SPINAL fusion surgeries for chronic low back pain are on the rise, despite the lack of research to back their efficacy, and experts are now calling for tighter guidelines, including a waiting period.
Dr Richard Williams, orthopaedic surgeon and spokesperson for the Royal Australasian College of Surgeons, told MJA InSight that a key regulation should be that patients must wait a period of 12 months before a spinal fusion surgery was performed.
During this time, the patient must undergo aggressive rehabilitation to try to lose weight and reduce their back pain.
“Most patients will recover after these 12 months,” he said. “It’s also the duty of the doctor to set realistic expectations for the patient, and explain that spinal fusion rarely results in having no pain at all. The surgery works for a proportion of patients, not all.”
Dr Williams was commenting on an article published online by the MJA which discussed the controversy around spinal surgery for chronic low back pain. The authors wrote that there was a continued lack of evidence when it came to the benefit of spinal fusion for low back pain.
In 1999, a Cochrane review found there were no published randomised controlled trials which established effectiveness of fusions for chronic pain. A 2005 review was critical of the outcomes measured, saying that the limited evidence on the long-term effects of either surgical decompression or fusion remained a matter of concern, given the numbers and the costs of the surgical procedures being performed.
- Related: MJA — Surgical management of low back pain
- Related: MJA — Spinal surgery and severe vitamin D deficiency
The authors wrote that patients were presenting with high expectations of modern medicine, and in many cases there were additional entitlements to monetary gains from workplace injury compensation and third-party incidents.
“There has been a lack of patient-oriented surgical outcomes, and there is a lack of outcomes for most things that we do for chronic low back pain,” they wrote.
While the spinal fusion procedure remains controversial, it would be valuable for spinal surgeons to undertake a national audit of patient-centred outcomes for the procedure, the authors concluded.
Professor Jeffrey Rosenfeld, senior neurosurgeon at the Alfred Hospital and director of the Monash Institute of Medical Engineering, told MJA InSight that there were two main reasons for the increasing rates of spinal fusion surgeries in Australia.
The first was that patient expectations of surgery can often be high, meaning they “lap up” the positive side of the story and don’t hear the negative side, he said.
Should some patients be given a choice between committing to several sessions of physiotherapy, seeing a psychologist and undertaking an exercise regimen to manage their pain, and undergoing a surgical procedure, many will choose the surgery because it feels like the easier option.
“Surgeons can also overemphasise the positives, and this gives the patient the wrong perspective about the surgery,” Professor Rosenfeld said.
Ian Harris, an orthopaedic surgeon at Liverpool and St George hospitals and professor of orthopaedic surgery at the University of NSW, told MJA InSight that the medical community found itself in a difficult position.
Randomised controlled trials were crucial, he said, and should always take place before any treatment became so frequently used. However, as this was never done with spinal fusions, researchers must now attempt to work in reverse and undertake these studies.
“Once a surgery is common place, it becomes a standard of care, and this is not questioned,” Professor Harris said.
He added there was a basic reason for why surgeons persisted in performing spinal fusion surgeries in the absence of evidence.
“Surgeons believe that it’s effective, and this belief comes from their own direct observation of patients.” However, relying on patient observations was inherently risky. “As with any other operation or treatment, we’ll always see that around two-thirds of patients seem to get better. But when there is such a poor evidence base, we can’t assume the surgery is effective,” Professor Harris said.
Professor Rosenfeld said that “the careful and considered selection of patients who may benefit from spinal surgery is the key issue here”.
Professor Harris said that when it came to clear indicators for spinal fusion surgeries to treat chronic back pain, “I don’t know of any”.
“Yes, if a patient has low back pain because they have a tumour or have been in an accident and have a dislocation, these are indicators.” However, if the patient had non-specific, chronic back pain, spinal fusion surgery was not warranted. “There are some invalidated constructs which are being used to justify intervention. The classic one is spinal instability,” he said.
Professor Rosenfeld said that for patients who do not have clear indicators for spinal fusion surgery, a multidisciplinary approach is preferable, which includes managing the psychosocial issues of chronic pain. This involves input from specialists, physiotherapists, chiropractors, clinicians, psychologists and other allied health professionals.
