The findings of the study by Sarah McNab and colleagues (March 28, p 1190)1 showed a substantial effect of isotonic fluid maintenance in children admitted to hospital. In the study, the number of patients who received emergency surgery between the two study groups, isotonic hydration with 140 mmol/L of sodium and hypotonic hydration with 77 mm/L of sodium, was significantly different (67 [20%] of 338 patients in the isotonic group vs 92 [27%] of 338 patients in the hypotonic group, p=0·02). I believe that this difference might have caused the difference in the number of patients with hyponatraemia because of the following reasons: the release of antidiuretic hormone is stimulated by surgical stress (eg, pain, narcotic use, and blood loss), which is experienced by many children undergoing surgery;2 previous studies3,4 suggest that the presence of hypotonic intravenous fluid during the perioperative period is associated with an increased risk of hyponatraemia; and the results of McNab’s study suggest that the risk of hyponatraemia might be greatest in the first 6 h of the study period in both treatment groups.
Preference: Surgery
1175
[Case Report Comment] Putting raised intraocular pressure in context
In The Lancet, Miles Kiernan and colleagues1 report an unusual case of a patient who developed sight-threatening ophthalmic problems after upper arm surgery. The ipsilateral symptoms and signs in this case (red eye, proptosis, limited eye movements, raised intraocular pressure, and retinal haemorrhages) are all classic presenting features of orbital venous hypertension. The most common cause is an arteriovenous fistula in the cavernous sinus and ophthalmologists are well aware of the need to investigate this possibility in any patient presenting with a unilateral red eye and raised intraocular pressure.
[Articles] Breakdown of simple female genital fistula repair after 7 day versus 14 day postoperative bladder catheterisation: a randomised, controlled, open-label, non-inferiority trial
7 day bladder catheterisation after repair of simple fistula is non-inferior to 14 day catheterisation and could be used for management of women after repair of simple fistula with no evidence of a significantly increased risk of repair breakdown, urinary retention, or residual incontinence up to 3 months after surgery.
‘Cracking good’ team supports life of service
A rural GP with a “cracking good” health team and a life-long fascination with the life of birds is among AMA members recognised in the 2015 Queen’s Birthday honours.
Dr David Hollands who, with his wife Margaret, has lived and worked in the east Victorian town of Orbost more than 50 years, was awarded a Medal of the Order of Australia for his many decades of service to his community, as well as his enormous contribution to ornithology.
In an interview with his local newspaper, the East Gippsland News, Dr Hollands recalled how, when he and his wife first arrived in Orbost not long after migrating from Britain, local doctors were expected to do “almost everything”, from delivering babies and stitching up cuts to dealing with major trauma cases.
“There was nothing like the air ambulance or helicopter evacuations,” he told the East Gippsland News. “People expected that the local doctor would cope with almost everything.”
Dr Hollands was among 20 GPs, specialists, researchers and educators recognised for their significant contributions to the health of the community and their services to medicine in the Queen’s Birthday Honours List.
AMA President Professor Brian Owler said the diversity and breadth of the accomplishments cited in the awards were testament to the significant contribution to the community made by medical practitioners every day.
Among the recipients is South Australian GP Dr Anh-Tuan Ngo, who had been a doctor in the South Vietnamese army and came to Australia as a refugee with his family in 1984. Since arriving in Australia, Dr Ngo has worked tirelessly, not only to look after his patients, but to serve the local Vietnamese community and support other veterans of the Vietnam War.
Another to be made a Member of the Order of Australia was Victorian GP Dr Barry Christopher who, in addition to his work as a doctor, campaigned for decades to advance Indigenous rights.
In the late 1950s Dr Christopher became President of the Victorian Council for Aboriginal Rights, and was a founding member of the Federal Council for the Advancement of Aborigines and Torres Strait Islanders.
Dr Hollands’ experience is indicative of how important is the role performed by many doctors in their community.
Working in an area that included 35 saw mills as well as major interstate roads, Dr Hollands and his wife – also a doctor – saw plenty of horrific accidents.
