THE incidence of anal cancer among Australians is increasing, according to research into the international incidence, but local experts say efforts to improve prevention, detection and treatment are underway.
A study published in the International Journal of Epidemiology found that the incidence of anal squamous cell carcinoma (ASCC) had increased in both men and women in Australia as well as in several other high income countries, including Canada, Denmark, France, Italy, the Netherlands, the UK and the USA.
In Australia, over the time period 1983–2007, there were a total of 1237 cases of ASCC in Australian men and 1904 cases of ASCC in Australian women, in an Australian population of over 20 million.
The incidence of ASCC had increased by 3.3% annually in men between 1989 and 2007, and by 5.9% annually in women between 1996 and 2007.
The researchers said that the reasons behind the increased incidence were unclear, but were likely to reflect changes in environmental risk factors. Infection with human papillomavirus (HPV), particularly HPV16, was an established risk factor for anal cancer, they reported, adding that almost all cases of ASCC were also positive for HPV.
Associate Professor Richard Hillman, a sexual health physician at the University of NSW’s Kirby Institute, said that anal cancer was more common in women than in men, particularly those women with a history of other anogenital HPV-related conditions.
“Women with a history of cervical cancer, for example, have generally a 10-fold elevated risk of anal cancer, compared with the background community,” Professor Hillman told MJA InSight.
Professor Hillman said that there was some uncertainty around the patterns of anal cancer in men, but gay men, particularly those who were HIV-positive, were at increased risk.
“HIV-positive gay men are the group at highest risk of all, presumably because of exposure to HPV plus impaired immunity,” he said.
“As our treatment of HIV has improved, many conditions have all but disappeared; however, the anal cancer rates have continued to increase.”
Transplant recipients too were at greater risk, Professor Hillman said, due to long term immunosuppression impairing the body’s ability to contain HPV infection.
He said that the introduction of the HPV vaccine – which has been available through the National HPV Vaccination Program to girls aged 12–13 years since 2007, and boys since 2013 – had dramatically reduced the prevalence of HPV in people aged under 26 years.
The HPV vaccine was expected to have a major impact on the incidence of anal cancer in the years to come, but Professor Hillman said that the effect would not be felt for several decades.
“We have this cohort of individuals who are mid-20s and 30s and beyond who have not been vaccinated pre-sexual debut and will have acquired HPV, and some will, over the years, develop anal cancer,” Professor Hillman said, noting that other risk factors included smoking and age.
He said that changes in sexual practices were likely to be responsible for the increasing incidence of anal cancer in younger cohorts.
“People who are 50 years old now have a higher rate [of anal cancer] than people who were 50 years old in the 1980s, for example,” he said. “The proposed explanation for that is change in sexual practices – more frequent partner change, and, potentially, we know that anal sex is more widely practised than it used to be among the heterosexual community.”
Professor Hillman said that HPV was highly infectious and the amount of sexual contact required for transmission was “fairly minimal”.
“You don’t need penetrative sex to acquire the virus, so even manual or oral sex may transmit the virus. While the condom message is very important to reduce the transmission of HIV, HPV transmission is only partially reduced by condoms,” he said.
Professor Hillman said that research efforts were underway to improve detection and treatment of pre-cancerous lesions.
“Detection is a big issue because that speaks to the stigma associated with anal cancer,” Professor Hillman said. “There is a stigma associated with anal function – and it’s not just among the general public. Clinicians are often reluctant to do anal examinations.”
While many anal cancers were asymptomatic, he said, the most common presenting symptoms were lumps, bleeding and tenesmus.
Professor Hillman said that the Study of the Prevention of Anal Cancer (SPANC), of which he is principle clinical investigator, was investigating a screening technique to improve the early detection of those most likely to develop anal cancer. He said that the technique was based on cervical screening methods and involved using a swab to detect HPV and cytological abnormalities, followed by high resolution anoscopy.
Professor Hillman said that a key stumbling block in providing this service to high risk groups more widely was funding. Professor Hillman is the only person in NSW funded to perform the service, and he has more than 500 people on his waiting list.
“We are pushing for more resources, and again we are battling the stigma and lack of knowledge of this sort of condition,” he said.
Research efforts are also focused on treatments for anal cancer precursors, he said. Pomalidomide (a derivative of thalidomide) was being investigated as a potential treatment, and a trial of a novel therapeutic cream, developed by Antiva Biosciences, was also soon to commence, Professor Hillman said.