“We need to develop more structured, multidisciplinary pain management and raise the profile and reach of these services. This will often give people better long-term pain outcomes than having multiple spinal surgeries.”

 more_vert
more_vert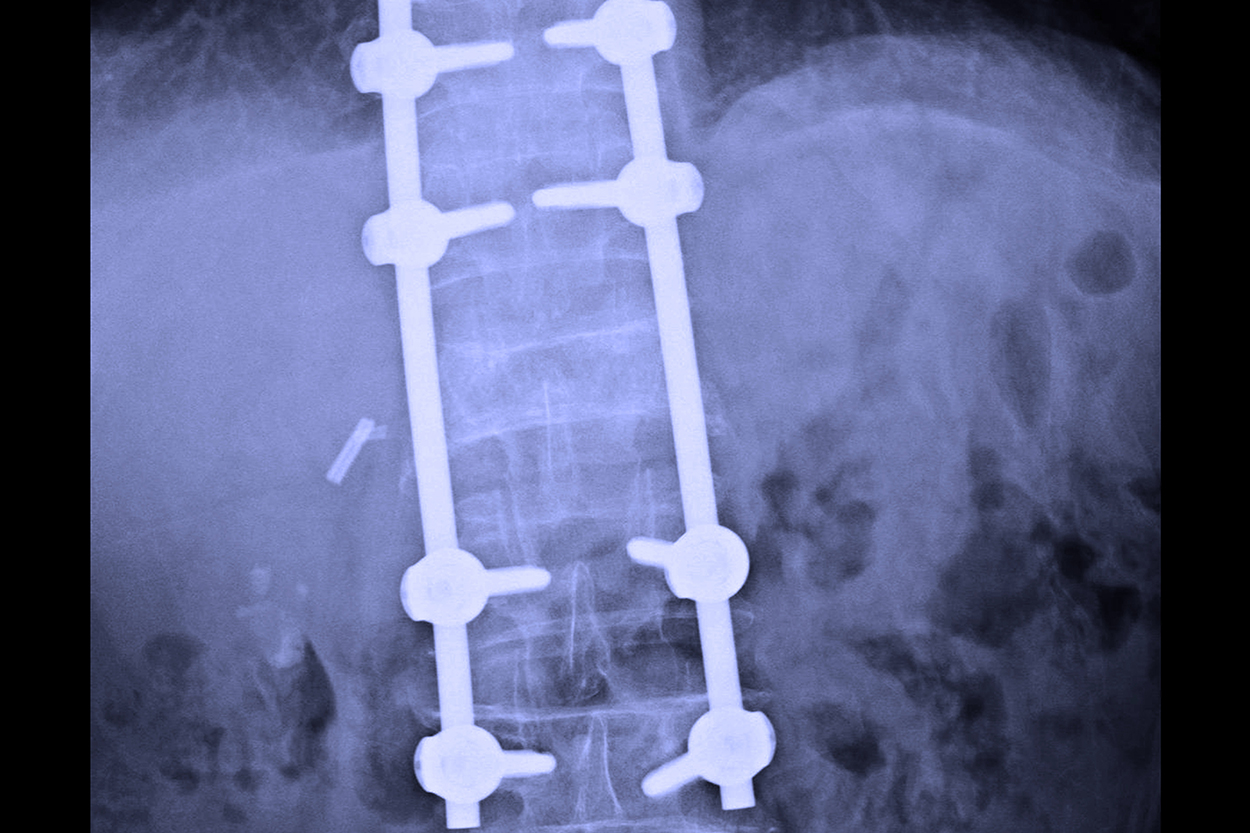
Why not…because its a SCAM…..
Spinal fusion – read faccts.
SPINAL FUSION is ineffective – regardless FACTS….45 years experience…it a SCAM…
What ever became of the call for a waiting period?
Did the orthopedic association kill this notion or just ignore it?