“Industrial health and safety was non-existent and alcoholism was absolutely rife – people would arrive at work on Monday still half pickled. So we had an enormous amount of trauma,” he said, adding that the number and severity of road accidents they attended were “just incredible”.
He recounted how 35 people were injured when a tourist bus overturned late at night, and he and another doctor worked for 48 hours straight at the Orbost Hospital, “non-stop setting fractures and sticking tubes in chests and sewing people up”.
Asked about his award, he said that although receiving it was “very nice”, much was due to a “cracking good team”, including his wife, two other doctors and devoted and capable nursing and surgery staff.
In addition to his medical work, Dr Hollands has also been recognised for his enormous contribution to the study of birds.
He told the East Gippsland News of his life-long fascination with ornithology, and his is the author of numerous books including Owls, Frogmouths and Nightjars of Australia, Owls – Journeys Around the World, and Kingfishers and Kookaburras.
“I’ve been a fanatical birder since about eight, so I’m getting an award for something I really love doing,” Dr Hollands said.
Professor Owler said Dr Hollands, Dr Ngo and Dr Christopher were examples of the major contribution made by many AMA members to aspects of life well beyond medicine, and were deserved recipients of Queen’s Birthday Honours.
Adrian Rollins
Insurance premium hikes waved through by Minister
Health Minister Sussan Ley did not challenge or knock back some of the biggest premium increases proposed by health insurers in years, it has been revealed.
Government officials have told a Senate Estimates hearing that Ms Ley did not reject any premium increases proposed by insurers prior to announcing approval for an average 6.18 per cent rise this year, following a 6.2 per cent hike in 2014.
Private Health Insurance Administration Council (PHIAC) Chief Executive Officer Shaun Gath told Labor Senator Jan McLucas that Ms Ley had not required any insurer to “show cause” for proposed rate hikes, or to make them re-submit a proposal.
But Mr Gath said this was because of an exhaustive process of investigation, negotiation and assessment undertaken by the Council before making recommendations to the Minister regarding premium increases.
He told the hearing that PHIAC assessed premium pricing according to three criteria: ensuring that insurers were raising sufficient revenue to remain financially viable; that the proposed price hike accurately reflected growth of business costs; and that the increase was competitive in the insurance marketplace.
Mr Gath said this approach, which had evolved in the past three years, involved “a lot of transparency, a lot of contact with the industry, a lot of clarity about our expectations, and also a very strong adherence to a competition-based model of pricing”.
“It has become quite a complex and sophisticated process which goes much longer than a simple exchange of paper in a flurry before Christmas.”
He said the proof of the success of the process was exactly that no proposed increases were challenged or rejected by either PHIAC or the Government.
“The reason that there was no return or show cause was that the process was designed to not to allow that to occur, because everybody knew…exactly what sort of pricing would be supported by PHIAC in its recommendation to the Government,” Mr Gath said.
This year’s increase, which came into force in April, drew criticism from the Opposition and consumer groups who complained that the average premium was growing a several times the rate of inflation.
The hike in premiums has fuelled concerns many consumers will downgrade their policies, leaving them with inadequate cover.
While the proportion of Australians with private health cover is growing – more than 47 per cent of the population had private hospital cover last year – doctors are worried that as premiums rise, more are opting for policies with multiple exclusions that often do not provide the benefits that they need.
AMA President Professor Brian Owler said the growth of such policies concerned the medical profession because they saw the consequences for their patients.
“Too often my members see patients who think they have cover, but don’t, because they purchased a cheaper product several years ago,” A/Professor Owler told a private health insurance conference late last year. “Treatment is planned, surgery is booked, only to be cancelled shortly beforehand because the patient is not covered.”
The AMA’s concerns have been echoed by the Private Health Insurance Ombudsman, who recently reported that policies with exclusions and restrictions regarding hospital-based treatment were a significant cause of consumer complaint.
