SPIROMETRY remains best practice for the diagnosis of chronic obstructive pulmonary disease (COPD) – the fifth leading cause of death in Australia – but a decreasing number of general practices offer it due to a lack of financial incentives, say experts.
Better access to good quality spirometry in a primary care setting would curb the misdiagnosis rate of COPD, leading to improved management and treatment outcomes for patients with confirmed cases.
Primary care workers face structural and financial barriers to conducting the lung function test. As a result, COPD is often diagnosed by a general practitioner on clinical symptoms or a chest x-ray alone.
Professor Nicholas Zwar, professor of general practice at the University of NSW, and director of the Centre for Primary Health Care and Equity, said that case finding and diagnosis remained problematic in the treatment and management of COPD.
“Getting good quality spirometry done in the primary care setting is a challenge because you need to have a reasonable amount of skill, and you also need to coach the patient to conduct the test,” Professor Zwar said.
“The Medicare rebate for pre- and post-bronchodilator spirometry offers a very poor rate of return for practices.”
General practitioner Dr Kerry Hancock, an executive member of the coordinating committee for the COPD National Program, is part of the thoracic medicine clinical review committee of the Medicare Benefits Schedule (MBS) Review Taskforce.
Dr Hancock said the committee had proposed better remuneration for spirometry as part of the MBS review.
“A lot of practices have stopped spirometry from a financial point of view, and access to spirometry from accredited laboratories is quite difficult; it’s just one more barrier in front of the patient if you send them to hospital for testing,” Dr Hancock said.
“We need to be innovative to allow GPs better access to spirometry if it cannot be done within their practice. This might include spirometry test centres such as those in the Netherlands, mobile spirometry services, or easier access to hospital services.”
The Lung Foundation’s COPD-X Plan guidelines outline the best-practice treatment and management of the condition, and are updated every 3 months in light of emerging evidence. Interventions for the treatment of COPD include smoking cessation, pulmonary rehabilitation, influenza vaccination, optimising medicines, patient education, and the effective management of exacerbations.
Professor Zwar said that while these COPD treatments were best carried out in a primary care setting, implementing appropriate management plans for patients had proven to be a challenge.
“There are clear, evidence-based treatments for people with COPD and interesting literature about the structured management of the disease with a self-management aspect,” he said.
“It’s about implementation – while self-management support programs can be helpful, it can be difficult to deliver those in primary care settings.”
A recent qualitative study into the implementation of the case finding and management of COPD with the participation of both the GP and a practice nurse found that while nurses developed technical skills through training offered in the trial, they tended to be less involved with patient treatment.
Lead author Dr Sarah Dennis said more research was needed to explore how the diagnosis and management of COPD in primary care could be optimised.
“In the study we trained the nurses to conduct high quality spirometry and to interpret the results, but there was reluctance from some of the nurses to make a diagnosis,” Dr Dennis said.
“Some felt it wasn’t part of their scope of practice, while others may have felt less confident.”
Dr Dennis said that improved primary care management of COPD by a broader health care team might ensure a greater uptake of effective interventions, such as smoking cessation and pulmonary rehabilitation.
Judy Powell, the Lung Foundation’s COPD National Program education and training project manager, said poor access to interventional therapies had an impact on patient outcomes.
“In rural and remote Australia, access to pulmonary rehabilitation is low or non-existent, which might see the development of an online tool in the future that allows patients to work through modules of self-management,” Ms Powell said.
“Sometimes programs are difficult to get to due to transport, waiting lists are long, or hospital specialists need to refer patients to the programs, setting the patient on a disability spiral.”
Ms Powell said the outcome of the Health Care Homes trial could inform the management of COPD in the future.
“Ideally we would like to see our patients with COPD have a GP that they work with and that they visit regularly, even when they are well, to get access to programs like pulmonary rehabilitation. This is one of the best evidence-based interventions to reduce hospitalisations for people with COPD,” she said.
“A key element of treatment is a care plan that the patient knows and understands how to use, which we call a COPD action plan, including how to manage medicines and education to self-manage their condition.”
