As Theodore Papaioannou and colleagues point out, projecting long-term health spending is challenging.1 Our Article2 and extensions of this research3 made health spending projections for 184 countries and extends through 2040. Many factors—environmental, epidemiological, demographic, cultural, political, economic, and scientific—influenced the creation and evolution of complex health systems, and have coalesced to determine current health spending levels. These same factors will undoubtedly also influence health spending in the future, although how these factors will interact and determine precise spending is difficult to predict.
Preference: Public and Environmental Health
964
[Correspondence] Health economics
Joseph L Dieleman and colleagues (June 18, p 2521)1 should be congratulated for their study on health spending prediction. However, this is a multifactorial and complex problem. The ongoing global financial crisis, rapid development of novel technologies that can increase or reduce total health expenditures, the emergence of often unexpected diseases such as the Zika virus, changing population genetics and epigenetics, and environmental changes and disasters are key parameters that impede the accuracy of spending prediction models.
[Editorial] UK air pollution and public health
The UK Government released its latest consultation documents for controlling air pollution on May 5. Under European law, the UK has a legal obligation to protect public health by minimising the impact of environmental pollutants, including particulate matter and nitrogen dioxide. The UK has been in breach of the European directive since 2010, and has been the target of legal action by environmental groups.
Reducing the incidence of burn injuries to Indigenous Australian children
Burns are a specific health burden, but understanding the detail is vital to finding solutions
It is undisputed that Aboriginal and Torres Strait Islander (Indigenous Australian) children are over-represented in statistics for injury and death caused by trauma. The incidence of each of the major mechanisms of fatal trauma in Australian children — drowning and low speed vehicle run-overs — is higher among Indigenous children.1,2 Burn injuries are also more prevalent among Indigenous children.3
In this issue of the MJA, Möller and his colleagues report a population data linkage study they undertook in New South Wales.4 Their results not only confirm that the incidence of hospitalisation of children for burn injuries is higher among Indigenous than non-Indigenous children. The authors also found that the proportion of burn injuries affecting more than 20% of total body surface area (TBSA) was greater for Indigenous than for non-Indigenous children, as was that of burns to the feet or ankles; that the incidence of being treated in a tertiary burns facility was lower and their median overall hospital stay longer for Indigenous children; and that they were less likely to undergo surgery, but more frequently received treatment from allied health professionals. This important epidemiological study not only supports the hypothesis that burn injuries constitute a significant health burden in Indigenous children, it is also the prelude to a much larger prospective study.5 Paediatric burns services throughout Australia are currently collaborating in a study funded by the National Health and Medical Research Council to examine the journey of the Indigenous child with a burn injury through the health system, including pre-hospital care and outpatient follow-up.5
The report by Möller and co-authors is initially somewhat disturbing, but more detailed analysis identifies factors that explain some of the disparities described. The proportion of Indigenous Australians living in rural and remote geographic locations, and therefore a long distance from tertiary burns facilities, is higher than for other Australians. It is consequently not surprising that many Indigenous children are treated in their local hospital, which has the advantage of keeping the family unit closer to home, with clear psychosocial and financial benefits. With the advent of telehealth services linking major burns services and local hospitals, and the application of digital photography to record wound status at each dressing change, a high standard of care can now be achieved even in remote locations.6,7
Whether a child needs to be admitted to hospital for a burn injury depends on many factors apart from the proportion of TBSA burned. One-third of children are admitted because of the impact of the injury on their family, not because immediate treatment of the burn is needed.8 It is often in the interest of the Indigenous child and family to be admitted to hospital when factors such as remoteness of the family home and socio-economic disadvantage would prevent the families traveling to outpatient appointments for dressing changes. Not only is admission to hospital more likely under these circumstances, the duration of stay will also be longer.
The region of the body affected by a burn is very much related to the mechanism of injury. For example, hot beverage scalds usually affect the face, neck and torso, whereas burns by hot embers and ash from campfires and burn-offs typically affect feet and ankles. Indigenous children have different patterns of burn injury types to other Australian children because of cultural and socio-economic differences. The higher proportion of foot and ankle burns in the report by Möller and colleagues is possibly explained by a higher incidence of campfire burns to Indigenous children.