At 17 I first injured my back. Constant chiropractic care at best offered slight relief to a pain that kept returning. At 40 disectomy of a large herniated disc. At 41 further investigation by a very good surgeon showed two more ruptured discs or annular tears. (discography) . The surgeon refused to fuse. Triple fusion would be very risky I know. 17 years later I am still in pain. Still semi employed. Still in bed laying on heat pads. A BMI of 25. 40 years is a long time to be in pain. I am with Mathew Scott Young. Find a surgeon on top of his game. One that studies the spine to a T. They will give you the results and also say no if it cant be done. No one wants surgery. But to live without pain would be so wonderful. Incidentally, a small company where I work (10 truck drivers) there have been one with a single level fusion, one with a triple fusion!! and one with a disc replacement. All clocking up miles. Oh and one with two ruptured discs semi employed and no fusion.
Further to to my earlier correspondence in the chiro debate, the medical profession have a lot to answer for. When I went out into solo private radioloical practice in a country centre, I was asked to do the chiroprctic work. I soon became alienated by the large doses of radiation to asymptomatic portions of the spin. Disillusioned,I then gave up this part of my practice, only to find the chiros then sent their patients across the border to a very large radiology practice, which was only too happy to oblige without demur1 Shot in the back! Some of the chiros then put in their own x-ray units, so they were free to blast away at anyone coming through the front door. I then approached our Royal College, pleading for chiro work be abandoned. Result: complete silence, to my chagrin! Money talks. Patient indoctrination is also a powerful weapon.Spinal fusion then entered the fray. Whilst there must have been successes, us radiologists began to see an increasing number of patients in agony, spawning a new industry of radiologist injecting cortisone into the spine, hoping for some relief! These blokes travel around with large lists. There is so much metal in there. It is no surprise that some impinges on the odd nerve or two. Some spinal surgeons have carved out huge practices.
I am quite shocked by the controversy over the right or wrong of spinal surgery. Should surgery only be done on the merits of each individual case. I can tell you from a suffer of 10 years with chronic back pain and sciatica, that even though it has only been 5 months or so since my brilliant surgeon( Dr Williams) preformed a decompression and fusion procedure on my spine ,it has given me such relief that it is like having a new life. The pain was so constant i could hardly think of anything else and even a 5 minute walk was just about impossible. A nights sleep, totally out of the question. Yes I did wait 12 months for my surgery and i tried the physio and palates etc.. but the only way I could function was full to the eyeballs everyday with codeine. No, I am not an overweight person ( and never have been) I weigh 65 kgs. The pain killers eventually inflamed my liver and caused me very poor health. So .. What alternative do we ( public Patients) have, live with debilitating pain or have the surgery. You try it. I know what you would choose, bad reports and all. Some of the negitive comments by medico academics, who obviously are just totally blinded by just the negitive side of spinal fusion and not the benifits of the surgery which can help people live a normal life again. I was warned of ALL the risks involved and even thou I have no medical training I am not an idiot,and I know that down the track I “MAY” need surgery again ,but at the moment I am happy with the outcome of my spinal surgery even though I am not totally pain free ( which I was told would be the case) I don’t need the pain killers anymore and I am enjoying my life. Isn’t that what it is all about!
I am concerned that the opinions stated by Dr Richard Williams are done so on behalf of the RACS. It is a strong statement to be made that there must be a ‘regulated’ 12 month wait before ‘spinal surgery fusion’. Was Dr Williams speaking personally or as a spokesperson for the RACS? I would suggest that all professionals should think carefully about what they will reap in circumstances where what they sow is a total abandonment of indepedent clinical decision making for completely proscribed decision making. In the blame frenzy the easy path to hell is to blame the techology and the generic technique. What those clinicans who understand the art of spine sugery know is that it is all about patient selection (clinical indication) and the skill of the surgeon performing the technique. Failures are in most instances a failure of indication and/or technique. If the standard of the evidence accepted by the MJA of late in th artices it hs published on this topic is reflective of the level of understanding of “good evidence” by the Australian medical profession, then I am very afraid about the depths to which the profession is going to fall. Read the articles that have been footnoted, send them to some non-medico academics you know and ask them for their critque and then hear them laugh. There are many competent spine surgeons who get up every day and help people get their lives back but you can’t hear their message over the shouting of those surgeons who never learned the art of surgery and want to make their name by destroying the technique they never mastered in all its forms.
Matt – please DO “bring it on” by referring us to some valid studies.