The Ombudsman reported receiving almost 350 complaints about benefits in the 12 months to September last year, up from a little more than 250 in the same period a year earlier.
“There is demand from consumers for more affordable policies, particularly from younger people who may be taking out a policy for the first time, and from people who are purchasing health insurance primarily for tax purposes,” the Ombudsman said. “One way insurers can reduce the cost of a policy is by restricting or excluding certain treatments on the policy.”
Adrian Rollins
Australia’s hospitals 2013–14: at a glance
Australia’s hospitals 2013–14 at a glance provides information on Australia’s public and private hospitals. In 2013–14, there were 9.7 million hospitalisations, including 2.5 million involving surgery. Public hospitals provided care for 7.2 presentations to emergency departments, with 74% of patients seen within recommended times for their triage category and about 73% were completed within 4 hours. This publication is a companion to the 2013–14 Australian hospital statistics suite of publications.
Sickest, smallest to be hit hardest by Commonwealth cuts
The Federal Government has been warned that more people are likely to die because of an increasing shortfall of thousands of doctors, nurses and other health professionals in public hospitals as a result of Commonwealth cutbacks.
AMA President Associate Professor Brian Owler said the Abbott Government’s decision to reduce public hospital by $57 billion over 10 years would have a devastating effect on the State and Territory health systems.
“The AMA has warned of a perfect storm if funding is not increased,” A/Professor Owler said. “We already see hospitals struggling to achieve performance targets. We know that overcrowding, we know that delays in getting into a bed from the emergency department, is not just a matter of the headlines, it is matter of increased morbidity. People have more complications or are more likely to die if they spend more and more time in an emergency department.”
The AMA National Conference was told that in Queensland alone, the Federal Government’s decision to slash growth in public hospital funding from 2017 will rip $11.8 billion out of the State health system over 10 years, resulting in 1503 fewer doctors and 5319 fewer nurses being employed in the time.
A/Professor Owler said the outlook for the smaller states and territories, which had limited revenue-raising capacity, was particularly worrying.
“I really fear for those states, because we know that their economies are quite small. They don’t have the ability to make up the shortfall in revenue, and those states are going to be really badly affected,” he said.
Queensland Health Minister Cameron Dick told the AMA National Conference that the Commonwealth was shoving more of the burden of public hospital funding on to the states.
Mr Dick released modelling by his Department showing that the Commonwealth’s share of national efficient public hospital expenditure would peak at 35.5 per cent in 2016-17 before rapidly falling away to just 32.1 per cent by 2024-25 – virtually 10 percentage points below the level committed to in the 2011 National Health Reform Agreement.
“There will be greater pressure on the hospital system as a result,” the Queensland Minister said. “People will have to wait longer for surgery, people will have to wait longer for patient appointments. We will not be able to deliver the services we need. As the population gets older and costly medical technology increases, there will be a gap.”
AMA Tasmania President Dr Tim Greenaway described to the AMA National Conference how the Commonwealth funding cut would hit his State particularly hard.
Tasmania has the nation’s oldest, fattest, poorest and – by many measures – least healthy population, and Dr Greenaway warned the Federal Government’s policy would only make the situation worse.
Despite having greater health needs than most other states and territories, Tasmania’s spending on health care ($1275 per capita) is below the national average ($1735 per capita), and Dr Greenaway said the Commonwealth’s funding cuts would only “lock in” the State’s inadequate investment in health, “which will inevitably increase health disparity”.
The states and territories are furious the Federal Government has walked away from its commitments under the National Health Reform Agreement, and the issue is set to be near the top of the agenda when Prime Minister Tony Abbott meets with his State and Territory counterparts to discuss reform of the Federation at a leader’s retreat in July.
A/Professor Owler said the Federal Government’s decision was indefensible.
“It’s up to the Commonwealth to live up to its responsibility to make sure that all Australia’s get access to the services they deserve,” he said, adding that the squeeze on hospitals would also have a significant effect on doctor and nurse training.
