 THE growing incidence of methicillin-resistant Staphylococcus aureus (MRSA) in the community has highlighted the need for Australian clinical practice guidelines to be developed for its treatment, experts say.
THE growing incidence of methicillin-resistant Staphylococcus aureus (MRSA) in the community has highlighted the need for Australian clinical practice guidelines to be developed for its treatment, experts say.
Associate Professor Graeme Nimmo, State Director of Microbiology for Pathology Queensland and president of the Australian Society for Antimicrobials (ASA), said the steady increase in the prevalence of community MRSA was of national concern and all doctors and members of the community needed to be aware of it.
He said it now accounted for 15-20% of all S. aureus infections in Australia and that rate was increasing.
“The prevalence has been increasing steadily in the past decade,” he said.
Professor Nimmo, who is also chair of the Australian Group for Antimicrobial Resistance, said MRSA appeared to be under control in hospitals, thanks to infection control initiatives.
“Hospital strains [of MRSA] are not on the increase; in fact, they seem to be decreasing, but they are being replaced by the community ones,” he said.
Professor Keryn Christiansen, a past president of both the ASA and the International Society for Infectious Diseases (ASID), said community MRSA was a major problem, particularly as it was infecting young, healthy people.
It was extremely important for GPs to be aware of the big problem of community-acquired MRSA and to be able to recognise these infections, which were characterised by “a lot of pus”, she said.
“I see people who come into hospital who require drainage and they have gone to their GP who has just put them on standard anti-Staph therapy that has no effect on MRSA,” Professor Christiansen, clinical microbiologist at PathWest Laboratory Medicine, Royal Perth Hospital, WA, said.
The number one treatment was drainage of boils and abscesses, followed by broad-spectrum antibiotic therapy, culture and testing, and a change of antibiotics if MRSA was found on culture and sensitivity testing.
Strains of particular concern that were becoming more common in Australia produced a toxin called Panton‒Valentine leukocidin (PVL), which caused more severe disease with a lot of pus formation and abscesses and required drainage and a longer hospital stay, Professor Christiansen said.
“[PVL-positive MRSA] is sweeping across Australia and now accounts for around 20% of our community MRSA in WA and the vast majority of community MRSA on the east coast,” she said.
“The other major worrying side of this is that the PVL-positive clones are infecting young, healthy people … in their teens, 20s and 30s.”
Professor Christiansen said a likely outcome of the Antimicrobial Resistance Summit, to be held in Sydney on 7-8 February, by the ASA and the ASID, was the joint development of MRSA guidelines by the two groups.
The two professors were commenting on the release of the first MRSA clinical practice guidelines by the Infectious Diseases Society of America (IDSA), published in Clinical Infectious Diseases. (1)
The ISDA guidelines were mainly aimed at community-acquired rather than hospital-acquired MRSA.
They provide recommendations on the management of some of the most common clinical syndromes encountered by adult and paediatric clinicians who care for patients with MRSA infections, including skin and soft tissue infections, bacteremia and endocarditis, pneumonia, bone and joint infections, and central nervous system infections.
Professor Christiansen said the IDSA treatment guidelines were similar to treatment recommended in Australia in the Therapeutic Guidelines. (2)
However, there were some differences. For example, in Australia, oral fusidic acid was used, always in combination with other drugs, and mupirocin should be used only sparingly.
1. Clinical Infectious Diseases 2011; 52: 285-292
Posted 17 January 2011

 more_vert
more_vert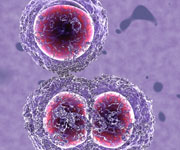
As an Australian living overseas I have only recently heard of the prevalence of CA MRSA in Oz. There is tons of literature on why and how all this has come about so I won’t repeat that here, but looking to government isn’t the answer.
To answer Robinson family’s question, yes your pets and animals can carry and re-infect you with MRSA or any resistant microorganisms. These can also be acquired in the community very easily. It is not that your hygiene standards or practices are lacking Mrs Robinson, it is simply that over the past decades greedy corporations and lazy governments have allowed business to abuse (by overuse) one of mankind’s greatest inventions ever (Antibiotics) and this is no longer the soft easy option that it was when we grew up. Our drugs are now becoming nearly useless in protecting or eradicating many of the nearly 9 million SPECIES of microorganisms out there, and scientists estimate some 15,000 new species evolve or mutate annually.
