HYDROXYCHLOROQUINE has never had more scrutiny than during the coronavirus disease 2019 (COVID-19) pandemic. As COVID-19 case numbers grew, the promise of a pharmacotherapeutic panacea to the world’s problems led to exponential growth in interest in a drug not used to attention. While enthusiasm has now been slightly curbed, the real negative impacts have raised questions as how to encourage appropriate prescribing.
Although originally used for malaria, hydroxychloroquine’s primary use is in autoimmune diseases. It is currently registered for rheumatoid arthritis, where it is an important part of standard combination therapy, and lupus. In systemic lupus erythematosus (SLE), it has unparalleled utility in preventing flares and subsequent hospitalisation, and is used universally in the absence of contraindication. This has encouraged prescribing in related conditions, including antiphospholipid syndrome, primary Sjögren syndrome, and palindromic rheumatism, although hydroxychloroquine’s inefficacy in hand osteoarthritis flags its capacity for failure.
Despite hydroxychloroquine displaying antiviral effects in in vitro studies, clinical outcomes in viral infections such as dengue and Chikungunya and in coronavirus-caused diseases such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) have been disappointing. Similar in vitro anti-viral efficacy against SARS coronavirus 2 (SARS-CoV-2) encouraged hydroxychloroquine use in COVID-19, often in combination with azithromycin. Early data were, however, of very low quality, with methodological concerns raised such as small subject numbers, poor study design including the absence of appropriate controls, and end points of unclear utility.
Possibly with the justification of rapid dissemination, many of these data were disseminated without any peer review or scrutiny on preprint servers, or with peer review called into question. This nevertheless captured media attention. Such data provided justification for political promotion of a “wonder drug” at a time when optimism was in short supply. Subsequently, better evidence has shown no benefit associated with hydroxychloroquine in COVID-19 (here and here). Randomised controlled trials are recruiting, but perhaps generate data too slowly to compete in public discourse. Additionally, the World Health Organization called a “temporary pause” on the hydroxychloroquine arm of its global clinical trial “while the safety data is reviewed by the data safety monitoring board”.
Political commentary initially suggested patients with lupus were not developing COVID-19 as a consequence of their hydroxychloroquine use. The COVID-19 Global Rheumatology Alliance physician-reported registry has so far captured 80 patients with SLE who developed COVID-19, and reported that patients taking hydroxychloroquine did not have differing rates of hospitalisation or supported ventilation, demonstrating that patients with SLE are not universally protected by hydroxychloroquine. This strong counterargument from real-world data has sadly been insufficiently heard.
Similarly, it has been suggested that little is to be lost from trying hydroxychloroquine in COVID-19. Two major concerns exist: the safety of those receiving it for COVID-19, and the risk of depriving patients with autoimmune disease the unique benefits of hydroxychloroquine. Hydroxychloroquine and azithromycin combined in COVID-19 are associated with increased risk of QTc prolongation, cardiac dysrhythmias, and death. Although confounding by indication in patients with underlying COVID-19-related myocarditis or comorbidities might contribute, so too might the higher doses required to achieve hydroxychloroquine concentrations proposed necessary for its antiviral effect. In the absence of proof of efficacy in COVID-19, these potential risks cannot be dismissed at this time.
In response to warnings of drug shortages, the Therapeutic Goods Administration and the Pharmaceutical Benefits Scheme acted to restrict hydroxychloroquine prescribing to preserve its supply for established indications (here and here). This should be applauded, but many patients with autoimmune diseases still report ongoing difficulty sourcing hydroxychloroquine, presumably due to altered global supply chains and aberrant prescribing, with consequent potential for real harm to these patients. If we have hydroxychloroquine stockpiles in Australia, shouldn’t patients with autoimmune diseases have access?
While the issue of hydroxychloroquine may have become politicised, and in the flurry of a medical crisis the principles of appropriate prescribing are easy to forget, as health professionals we should learn from the sobering reality of this case. In the cold light of day, hydroxychloroquine’s promise is dissipating, and the implications of hype are hard to ignore. This will happen again, so how can we prepare?
While as prescribers we should do better, our system needs change – to anticipate problems and boost better practice. Can we make it easier to enrol patients in clinical trials by centralising and streamlining ethical approval and governance? Could synchronised electronic systems rapidly report large-scale real-world outcomes? How can we coordinate national pharmaceutical stock levels better, to manage the next shortage? How can we proactively promote sensible medical discussion in a contemporary media landscape?