A video of the Quality public hospital services: funding capacity for performance policy session can be viewed at: media/ama-national-conference-30-may-2015-session-1
Adrian Rollins
Quality selection, training vital to safeguarding GP future
By Dr Penelope Need, Director of General Practice training at Southern Adelaide Local Health Network; tutor in Medical Professional and Personal Development, University of Adelaide; Partner, Pioneer Medical Centre, Tea Tree Gully, South Australia.
General practice training is having its first shake up since the implementation of the training providers more than 10 years ago.
The last couple of years have seen large numbers of applicants. General practice is a specialty of choice for many junior doctors. We need to keep it that way.
Quality general practice training is mandatory if we wish to maintain high standards in primary care.
General practice is a challenging career. Future GPs need to be carefully selected and trained to a high standard.
We all know that primary care is the most cost effective area of the health system. Why then is it being targeted for so much reform?
I have a tutorial group of nine year 3 medical students, none of whom have a GP. If these carefully selected medical students don’t see the value in general practice then how can the rest of the community?
At interviews, potential GP registrars can tout “continuity of care”, but is this still a reality?
Access is a real issue in general practice at the moment. Chronic disease management, and an aging and increasingly overweight and mentally distressed population puts a strain on well-meaning general practitioners.
The current model of funding rewards throughput. Is this what we want to see into the future? Are we going to be palliating our own patients or leaving it to the ambulance officers?
Pharmacists are providing vaccinations, physiotherapists are requesting referral rights. Why? How has this gap been created that someone wants to fill?
That other catch cry of general practice, “holistic care”, is also under threat.
The solution to these problems starts with selection. We need to select appropriate individuals. Selecting rural students has been shown to increase rural retention.
We then need to ensure they are adequately trained.
The loss of the Prevocational General Practice Placements Program is a real blow for general practice. It was vital for improving inter-professional communication and respect. Emergency, medicine and surgery are all mandated in internship. Why not primary care? Like anything, until you are exposed to general practice you do not understand the complexity and the challenges.
The AMA is looking at alternative models of reviving prevocational exposure to general practice. I personally feel this is vital for the ongoing health of the profession.
Just because we have a lot of applicants for general practice training does not mean that we will have a lot of quality GPs in another three years. We need to select the right people for the job and train them to a high standard.
Maybe a litmus test – would you be happy to be treated by doctors trained under this program? Don’t be like my third year medical students – everyone needs a good GP. Let’s just hope there will be enough to go around.
Warfarin-induced skin necrosis following recommencement of warfarin after perioperative Prothrombinex-VF
Clinical record
A 62-year-old man with thrombophilia was receiving warfarin for recurrent venous and arterial thrombosis, and had a known 48 mm diameter infrarenal abdominal aortic aneurysm (AAA). He presented with collapse at home after 2 days of increasing pain in the left flank. A left-sided retroperitoneal haematoma was identified by computed tomography angiography. Increasing abdominal pain and a decline in haemoglobin levels from 125 g/L to 88 g/L made it necessary to transfer the patient urgently to theatre for exploration and open repair of a presumed ruptured AAA.
The patient had been taking 1.5 mg warfarin each day for 20 years without complication. He was known to be heterozygous for both the factor V Leiden and the prothrombin G2021A mutations. He was a current smoker with a 40-pack-year history who also had mild rheumatoid arthritis, insulin-dependent type 2 diabetes mellitus, stage 3A chronic kidney disease, moderate aortic stenosis and hypertension.
Before surgery, anticoagulation with therapeutic warfarin (international normalised ratio [INR] 2.5) was reversed according to our unit protocol with 5000 IU Prothrombinex-VF (CSL Behring Australia). A posterior rupture of the AAA was confirmed during the operation. Sodium heparin (5000 U) was administered before aortic cross-clamping, and its action was fully reversed at the end of surgery with 50 mg protamine sulphate.
Recovery was initially uneventful, and therapy with 1.5 mg warfarin was resumed on postoperative day 1, together with a renally adjusted dose of enoxaparin sodium (40 mg twice daily).