The estimated TBSA burned is probably the greatest source of inaccuracy when documenting a burn injury.9 Areas of superficial burn (erythema only) are often erroneously included, leading to grossly overestimating the extent of the burn. Burn depth can also progress with time, but the TBSA is often not re-calculated, so that the initial estimate is the only value documented by hospital coders. Overestimation of burn extent would probably occur more frequently in non-tertiary facilities. Lund and Browder charts have traditionally been employed for calculating TBSA, but they are cumbersome to use and should therefore be replaced by mobile phone apps that accurately estimate TBSA by digitally shading on the screen the areas affected. The New South Wales Institute of Trauma has developed an app for this purpose that is free, quick and easy to use; the age and weight of the child are entered, and the degree of fluid resuscitation required (using the Parkland formula) is also calculated.10
People from populations with darker skin colour are reported to re-epithelialise burn injuries up to 25% more quickly than those from populations with lighter skin.11 However, darker skin has a higher propensity for hypertrophic scarring, explaining why the Indigenous children in this study had fewer operations for skin grafting, but significantly greater requirements for management by allied health professionals.
Preventing burns must be part of any intervention to reduce the burden of burn injuries in Indigenous children, alongside optimal first aid. Campaigns to prevent burn injuries will only be successful if they are targeted at specific populations that are at greater risk, and it is important they include collaboration between injury prevention advocates, Indigenous leaders, and health care workers.
Complicated silicosis resulting from occupational exposure to engineered stone products
Clinical record
A 54-year-old man, formerly a smoker, presented with a 6-year history of chronic cough and exertional breathlessness without previous respiratory illnesses. Born in Vietnam, he came to Australia as a refugee at the age of 20 years. A screening chest x-ray was performed on his arrival in Australia; as the patient was not informed about any abnormality, this was assumed to be normal. He commenced work as a labourer; he denied exposure to silica-containing materials and did not participate in activities typically associated with silica exposure (such as jack-hammering) during this period. About 15 years later, the patient started a job manufacturing stone benchtops. He cut, ground, finished and installed the benchtops, using a popular brand of engineered stone comprising > 85% crystalline silica. Occasionally, he made benchtops from granite and marble. During the first 7 years of this work, the patient did not use any respiratory protective equipment, but later used a simple paper mask. Despite some dust extraction facilities in the factory, he reported that the environment was visibly dusty and that dust suppression with water was hardly ever used.
At presentation, chest examination showed scattered fine crackles and bronchial breath sounds bilaterally in the upper zones. Spirometry showed restriction (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC], 1.9/2.6 L [73% and 82% predicted, respectively]) and no bronchodilator reversibility; gas transfer was reduced (diffusing capacity of the lungs for carbon monoxide [Dlco], 60% predicted, carbon monoxide transfer coefficient [Kco], 92%).
Multiple sputum specimens tested negative for acid-fast bacilli. Levels of inflammatory markers were within reference levels, and the result of a screening test for autoimmunity and vasculitis was negative. A computed tomography (CT) scan of the chest (Box 1) showed confluent bilateral calcified fibrotic masses in the upper zones, with marked volume loss, distortion and perilesional bullae. Occasional small peripheral lung nodules were present, predominantly distributed in the upper zones. There was calcified mediastinal lymphadenopathy.
Bronchoscopic washings tested negative for acid-fast bacilli and malignant cells. Positron emission tomography (PET) scanning showed intense uptake in the confluent densities (maximum standardised uptake value, 10.6) and mediastinal lymphadenopathy. CT-guided fine-needle aspiration biopsy was negative for malignant cells. Transbronchial fine-needle aspiration biopsy of lymph nodes using endobronchial ultrasound was non-diagnostic. An open biopsy of the right upper lobe lesions and paratracheal lymph nodes was performed. Histological analysis of the lung sample showed numerous large sclerotic silicotic nodules surrounded by collections of histiocytes (Box 2). Analysis of lymph node sections confirmed prominent nodular silicosis.
Overall, the findings, including PET, were compatible with a diagnosis of complicated silicosis with progressive massive fibrosis. The patient continued to experience worsening breathlessness, despite treatment with bronchodilators and inhaled corticosteroids. He subsequently developed bilateral pneumothoraces, requiring temporary intercostal drain insertion, and is now listed for lung transplantation.