Why dont you talk to a spine surgeon who is in practice and is up to date in Evidence Based Medicine. The levels of evidence coming out of spine journals surpasses the quality of other journals in surgery . You ask the political aspirants and the retired surgeons the same questions and all they ever talk about is liw level data . This include rubish level 3 papers that are preformed often by phd’s in a quest to publish or perish. Most of it has an inocent ignorance asocciated with it , but often agends exist . Why not ask a practicing surgeon who understands proper up to date modern spine surgies and related outcomes what he or they think about this publication . Enough of the rubbish surgeon Nd spine surgery bashing and time for a serious debate which i am happy to have with the above mention individuals . Bring it on . Also balance the argument, this time with real evidence.
Matt scott-young
spine surgeon
I am fortunate to work in an integrated practice that can offer all the assessments and treatments listed above other than having a spinal surgeon in-house (no chiropractic either). We have diagnostic equipment capable of assessing progress as well as displaying maladaptive patterns of movement patients can understand. We achieve good, but variable results depending on the patient. Pain response, commitment, expectations, long-term follow-up and money (you can’t cure chronic back pain with 5 Medicare “treatments” per year) are patient-based variables that are difficult to manipulate in the real world. Same applies to surgeons and their patients though!
I have almost never understood how fusing spinal level/s would help my patients. It can in some cases, but if we are talking degenerative disc instability, to fuse = more stress on adjacent levels and potentially more rapid degeneration, as stated above. Disc replacement surgery seems a far better option, but is currently extremely prejudiced against by every stakeholder in the medical insurance industry.
Yes patients should undertake a multi-disciplinary approach to their condition where applicable. No they should not choose fusion before an integrated approach, but that means the patient must be integrated into it as well. However, patients will always seek what they want and will pay for it as they feel appropriate.
Am I the only one who sees that pursuing a whole of disease approach places real-world patients with temporal and financial constraints in the awkward position where fusion may become a more logical alternative?
Bad news for neurosurgeons and spine surgeons.
I always wondered how 8 out of their 10 operated patients had good outcomes as stated by some of the neurosurgeons in their letters, when apperently no science is supporting these statements. I must see only the 2 out of 10 in my practice with bad outcomes all the time. Hopefully we will have soon some good science regarding spine surgeries, but that may be bad business for DB 9 and McLaren dealers.
Conservative measures should be the mainstay of therapy for back pain as surgery is not curative. If one segment of the spine is fixed the levels above and below are more effected.
As a radiologist I see so many people with little or short term relief from surgery.
I would recommend a physio specialising in back pain, weight reduction and a graded exercise program.
“Could professor Rosenfeld provide the evidence for chiropractic management of chronic back pain?”
Yes please provide the evidence
Could professor Rosenfeld provide the evidence for chiropractic management of chronic back pain?
In my personal experience spinal fusion (performed by a very experienced surgeon) has been Amazingly effective.
Prior to being able to obtain this solution I was put through Years of “Other’ treatments includng Physiotherapy, Exercise, Stretching, Cortizone and even 3 x Microdiscectomies before the surgeons would agree to perform a Fusion.
In summary my perception is that surgeons are already extremely careful to offer all sorts of alternatives before surgery so they aren’t accused of not doing so.
In addition I find that many sufferers will not consider surgery due to a perception that the success rates are low.
IMHO low overall international success rates are due to the influence of statistics of surgeons with little experience.
Easy Fix! Remove the item number for Spinal Fusion and replace it with a new number called “Multi-Disciplinary refered spinal surgery. ” The team should have Rehab, pain, psych, physio, clin pharmacology and spine surgeon. This will overcome the problems of self referral bias. Spine surgeons should be offered support to retrain in areas where there is a defined cost / QALY . Some back pain is not fixable!
if spinal canal stenosis surgery is required, the surrounding disc and vertebrae are usually severely compromised and spinal fusion stabilisation is needed.Also chronic disc prolapse in older patients often not suitable for isolated disc surgery
Conservative treatments, physio, acupuncture etc should be tried. If we get 100 people above 40yrs most of them witll show some degree of prolapse disc. That does not mean disc prolapse is the cause.