On postoperative day 5, the patient experienced increasing abdominal pain and was returned to theatre for an exploratory laparotomy; nothing significant was found. His INR was 3.1, and reversal of anticoagulation was not performed.
On postoperative day 8, he was transferred to the intensive care unit because of deteriorating gas exchange, hypotension and an evolving coagulopathy. Large and painful areas of skin necrosis had developed on the abdomen, flanks and thighs (Figure, A). His INR was 6.2, activated partial thromboplastin time (APTT) 64 seconds, fibrinogen levels 1.0 g/L, and platelet numbers had dropped from 265 × 109/L to 123 × 109/L.
Seven units of fresh frozen plasma and 10 units of cryoprecipitate were infused. Warfarin treatment was withdrawn, and anticoagulation therapy with intravenous heparin initiated (target APTT: 65–100 seconds) to treat the presumed warfarin-induced skin necrosis (WISN).
The results of an enzyme-linked immunosorbent assay (ELISA) test for heparin-induced thrombocytopenia were negative, as was screening for vasculitis-related antibodies. Anti-cardiolipin and anti-β2 glycoprotein I antibodies were not detected, nor was lupus anticoagulant. Protein C and S levels were low (0.45 U/mL and 0.53 U/mL, respectively).
The skin lesions continued to demarcate over the next 2 days, and were debrided on postoperative day 10 (Figure, B). Histopathological findings were consistent with WISN (Figure, C).
Anticoagulation treatment with intravenous heparin continued for 2 weeks, and was then changed to enoxaparin sodium (100 mg twice daily).
The skin lesions were regularly debrided and negative pressure dressings applied during the following months. Autologous split skin grafts were later performed with excellent results (Figure, D, E), and the patient was transferred to our rehabilitation facility on postoperative day 63. Treatment with oral rivaroxaban was initiated when he was discharged from hospital, and is to continue indefinitely at a dose of 20 mg daily.
Warfarin-induced skin necrosis (WISN) is a rare complication of a commonly used medication. The underlying mechanism is unclear, but it is thought that WISN is induced by a transient paradoxical hypercoagulable state.
Warfarin inhibits certain vitamin K-dependent factors more quickly than it does others, producing a transient imbalance in procoagulant and anticoagulant activity.1 The anticoagulant activity of protein C is rapidly reduced (within 24 hours) because of its short half-life (5–8 hours). The levels of other vitamin K-dependent coagulation factors (II, IX and X) decline at slower rates because they have longer half-lives (24–72 hours). The initial result, therefore, is a relative increase in thrombin generation and a transient hypercoagulable state that may lead to thrombotic occlusion of the microvasculature and thus tissue necrosis.
Our patient had several risk factors for WISN, including his age, obesity and a history of thrombophilia. Further, he was heterozygous for the factor V Leiden mutation (resulting in activated protein C resistance and a functional protein C deficiency) and for the prothrombin G2021A mutation (resulting in elevated prothrombin levels).2 Hypercoagulable conditions more commonly associated with WISN include deficiencies of protein C, protein S and antithrombin III. Other recognised predisposing factors include being female and being given higher loading doses of warfarin.3
The potential role of Prothrombinex-VF in the development of WISN in our patient warrants further consideration. In Australia, immediate warfarin reversal is achieved by using prothrombin complex concentrates or fresh frozen plasma. Prothrombinex-VF is the only prothrombin complex concentrate routinely used in Australia and New Zealand. It is a three-factor concentrate (prothrombin II, IX and X), including low levels of factor VII, but does not contain proteins C or S.
Our unit protocol for immediate warfarin reversal at the time of this patient’s admission reflected the recommendations published in 2009 by Chiu and colleagues.4 Our patient received Prothrombinex-VF alone; neither vitamin K nor fresh frozen plasma were used during reversal. We hypothesise that protein C and S levels were low at the time of his operation, as Prothrombinex-VF does not reverse the reduction of protein C and S levels caused by warfarin. Perioperative blood loss would have reduced their levels further, and the resumption of warfarin treatment immediately after the operation would have depleted them even more. We therefore suggest that very low levels of proteins C and S, together with his pre-existing thrombophilia, are likely to have tipped the balance in favour of thrombosis.