This will take broad consultation, bright ideas and political determination, but crises can catalyse change. As we venture further into the challenge of pandemic pharmacotherapeutics, it is wise for us to remember the lessons about appropriate prescribing that hydroxychloroquine has left us with.
Dr David Liew is a rheumatologist and clinical pharmacologist at Austin Health in Melbourne, where he leads the Medicines Optimisation Service. He is also the Australian regional lead for the COVID-19 Global Rheumatology Alliance.
Dr Darren Roberts is a Consultant Physician working in clinical pharmacology/toxicology and nephrology at St Vincent’s Hospital Sydney and Sydney Children’s Hospital Network. He is a Conjoint Associate Professor at the University of NSW. His research interests are in the broader fields of therapeutics, evidence-based medicine and pharmacokinetics.
Professor Catherine Hill is a Consultant Rheumatologist at The Queen Elizabeth and Royal Adelaide Hospitals, and Clinical Professor at the University of Adelaide. She is a Member of Pharmaceutical Benefits Advisory Committee with research interests in musculoskeletal epidemiology.

 more_vert
more_vert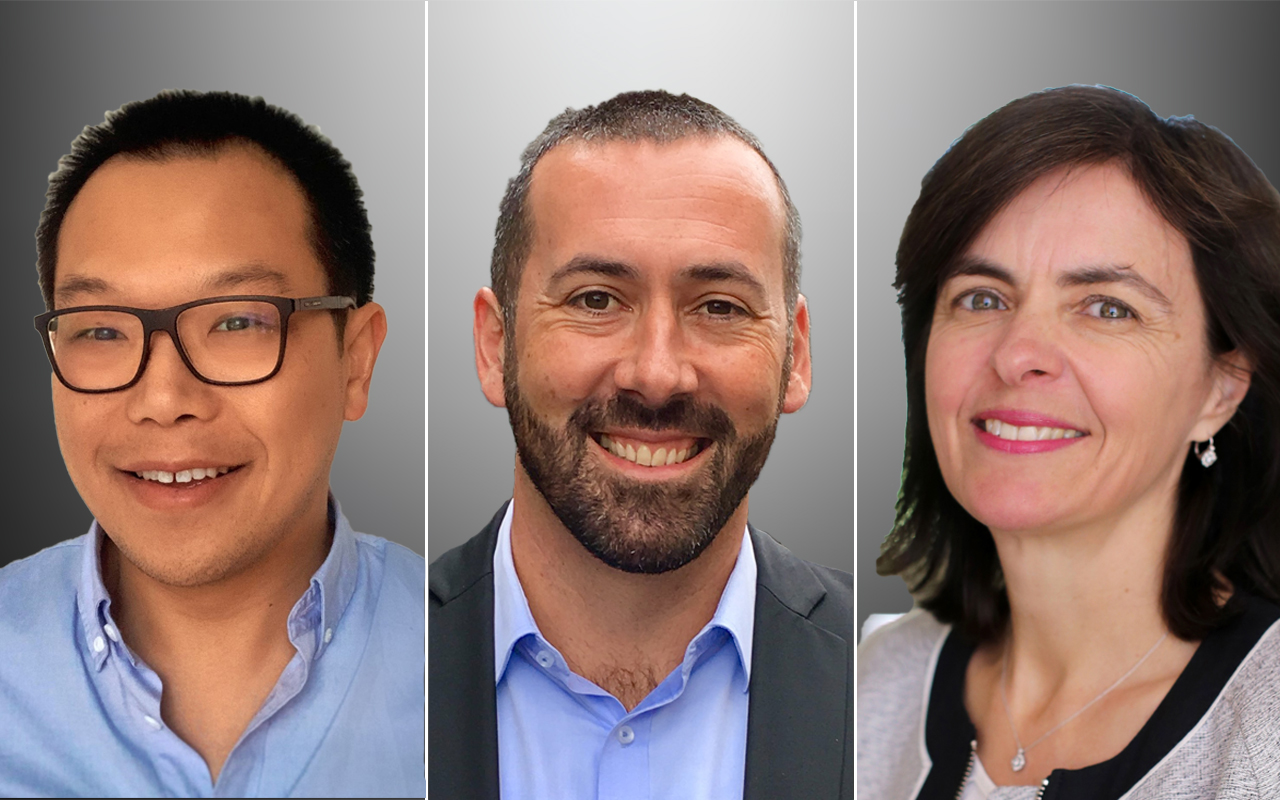
Please forward to the real Donald Trump
Very informative and well-written article.