Silicosis refers to a spectrum of progressive and debilitating occupational lung diseases caused by the inhalation of free crystalline silica. Once established, there is no effective treatment. Prevention is therefore paramount. Exposure to silica has been unequivocally associated with an increased risk of lung cancer, as well as an increased frequency of tuberculosis and possibly also autoimmune disease. Implementation of appropriate workplace standards to minimise exposure is crucial to reduce incident and severe cases of silicosis.
Silicon dioxide (silica) is the most abundant mineral on Earth and is present in almost all types of rock, sand, clay and gravel. The most common crystalline forms of silica are quartz, cristobalite and tridymite. Silica exposure may occur in many work settings. Despite a global downward trend, new outbreaks of silicosis have recently been reported, with life-threatening silicosis occurring after exposure to a relatively new type of engineered stone product used for kitchen and bathroom benchtops.1,2 These products (known as “artificial quartz conglomerate” and “artificial stone”), which contain a high content of free crystalline silica (70–90%), are increasingly used in preference to their marble and granite counterparts because of their low cost, improved durability and hardness.
Risk of exposure to high levels of crystalline silica from engineered stone is present at all levels of this industry, from manufacturing (stone cutting, shaping and finishing) to assembly and installation.3 In a recent study, 25 ornamental stone workers who had been employed in dry-cutting a synthetic stone product developed advanced silicosis.1 In another report, silicosis was diagnosed in 46 men working in the manufacture of artificial stone for kitchen benchtops.2
Following these reports, an alert issued in the United States highlighted potentially dangerous levels of silica exposure associated with suboptimal practices in the artificial stone industry.4 Further calls to action have come from Europe, with a report from Tuscany citing seven cases of silicosis in workers exposed to crystalline silica during benchtop manufacturing.5 In almost all reported cases, there was little adherence to basic protection measures, such as provision of appropriate ventilation systems and use of personal protective equipment.