A recent update of the consensus guidelines for warfarin reversal in Australia suggested that 5–10 mg vitamin K1 be given parenterally at the same time as Prothrombinex-VF.5 The half-lives of the infused clotting factors are similar to those of endogenous clotting factors, but the addition of vitamin K1 (as a cofactor in their synthesis) would sustain the reversal effect. It may also increase protein C and S levels, and thereby avoid a transient prothrombotic state when treatment with warfarin is resumed.
Our case highlights the importance of being aware of WISN as a rare complication of warfarin therapy. Consideration of individual patient factors, including a history of thrombosis, before initiating warfarin reversal is critical for ensuring that appropriate adjuvant therapy is provided and an optimal outcome achieved. Vitamin K1 should be administered with Prothrombinex-VF during warfarin reversal, as it sustains the reversal effect, may increase the levels of proteins C and S, and thereby avert thrombotic complications.
Lessons from practice
- Individual patient factors, including a history of thrombosis, must be considered before warfarin reversal.
- Updated consensus guidelines for warfarin reversal suggest giving vitamin K1 with Prothrombinex-VF.
- By increasing protein C and S levels, vitamin K1 may prevent a transient hypercoagulable state after resuming warfarin therapy.
Warfarin-induced skin necrosis and results following autologous skin grafts
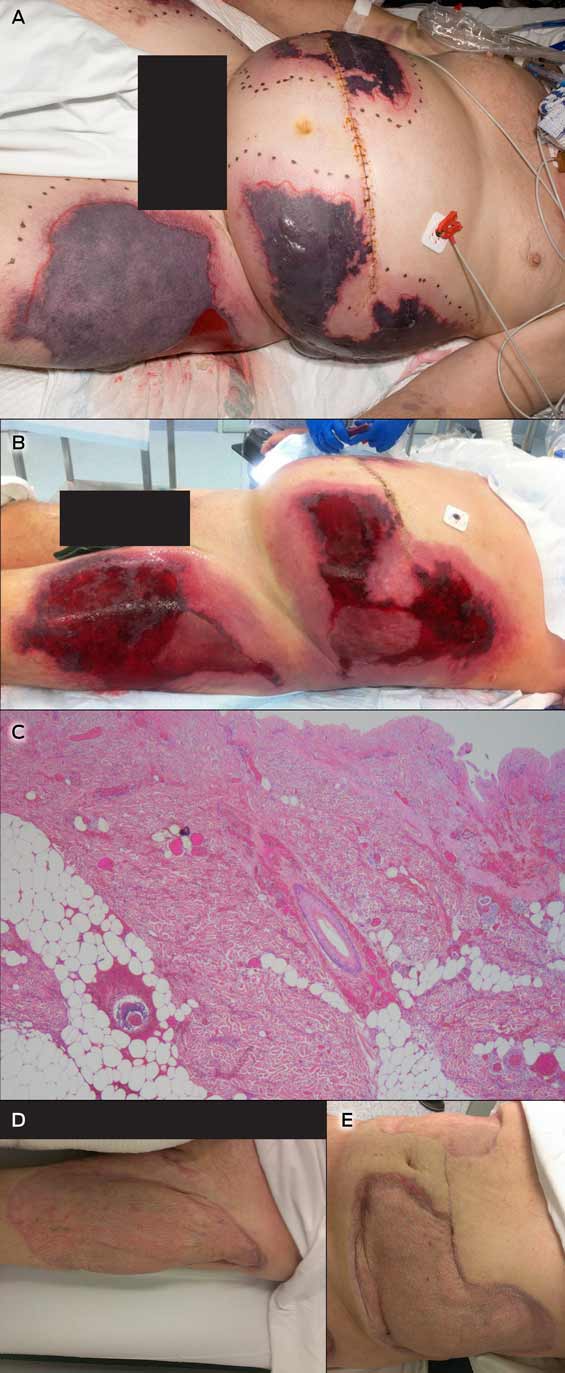
A Bilateral flank and thigh skin necrosis.