Margaret Chan (Director general of the WHO) was recently quoted as saying “In terms of new replacement antibiotics, the pipeline is virtually dry. The cupboard is nearly bare.”
The huge corporations have some blame at their feet for this in both medical and veterinary fields (more the latter) but it is just simply greed that got us here.
Unfortunately for Australia its those huge organizations that you have to rely on to find (expensive) answers because they have the politicians ‘under their wing’ and it is now near impossible for small inventive innovative businesses to get into the Australian US or UK markets via the massively expensive regulatory labyrinths. There are answers and innovations that can lead the way out but unless they are borne from Big Pharma or Big Chemi things will only get worse.
I speak from experience here.
Using current drug technologies and old hygiene standards and practices will not resolve these new problems. It is a new enemy, and new battle and in some ways this takes us back to the 1800s when people barely had good hygiene practices at all. That is to say that society didn’t really change its habits much until lots of people were dying from the plagues & diseases etc. Our societies might need to re-look at the concept again, because we have new very real killers out there that we have no easy pills for.
We can kill MRSA & resistant microbes, the technologies exist today. We just have to wake up and realize that our habits and concepts of what hygiene is, is about to change significantly. Look for biopolymer based sanitizers & soaps etc. however I doubt you can buy them in Australia yet, but MRSA and the like are easily wiped out by them as they emulate natural components of immune systems. They are also not toxic nor sensitizing to animals or human cells. It’s just one sure way you can ensure some protection for now if you have access to these technologies. Unfortunately you’ll probably have to wait many years until the big corps get their own products out in the Ozzie market. We started on doing it in Asia some 9 years ago and have no hope of bringing it to Oz unless things drastically change.
I know this story is old but am hoping someone in the health industry may offer some hope. I was a fit (running km’s each day) otherwise healthy woman until earlier this year. I got an infection on my heel, was prescribed antibiotics but with no response. Presumed to be a spider bite (live in tropical area). On day 10 after first lump surfaced was admitted to hospital with 2 abscesses, involving tissue, archilles etc put on IV antibiotics. Day 4 in hospital finally diagnosed with MRSA, was 1 day post op to drain/clean. Moved pronto to isolation! Day 5 (less than 24hrs on correct IV antibiotics) discharged at 8am. Prescribed cleocin upon discharge, administered stop/start for 5weeks, first 4 weeks at double dose i.e. 2 tablets 4 times/day. Literally took months for op wound to close over. One child then also infected with MRSA 2 weeks post op. Prescribed same medication at regular dosage. Responded well. No infections for 9 weeks. As I type, partner diagnosed 4days ago, child diagnosed with second infection today. Both on Cleocin regular dosage. Child’s infection involving eyelid, can hardly see for the swelling. I’m very very concerned. GP is at a loss to explain why we have been struck down with this. No family illness. No pre-existing wounds/injuries. All very healthy with minimal antibiotic use in our lives. Not immune suppressed, no hospital stays etc. I’m beginning to get very very worried, seems to be very little answers available. Home hygiene is impeccable yet this is still being transmitted. Should I be pressing for more advice/help? Should I be pressing for more answers? I think the level of concern isn’t in line with what I have informed myself via medical journals/govt fact sheets etc. Should I be bypassing the GP & going back the the regional hospital that I was admitted to? Also, I’ve read dogs can carry this. Could our dog be the one re-infecting us? Any advice would be most appreciated. Trying not to feel overwhelmed but something is not making sense here, we don’t seem to fit the “normal criteria” of those at higher risk. This seems to be CA-MRSA, why are we being affected with abscesses, why are our bodies unable to cope with being exposed to this? Apparently carriers are common within the community. Please help.
Could Professor Christiansen explain why mupirocin, which I was taught to use for MRSA, should be used only sparingly. Query, not criticism.
Our experience exactly. I work in country NSW, where CA-MRSA has gone from nil in 2000 to 27% of all S.aureus isolated in 2009. Of shared concern is the greatly increased number of otherwise healthy young patients who are now being hospitalised for surgical management.
Keryn mentions the Theraputic Guidelines. Very sadly the updated section (2010) on CA-MRSA and skin infections has been moved from Antibiotic to Dermatology, making it unavailable to those who use the printed version. Equally sad is the lack of leadership in the public health arena to seriously tackle this increasing problem. We have had four deaths so far… how many more do they need before becoming proactive?