AUSTRALIA’S abortion rate could be reduced by improving access to long-acting reversible contraceptives among women who have already had an abortion, experts argue.
New research in this week’s MJA shows only 27.4% of 6348 women attending Marie Stopes International’s 16 Australian clinics said they planned to use either a progestogen-only implant or intrauterine contraceptive (IUC) after having an abortion, and only one in five actually had either device inserted immediately. (1)
This was despite 38% of respondents having a history of previous abortion, the survey of women undergoing abortions in 2012 found.
Noting that an estimated 80 000 induced abortions occurred in Australia annually, the study authors said long-acting reversible contraceptives (LARC) such as IUCs and implants could reduce unintended pregnancy by 20-fold compared with contraceptive pills, patches or rings.
They suggested that if women who had an abortion used LARC methods, it could reduce the chance of repeat abortion by 95% compared with the oral contraceptive pill, based on Scottish research.
However, the study identified cost as a likely barrier to access.
“The difference between stated intention to use a LARC and actual immediate provision may reflect the fact that women are required to pay an additional fee to have a LARC method initiated at the time of surgical and medical abortion”, the researchers wrote.
“Some women, particularly those who are younger or from areas of high socioeconomic disadvantage, may have faced difficulty finding the extra money required for upfront payment for their chosen LARC method.”
While the cost of the implant and the hormonal IUC were both subsidised by the Pharmaceutical Benefits Scheme, the copper IUC was not, costing $100–$150.
The combined oral contraceptive pill and the male condom were the most common contraceptives chosen by the women after abortion (39% and 15% respectively).
Although women under the age of 20 years were most likely to express a desire to have a LARC, women over the age of 30 years and those in the highest socioeconomic bracket were more likely to actually have a device inserted.
The researchers warned that “delayed insertion of a LARC, although sometimes unavoidable, may mean that the method is never initiated”. IUC devices could be inserted immediately in the case of a surgical abortion, but a delay of 5–9 days was necessary after medical abortions.
They concluded that public health policy needed to facilitate access to LARC methods after abortion “so that more women are able to avoid a further unintended pregnancy”.
Dr Deborah Bateson, medical director of Family Planning NSW, said while the number of women who opted for LARC after abortion was higher than the 7% uptake rate in the general community, the fact numbers were still low could reflect the “additional challenge of decision making about contraception at an already challenging time in the woman’s life”.
“We’ve really got to raise the awareness of LARC methods amongst the general community as well as in the abortion setting”, she said.
Dr Bateson said there were many myths about LARC, including misplaced concerns about infection risk with IUCs and their suitability for younger women, and overestimation of bleeding side effects with contraceptive implants and concerns they might affect future fertility.
A major challenge was improving access to LARCs at the general practice level. “GPs need to be mindful to discuss LARC when seeing a patient for a repeat pill script”, she said, adding that those who had not undergone training in IUC insertion should know where to refer patients.
“We also need to look at reimbursement for GPs for insertion of the devices, which can be a barrier to access.”
Professor Jayne Lucke, director of the Australian Research Centre in Sex, Health and Society at Melbourne’s La Trobe University, told MJA InSight that while the upfront cost of LARC might put women off initially, the devices were much more cost-effective over time than more traditional methods — both to the individual and to the health system — and were much more effective at preventing unintended pregnancy.
“Women are often unaware of the availability of LARC methods, and may simply ask their doctor for ‘the pill’ when seeking contraception”, Professor Lucke said. “This means that a discussion about the full range of contraceptive options may be circumvented.”
Meanwhile, a study in the New England Journal of Medicine demonstrated substantial reductions in the rates of pregnancy, birth and abortion among sexually active 15–19-year-old US girls and women who were provided with their choice of LARC at no cost and with appropriate education, compared with average population rates. (2)
There were just 9.7 abortions per 1000 teenagers taking part in the study, which included 1400 participants, compared with a national rate of 41 abortions per 1000 among sexually experienced US teens.
1. MJA 2014; 201: 412-416
2. NEJM 2014; 371: 1316-1323
(Photo: Saturn Stills / Science Photo Library)

 more_vert
more_vert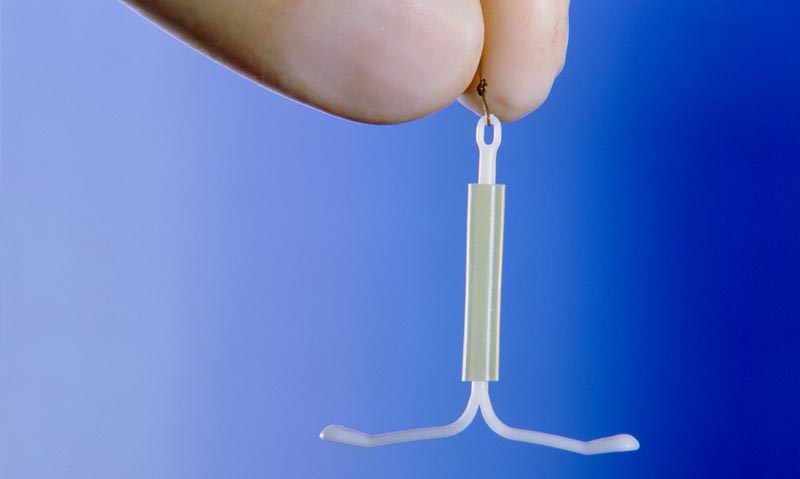
I am all for LARC. Today I inserted a Mirena. The bulk bill medicare fee I recieved was about $40. I am the only GP in my area that inserts IUDs. I counselled the patient. I used intruments that need sterilising, I used consumables like gloves etc. Specialist insert them exactly the same way for a couple of hundred dollars. I think if the medicare rebate was higher more GPs would learn the procedure, take the time and take the risk involved and patients would be encouraged by realistic reimbursement. The fee is out of proportion to the skills required, the time, the risks and the instruments etc etc.
I know, working in a lower socio-economic area, that providing contraception advice and options, particularly long acting implants etc, is not only an important part of medical treatment to discuss (it is a medication, after all) but probably one of the most useful, practical ways of improving socio-economic chances and overall well-being for my patients. If I couldn’t offer this, I jolly well should be able to refer them to someone who can.
My anecdotal experience of gp supervisors during my training was a few actively chose to not bother with LARC implant training, deeming it too complicated or a high chance of causing the patient to complain of side effects. This article shows this attitude is probably harmful to patient care (and rates of terminations).
I have found that when I am honest with my patients, and tell them that prescribing contraception does not fall under the banner of medical treatment, then it opens the Pandora’s Box of the real questions to be asked. “What is the purpose of sex?” “What is the purpose of life?”