Latest news from doctorportal:
- Life interrupted: young people need help moving forward after cancer
- Big pathology to get massive windfall at expense of patients, doctors
- Cancer survival in rural Australia ‘alarming’
- Most unaware of dementia lifestyle link

 more_vert
more_vert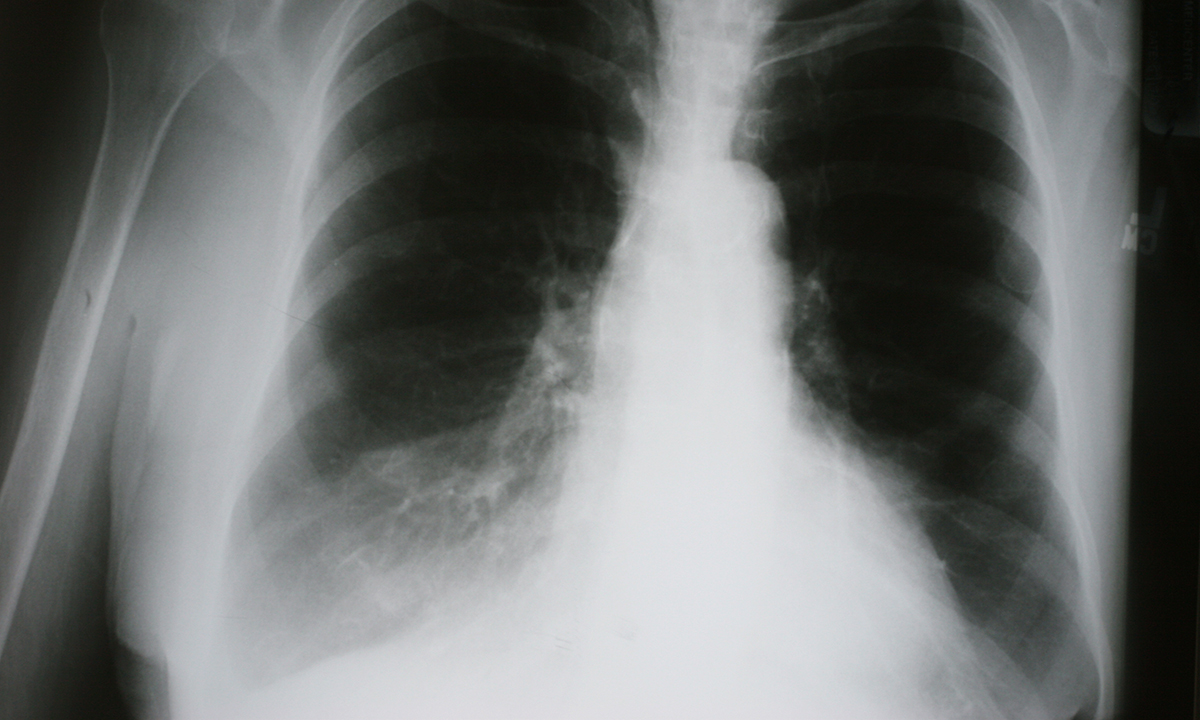
I send all my patients to a lung function lab – so no spirometry overuse is recorded against our practice- it costs a sh–t load of money to the government but protects our backside and supports our colleagues to have latest equipment- and our patients get the rolls royce treatment.
If there was a realistic spirometry rebate our practice would change to more practically cost effective method – but no doubt still watch out for the zealous investigators of the commonwealth – who will not allow best practice and the poor practitioner has to justify it.
I don’t understand why you are all stuck with the rebate concept in relation to spirometry charges. Charge an appropriate fee that covers all the costs involved. It’s not that difficult really!
I was reviewed for claiming too many spirometry readings in 2010. Figures for item 11506 claims per year, given to me are enlightening:
25th percentile 0
50th percentile 1
75th percentile 6
90th percentile 19
95th percentile 32
99th percentile 86
The item for spirometry and MBS bears no relationship to its utility. It is a barrier in requiring post bronchodilator readings when these are not always required. I and many other GP’s and specialists do perfrom spirometry without claiming. The item is thus irrational and useless for any meaningful monitoring of spirometry.
The rebate is inadequate particularly as the MBS does not allow a co-payment when bulk-billng to cover consumables and equipment costs.
This is a woeful situation for the asthma capital of the world.
An evidence-based alternative to spirometry for general practice is a COPD screening device, such as the Vitalograph copd-6 or the PiKo-6. These devices are cheap <$200) and simple to use. Both are validated as reliable screening devices for COPD in adults. The copd-6 has the advantage of calculating a 'lung age' as well, which a valuable tool for motivating smokers to quit. Every practice should consider purchasing one of these.
Soirimetry is too expensive in General Practice. The Rebate is low and we have to give over 50% of the rebate to the doctor. It takes 20 minutes of the nurses time (that costs $15) and there are disposables eg a Nebuliser mask or vilumatic and one way bacterial filters, the cost of the machine and annual calibration.
The costs mean we lose a substantial amount of money on each test. We have two spirometers but they sitting in the cupboard gathering dust.