A REANALYSIS of evidence supporting the anti-influenza drug oseltamivir has undermined confidence in published research for one of the review authors, who has called for an overhaul of the way systematic reviews are conducted.
Professor Chris Del Mar, professor of public health at Bond University, Queensland, was one of seven Cochrane researchers who reanalysed the evidence for oseltamivir (Tamiflu) using primary trial data, much of which was unpublished. (1)
They found several inconsistencies with published reports, such as that oseltamivir did not reduce hospitalisations. The reanalysis also showed a possible underreporting of adverse events, although the drug was found to reduce duration of influenza symptoms by 21 hours.
Governments globally had spent billions of dollars stockpiling oseltamivir after a previously published analysis, funded by Roche, found that the drug reduced complications and hospital admissions. However, eight out of the 10 trials used in the Roche analysis were unpublished and their data sets were not available from either the authors or Roche. (2)
The researchers postponed an analysis of zanamivir (Relenza) evidence because its manufacturer, GlaxoSmithKline offered to provide individual patient data.
The Cochrane researchers found that 60% of patient data from oseltamivir trials had never been published, a fact Professor Del Mar described as “disgraceful”.
In what Professor Del Mar believes is a world first, the researchers obtained original clinical study reports — which can run to tens of thousands of pages — by approaching national regulators, such as the European Medicines Agency and the US Food and Drug Administration (FDA).
Oseltamivir manufacturer Roche also provided data; however, the pharmaceutical company did not provide the full data despite five requests from the researchers.
Professor Del Mar told MJA InSight he believed the current system of systematically reviewing only published literature “isn’t up to the task”.
“We need to revisit that system, probably based on something more like what the regulatory authorities have, where they look at all the information and make their decision by actually querying the manufacturers’ research”, he said.
However, he acknowledged that the considerable time and manpower involved in analysing primary data was a barrier.
Professor Del Mar said that regulators such as Australia’s Therapeutic Goods Administration also needed increased funding and transparency to improve their analysis of any drug requiring significant public expenditure.
He said that drug companies should make any trial data about a drug’s efficacy and safety publicly available, although he acknowledged that early drug development information was commercial-in-confidence.
Professor Del Mar also suggested that raw data from trials could be posted online, possibly hosted by journals as an addendum to published studies. However, he said this raised questions about data ownership and the ethics of reanalysing other researchers’ data.
In an article in the BMJ, three of Professor Del Mar’s coauthors, including Dr Peter Doshi, of Johns Hopkins University School of Medicine, wrote that open access to all relevant trial data was necessary to make ethical health care decisions. (3)
“We think that full, unabridged and properly anonymised clinical study reports would be a good start”, they wrote.
The researchers — from Australia, Italy, US, UK and Japan — were unable to complete a full meta-analysis because of the incompleteness of data; however, they continue to pursue additional data from Roche and the FDA.
“We’re still grinding away getting stuff. A whole lot of hypotheses have come out of this and made us rethink things. We found all sorts of odd stuff”, Professor Del Mar said.
One of the surprising findings was that the placebo used in many of the trials actually contained active ingredients.
The research has also raised questions about the mechanism of action of oseltamivir.
“One of our team has suggested that oseltamivir’s effect might not to be due to an antiviral action but to do with a general brain suppressant … if it is working that way, then it’s no better than paracetamol but a lot more expensive”, Professor Del Mar said.
– Sophie McNamara
1. Cochrane Database of Systematic Reviews 2012; Issue 1
2. Arch Intern Med 2003; 163: 1667-1672
3. BMJ 2012; 17 January (online)
Posted 23 January 2012

 more_vert
more_vert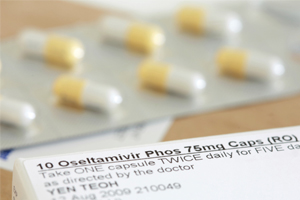
We vilify industry without acknowledging its nature. A ‘for profit’ organization must make profits, or it ceases to exist. In this competitive world, only those industries that make high profits will continue to exist. Where ethics and existence compete, which is paramount? Governments around the world have continued to slough off onto the private sector tasks they previously understood were properly the role of an independent arbiter. Politicians now obtain power, and use power to achieve partisan and irrational goals. The problem is not simply the ethics of industry (any industry). It is the ethical standard and reasonable expectation of the community as a whole.
I never use it anyway – found early on many patients, especially young adults, vomited it back too soon for it to be effective, so I have always used Relenza, and can certainly attest to it working. I have see flu sufferers so ill they had to be assisted into the rooms by a relative, who after 3 days on Relenza wanted to go back to work. Impressed me anyway. That never happened before in the days before Relenza.
We are now reaping what has been sown. Research and those undertaking it have to be independent, objective and unbiased. The problem is that far too much research both within and outside of medicine has become politicised in one form or another.
Winning research funding is as hard as winning the lottery. The only advantage for the lottery is that it doesn’t take very long to buy the ticket, compared to the hundreds of hours that are cumulatively spent preparing research protocols and getting them through funding bodies and research/ethics committees.
With heavily cash-strapped researchers increasingly turning to industry for funding any semblance of independence and objectivity is gone. Furthermore, if the results aren’t as the funding company wants they will not uncommonly claim intellectual property right and either refuse to allow the results to be published or bury them as in the above story. Likewise with government run/funded funding bodies where researchers know very well that if they provide the answers the government wants they’ll get more funding in the future and contrary views will be silenced; take as an example the arguments about climate change.
It would be wonderful to see one major and totally independent funding organisation.
A significant source of clinical trial data is the U.S. National Institutes of Health (NIH) website (http://www.clinicaltrials.gov). Since 2007, U.S. legislation mandates that information about all clinical trials that are commenced in the US must be made available on the NIH website within 2 months of the enrolment of the first patient. The sponsor or developer of the new drug must submit to the NIH data which include, inter alia, descriptive information, in language intended for the lay public, concerning the purpose of the trial, the study design, the disease or condition being studied, the name of the drug, primary and secondary outcome measures, eligibility criteria, including exclusion protocols, and the trial protocol identifier. The results of all clinical trials carried out in the US are required by law to be made available on the NIH website within 30 days of the approval of a new drug by the US Food and Drug Administration (FDA). These results must include data on participating patient demographics, withdrawals and exclusions from the final analysis, and tables of values for primary and secondary outcome measures, including statistical analyses. The NIH clinical trials database also includes reports of clinical trials sponsored in other jurisdictions when those trials have US trial arms. Some 50% of the world’s new drugs are launched in the US, so the NIH website will be a comprehensive source of detailed information on clinical trials of new drugs.
Commercial interest and the need to “publish or perish” have a lot to do with trickery in “research”. That applies not only in medicine but in other fields like climate science, and social programs where budgets may be influenced.