The Safe Work Australia workplace exposure standard for respirable crystalline silica (time-weighted average) is 0.1 mg/m3, which is designed to prevent the occurrence of silicosis.6 Our case reaffirms the need for vigorous enforcement of dust reduction regulations, particularly in the growing industry of engineered stone products. Benchtop stonemasonry is a potentially dangerous occupation, and medical practitioners should have a heightened awareness of this newly described occupational hazard.
Lessons from practice
-
Silicosis is a disabling but entirely preventable occupational lung disease caused by exposure to inhaled free crystalline silica.
-
Recent outbreaks of silicosis have been associated with the manufacture of relatively new engineered stone products that are used for kitchen and bathroom benchtops.
-
Medical practitioners should be aware that cutting and installing these engineered artificial stone products can be a hazardous occupational exposure.
-
Appropriate dust suppression practices and the use of respiratory protective equipment should be reinforced to prevent silica-related diseases.
Box 1 –
Axial (A) and coronal (B) computed tomography scans of the patient’s lungs
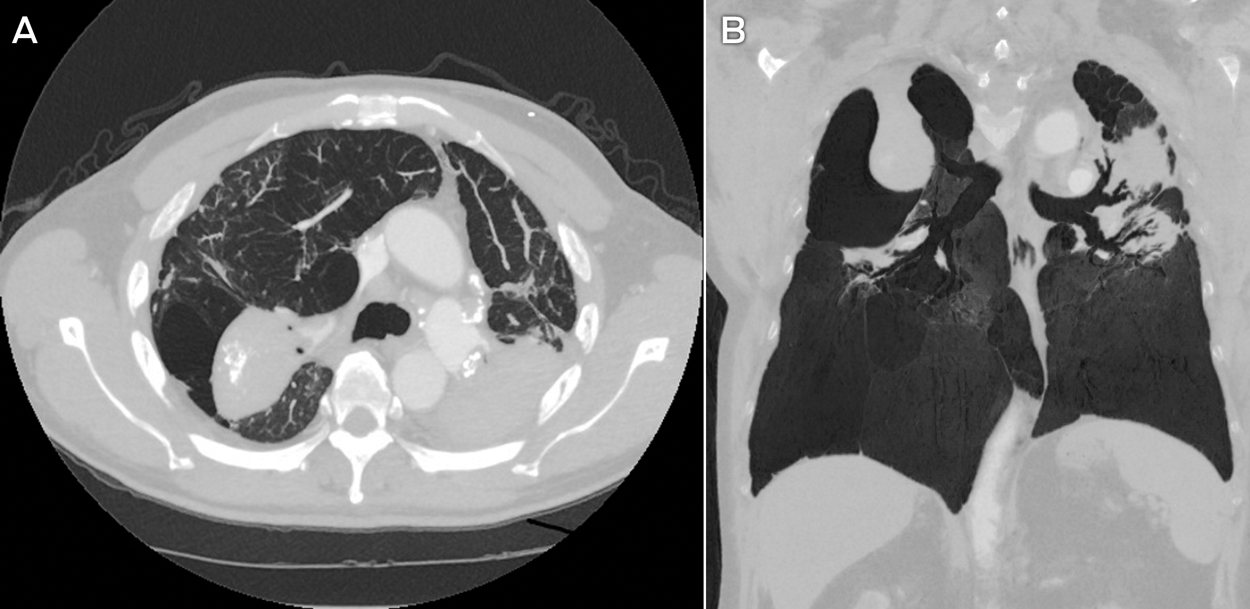
The scans show confluent mass-like fibrosis in the posterior upper lung zones, with adjacent bullae and compensatory expansion of the lower lobes. Calcification is seen within the fibrotic masses as well as within the hilar and mediastinal lymph nodes. There are occasional small peripheral nodules, most obvious in the right lung.
Box 2 –
Typical features of silicosis on lung histopathology slides
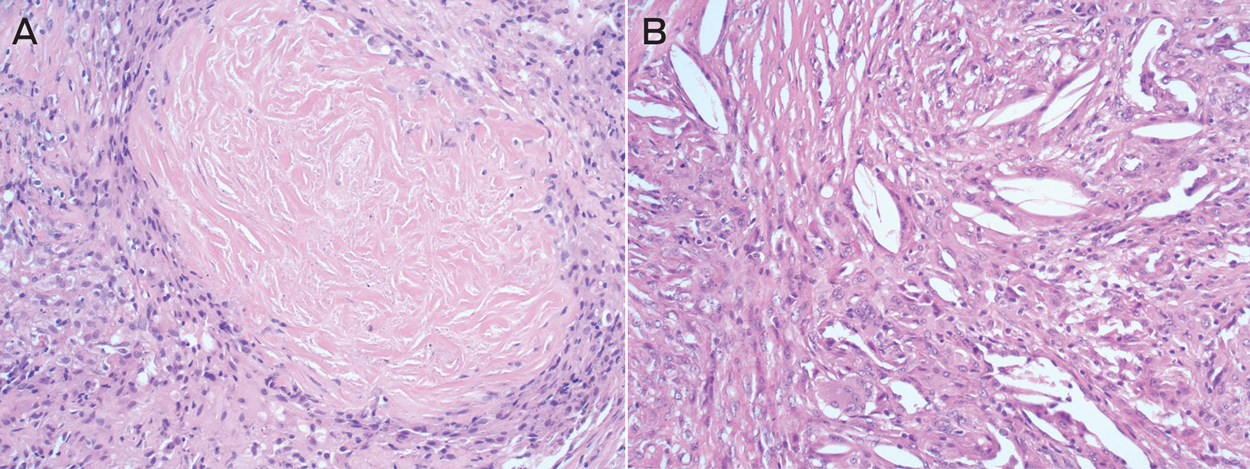
The biopsy specimen (A) shows the whorled appearance of a silicotic lung nodule, consisting of concentric laminated collagen fibres (haematoxylin–eosin stain, magnification 10×). A higher magnification image (B) highlights clefts containing faintly visible silicate particles surrounded by macrophages and giant cells (magnification 20×).
No Jab, No Pay and vaccine refusal in Australia: the jury is out
High immunisation rates in Australia mean that the threat of disease transmission posed by vaccine refusal is low — policy responses should be proportionate
The topic of vaccine refusal has received worldwide attention in recent years. Vaccine attitudes span a continuum from complete acceptance to complete rejection. Vaccine refusal (rejection of all vaccines) is at the extreme end, whereas vaccine-hesitant individuals are a more heterogeneous group, with some opting to fully vaccinate despite substantial concerns while others are more selective.1 People may also change their attitudes and positions over time.