B: Wound debridement.
C Diffuse dermal ischaemic necrosis, haemorrhage and oedema. A small number of platelet thrombi are evident in the small veins of the dermis. There is no evidence of vasculitis. Haematoxylin-eosin stain; magnification × 200.
D: Left thigh at 6-month follow-up.
E: Abdomen at 6-month follow-up.
Specialist patients up for thousands as rebate freeze bites
Patients undergoing heart surgery and other specialist treatments face a major hike in out-of-pocket expenses in the next three years that could leave them thousands of dollars poorer if the Federal Government persists with its Medicare rebate freeze, an AMA analysis has found.
Figures prepared by the AMA show the freeze will save the Government almost $2 billion by mid-2018, with more than half of this coming from medical specialists, their patients and health insurers as the value of the Medicare rebate declines and the cost of providing care rises.
The Government has kept the rebate freeze, first announced in last year’s Budget, as a device to encourage the AMA and other medical groups to assist in identifying efficiencies and savings through the Medicare Benefits Schedule review initiated last month.
Health Minister Sussan Ley has described the freeze as a regrettable necessity, though indicating that, “as an article of good faith, I am open to a future review of the current indexation pause as work progresses to identify waste and inefficiencies in the system”.
But the AMA analysis shows it will come at an enormous cost to patients, as the Government dumps a bigger share of health care cost onto households and practitioners.
The AMA estimates the freeze will have caused a $127 million shortfall in Medicare funding this year alone, rising to almost $364 million next financial year, $604.1 million in 2016-17, and almost $850 million in 2017-18. Even without any increase in the number of services provided, the rebate freeze will cumulatively rip $1.94 billion out of the system over four years.
Its effect in general practice has been likened to a “co-payment by stealth”, after University of Sydney research suggested GPs may have to charge non-concession patients more than $8 a visit to make up for the money withheld from the system as a result of the rebate freeze.
AMA President Associate Professor Brian Owler said patients would bear the brunt of the funding shortfall.
“We know that doctors’ costs are going to keep rising. The costs for their practice staff is going to keep rising. The costs to lease their premises and to provide quality practice as a GP or a specialist is going to keep rising,” A/Professor Owler said. “If the rebates don’t rise, those costs have to be passed on in out-of-pocket expenses – we will see less bulk-billing, and there is the possibility of seeing a co-payment by stealth, as has been alluded to by some.”
The AMA President said the effect on patients in need of specialist care would be even more profound, warning that, “the out-of-pocket expenses for specialists are going to be most severely hit”.
Under current arrangements, the Medicare rebate only covers a proportion of the cost of specialist care, and private health funds commit to covering an extra 25 per cent of the MBS fee, plus a loading on top of that for doctors who participate in “gap cover” schemes.
In the past, the health funds have indexed their cover in tandem with increases in the Medicare rebate – and have on occasion increased their cover even when rebates have been held flat.
But A/Professor Owler is among those fearful that insurers will be reluctant increase their cover without any lift in the rebate. If this occurs, many specialists may opt-out of gap cover schemes, which would mean private health cover would revert to the bare minimum 25 per cent of the Medicare rebate, with patients left to pick up the tab.
“I think there is a real issue for private health insurers,” he said. “If they choose to index independently of the MBS, they are going to have to pass on higher private health insurance premiums to people, or, if they choose not to index, there is a real chance that out-of-pocket expenses for specialist costs are going to rise significantly.”
The AMA has prepared resources for doctors and patients to help explain the Medicare rebate indexation freeze and its impact, including a patient guide and clinical examples. The resources are available at: article/medicare-indexation-freeze-support-materials-…
Adrian Rollins

 more_vert
more_vert