Dr Amitesh Roy, medical oncologist at Flinders Medical Centre and senior lecturer at Flinders University, said that the International Journal of Epidemiology article highlighted the fact that even though anal cancer was a rare cancer, the incidence was increasing.
“One of the things to bear in mind is that anal cancer is an uncommon cancer, comprising just 2.5% of all digestive system malignancies. It’s a treatable cancer – most patients would present with early stage disease and 90% of these patients would be able to achieve cure with concurrent chemo-radiotherapy treatment,” he said.
Dr Roy said it was unclear if the increasing incidence of anal cancer would lead to an increase in more advanced or metastatic disease presentations.
Dr Roy is the Australian principle investigator of a multicentre trial called InterAACT [International Multicentre Open Label Randomised Phase II Advanced Anal Cancer Trial Comparing Cisplatin plus 5-fluorouracil versus Carboplatin plus Weekly Paclitaxel in Patients with Inoperable Locally Recurrent or Metastatic Disease] that is evaluating two types of chemotherapy regimens in patients who present with either inoperable, locally advanced anal cancer or metastatic anal cancer.
The trial, which is part of the International Rare Cancer Initiative, aimed to establish a standard of care for patients presenting with advanced disease, he said. More than 80 patients had been recruited to the trial, including one from Australia.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert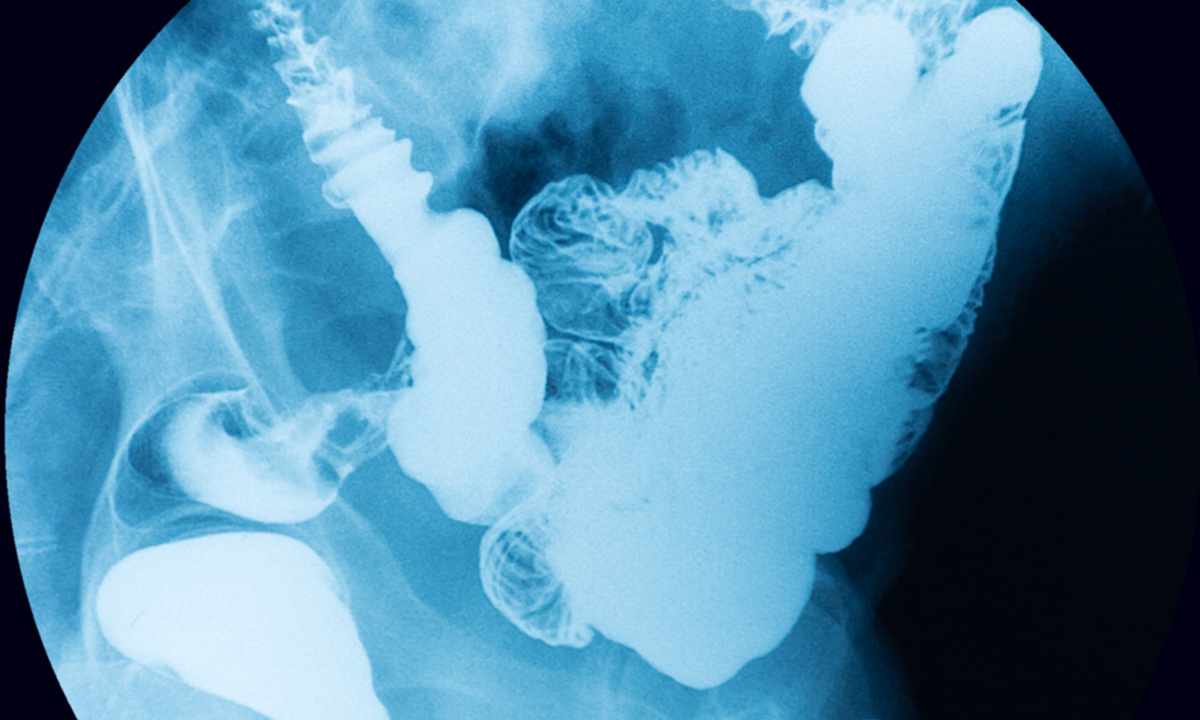
Black, JS (1986) Australian Family Physician 15:20-24 “The Medical consequences of unorthodox sexual behaviour”. (The journal’s editor of the time commissioned this article but I refused his title “…abnormal sexual behaviour”. We settled on the above. I am pleased Prof. Hilton observed the increasing incidence of anal intercourse in the heterosexual community that’s actually been going on over decades.