Playing woodwind instruments has long been shown to assist those with asthma; now playing the didgeridoo is also found to help
I first met Charlie McMahon in Australia’s bicentennial year when he played at a dinner I was hosting. Charlie is a “whitefella” who, ironically, lived most of his early life around Blacktown in New South Wales. His virtuosity on the didgeridoo gained him international attention both playing with his own band, Gondwanaland, and with Midnight Oil in the 1980s and 1990s. After the dinner, a memorable moment was captured when he was jamming with Galarrwuy Yunupingu — two didgeridoo exponents at the height of their musical powers.
Charlie first became intrigued with Aboriginal culture at the age of 4, when he saw the Charles Chauvel film, Jedda. As a child on his uncle’s farm, Charlie developed his talent for playing the didgeridoo by practising on water pipes of various lengths. This was translated to learning to play the actual instrument in his early 20s, at a time when he was graduating from the University of Sydney with an Honours Arts degree in 1974. Rosalie Kunoth-Monks, who played the title role in Jedda, is a fan of Charlie’s contemporary music.
Charlie’s adolescence ended abruptly when, at 16, he lost his right hand and forearm while making what he describes as a “rocket”. Hence, Charlie has had a prosthetic “hook” arm for the past 48 years. In fact, when he was a guest on the David Letterman show in 1995, the hook attracted as much attention as the instrument.
From 1981 to 1984, Charlie was responsible for establishing essential services in Kintore and Kiwirrkurra near Lake Mackay in the Great Sandy Desert, along the border between the Northern Territory and Western Australia. One of his major tasks was drilling for water and constructing bores.
He was among the group who, in 1984, found the Pintupi Nine — nine Aboriginal people who had continued to live the nomadic lifestyle after the rest of their “mob” had moved out of desert about 20 years before. As Charlie tells it, the Pintupi Nine had been difficult to locate and — even though the husband of the two women (who were co-wives) and father of the seven children had recently died — they were still uncertain about contact with these men who had come to improve the water supply. In fact, they fled when they first encountered Charlie’s drilling crew.
Charlie showed me the film made on his Super 8 after the group had been located, brought into camp and clothed in a motley array of garments to cover their nudity. This was based on their kinsfolk’s advice, to save the Pintupi Nine the awkwardness that their kinsfolk had experienced on first confronting clothed people in the 1960s, “before trouser time” as they put it.
The didgeridoo is an instrument of the Top End of the NT. It is made from eucalypt, predominantly wooly butt, which has been hollowed out by termites, and is allied to the drone trumpet. Charlie adapted the didgeridoo to create the didgeribone which, as the name implies, is a cross between a didgeridoo and a trombone, with a pitch slide function. Unlike the traditional didgeridoo, the didgeribone is made of plastic and therefore not dependent on the native woods, which are becoming increasingly scarce. For example, as the salmon gum is the nesting place of the endangered Gouldian finch, its use is prohibited. In his conversation, Charlie rattles off the number of keys that this “bone” adaptation of the “didge” can achieve. With the help of his Aboriginal friend Tjupurru, Charlie has popularised the didgeribone, having sold 15 000 since 2000.
Charlie has found that playing the instrument improves the lung capacity of people with asthma and other respiratory complaints. This is a purely empirical observation, since playing these instruments requires inhaling only through the nose and essentially using the diaphragm to expel the air. The rhythmic breathing is helped by the cheek muscles where the air circulates before being expelled into the air column where it resonates.
Once the technique of continuous tone through rhythmic breathing has been mastered, there comes, as one continues to play, what Charlie describes as “didge euphoria”. It is described as a feeling of elation not unlike what may be experienced with yoga, and seems to intensify the longer one plays the didgeridoo. The relaxing effect has also been found to help those with panic attacks associated with asthma.
Robert Eley, then at University of Southern Queensland, carried out some research with Aboriginal school students with respiratory problems. Asthma, especially among Aboriginal children, is a problem in schools. He established a program for school children with respiratory problems to learn to play the didgeridoo. For cultural reasons, only the boys were in the cohort receiving didgeridoo tuition; the girls undertook singing and breathing exercises. It was found that the didgeridoo lessons were enthusiastically received and there was evidence that the children’s respiratory function did improve.1
However, many such projects are self-limited — the principal researcher, in this case Eley, moves to a different university with a different job and the impetus is lost.
It is not that the didgeridoo is the only musical instrument that has been recognised as of help to patients with asthma. Playing woodwind instruments has long been shown to assist those with asthma;2 however, it is the sustainability of these projects that is the issue. As I found out myself, one has to first master the art of getting a musical sound out of a woodwind instrument — in my case the clarinet. This can be difficult for those who are not naturally musical. This did not seem to be a problem with the didgeridoo but the sustainability of any program is continued access to, and money for, teachers. While funding was available for the research, there was also the question of ongoing funding for the teachers. When the funding dried up, a promising program became a pile of journal articles (Dr Rob Eley, Academic Research Manager, Faculty of Medicine and Biomedical Services, University of Queensland, personal communication, Aug 2015).
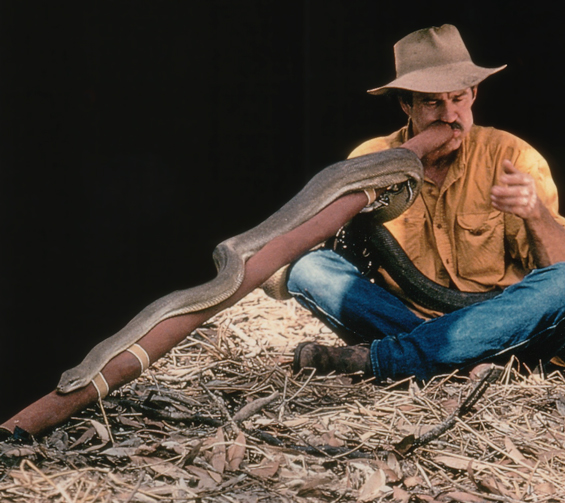
Charlie McMahon likes to teach. He looks and talks like a bushie, with his trademark hat and his moustache concealing a scar from the teenage “rocket attack”. When describing his outback experiences he laces his talk with Aboriginal phrases and sentences. Charlie knows the land but as a whitefella and does not pretend to be Aboriginal. Elders credit Charlie for “inventing complex new ways of playing didjeridu”,3 which has freed him from any accusations of plagiarism.
However, he is the quintessential teacher. I introduced him to a grand round where respiratory disease was the topic. Charlie captivated the audience when he produced his didgeribone and started to play; the audience, which included several foreign graduates, was mesmerised as he went through the keys — the sounds of kookaburra and cockatoo emanating from this exercise in rhythmic breathing.
Charlie needs a home in a respiratory unit, maybe adult, maybe paediatric, maybe adolescent. He has too much talent, knowledge and experiential adaptability for conventional medicine to ignore. There is a challenge to systematically work out whether these instruments, be it didgeridoo, didgeribone or even the Celtic drone trumpet, are therapeutic for people with asthma or other respiratory conditions. The one thing for some respiratory physicians to do is to “bellow” — accept the challenge and travel with Charlie. You never know. These drone instruments may end up being funded as therapeutic devices — but not, as one wag said, “if they have to go through the Medical Services Advisory Committee”.

 more_vert
more_vert