ruined. All the pro mesh Drs are going to be on the wrong side of history.
I can relate to the pain! I’ve had four prolapse surgeries, one failed in 2010 and three with mesh within three years! I can’t sit, walk, bend down,look after my garden, or even manage a car trip more than twenty minutes drive! I often have spots of blood & green discharge from the bladder and then frequent bladder infections, so much pain and suffering.
it makes it very hard to manage my every day life, seeing that I am on my own!
The last surgeon who operated on me, tells me: it’s all fine& no problem!
GO FIGURE!!!
I have asked to be treated in the public system where I think, they have more knowledge about Mesh& I was refused treatment twice, they said: i live outside their Zone!!
something is wrong somewhere, the system needs looking into.
I have a very rare blood disorder as mesh migrated through an organ, 35 blood transfusions, inserted 2004 with no knowledge to repair a hysterectomy, years of uti kidney stones esophageal yeast bone density loss X 18 % 12 joint surgeries, I wasn’t in a relationship therefore, I didn’t know, nor was I told
And how many doctors rapport problems? Not 10!!!!
How many men and woman, with mesh, complained with their doctor, but were told..iT is all in Your head, you read too much on the internet..
Your terrible backpains? This is ‘normal’..wait for a few more months…
No bladderfeeling? This is ‘normal’…wait for a few months….
Extreme bloating….this is ‘normal…wait for a few months….
Soiling….all ‘normal’…takes time…
Bellypains?….”normal’…
Extreme constipation? More than before the operation?…..”normal”…take laxative….
Nervepains?….’normal’….all people with surgery have this….
This are only a ‘few’ examples..
In the mean time…
You get epidurales,facetinfiltrations,nervedenervations,
Take more painmeds but realise you are reacting on meds, food, etc..
A specialist finds that you have ASIA syndrom..
After a year of ‘complaining’….
Your doctor Will tell you…
Take the mesh out?….Now iT is too late, you have to search for a balance between the painclinic and weekly rincing Your bowels…
And you Will get upset because this Will be Your future…
And this ‘so called dr’ Will send a letter to Your homedr…’explained everything to this lady and she was reassured’….NOT AT ALL!!!
Does the ‘stort’ ends here?
Ofcourse not…
Your bloating gets more and more and you look pregnant..constipation gives you the feeling that Your bowels are going to explode..
Something you end up at emergency..
Oh and Your professor, who you and Your husband saw, who would operate you, you thought…
After asking for Your ‘real’ operatingpapers…you Will find out, he was not even in the operatingroom…
No, a ‘strange’ dr did the operation…the same strange dr who you met a month after Your operation and did Your complaints too,
And never Will this strange dr or Your prof tell you who did the operation..you Will have to find out for yourself…
And than, after a year, you Will meet Your professor, explain all the complaints and Will he send a letter to Your homedr..
IT Will say that with too much bloating he Will take Your bowel out and you Will have a ‘few’ times fluid stool a day, but iT Will get better…
And in this letter he Will wrote…I told this lady ‘al the complications’ and only we have to get the operationdate….
Never went back with this ‘dr’…
And than…after 4 years, Your homedr’ s don’t believe you Will gain wait while you say you did not more eat…
No, ‘they’ say…every pound gets through the mouth…
And Your legs and belly Will swell more and you get red ‘places’ on Your leg which Will burn like hell…
And Your homedr Will say….just exzema…
But you don’t feel right with iT because ‘you get too much on the internet’ and Will search for an other dr….
And you get a scintigraphy…which explains that Your lymphs in Your feet, legs and belly Will not work anymore how they should..
Due to this last operation…and this red ‘places’ are inflammation under Your skin due to long swelling …
And you Will search for somebody to treat this…etc…
Does iT stop here?….
No!!!
Because even the smallst handoperations Will give you problems, too much scarf, called fibrosis…
The mesh Will start inflammation for scarf..but this never stops…so you have to have second handoperations to remove the scarf…
Small detail…
I have ‘the gold standard’
A flat monofilament knitten mesh….not recalled…
Lack of complications from TFS? I find that difficult to comprehend seeing im coming up for yet another round of tissue anchor removal from migrating anchors oh and not to mention mesh that has vanished, chronic pain, unable to sit or walk for extended periods, unable to have sex the list goes on.
The sub-urethral sling developed by Prof. Peter Petros is still accepted as the “gold standard” for surgical treatment of urinary stress incontinence.A 5mm ribbon of mesh strenghens the pubo-urethral ligment leading to cure of symptoms.Mesh rejection is rare and easily treated.
Prof. Petros also developed the Tissue Fixation System (TFS) where similar 5mm tapes strengthen damaged cardinal and utero-sacral ligaments allowing cure of many pelvic floor problems.Again results were excellent with rare mesh rejection
Despite the lack of complications approval for the TFS was withdrawn by the TGA 2 years ago. There are no class actions against the TFS and the TGA have been unable to jutify their action.