Some countries, including Australia and the United States, have introduced legislative provisions actively targeting vaccine refusal. In Australia, No Jab, No Pay legislation was introduced nationally on 1 January 2016. It removed an exemption, which previously allowed parents whose children were not fully vaccinated, to remain eligible for family assistance payments if a health practitioner certified that they were conscientious objectors to vaccination. The requirement to be fully immunised for age to retain eligibility for family assistance payments commenced in the late 1990s.2 At state level, No Jab, No Play legislation, which requires children attending childcare centres to be immunised, has been tightened in New South Wales and passed in Queensland and Victoria. Victoria has the strictest requirements, with full immunisation necessary for attendance, unless the child has an approved medical exemption or is on a recognised catch-up schedule. NSW continues to allow a written exemption for children of vaccine-refusing parents, and Queensland allows facilities discretion over whether to apply the requirements. In California, recent school entry legislation has removed all non-medical exemptions to mandatory school immunisation requirements, leaving home schooling as the only option for vaccine-refusing parents.
History of vaccination refusal
Ever since the introduction of widespread vaccination to protect against smallpox in the early 1800s, there have been people and groups who have vociferously opposed vaccination.3,4 Legislation to make smallpox vaccination compulsory, introduced in the mid-19th century in Britain4 and in Victoria, South Australia, Western Australia and Tasmania,5 particularly inflamed anti-vaccination sentiment.4,6 As a result of concerted opposition, no such legislation was ever enacted in NSW, despite repeated attempts to introduce it between 1853 and 1913.5,6 In response to sustained pressure, conscientious objection provisions to compulsory vaccination were introduced in Britain in 18984 and in South Australia in 1901, Western Australia in 1911 and Victoria in 1920.5
Recent vaccination refusal in Australia
The first Australian National Immunisation Strategy in 1993 specifically ruled out compulsory vaccination and recommended that conscientious objection be accepted grounds for not vaccinating.7 In 1997, the Immunise Australia Program with its Seven Point Plan was introduced and included, for the first time, the notion of linking eligibility for family assistance payments to vaccine receipt.2 The Australian Childhood Immunisation Register (ACIR) was established in 1996 to collect data on vaccination rates in children under 7 years of age. The ACIR also recorded registered conscientious objection until the introduction of No Jab, No Pay in 2016. Vaccine coverage, as measured by the ACIR, increased markedly over the late 1990s and has remained stable at above 90% since the early 2000s.8 While there was a ninefold increase in recorded conscientious objection between 1999 and 2014, from 0.2% to 1.8%,9 this increase was likely driven in part by increasing awareness over time that registered objection preserved eligibility for applicable family assistance payments.2,10 Our recent study estimated that around 3.3% of children aged 1–6 years in 2013 were affected by registered and unregistered objection combined — not much more than in a previous national survey from 2001, which estimated 2.5–3.0%.10 Although Australia does not have the enclaves of religious-based objection that occur in countries such as the Netherlands,11 there have been consistent geographic clusters of recorded objection — highest (about 10%) in regional areas of northern NSW and southeast Queensland, but present in all states.10 The recent media and government focus on improving vaccination coverage through targeting vaccine refusers can be traced back to the first report of the National Health Performance Authority in 2013,12 which made data on vaccine coverage publicly available for the first time at a small area level. The report received extensive media coverage, which focused particularly on low vaccine coverage in some areas of relatively high socio-economic status in large cities and concluded that this heightened disease risk.13
Level of vaccine coverage needed to control disease
Australia has set a national vaccination target rate of 95% in children,14 based on review of the evidence, consultation with experts and practical considerations. As well as direct individual protection, many vaccines also generate significant indirect herd immunity benefits to the broader population when threshold levels of coverage are reached. The proportion of the population required to be immune to achieve community-level protection (the herd immunity threshold) against a particular disease depends on its basic reproduction number (R0). R0 is a measure of transmissibility and is calculated as the number of people who will be infected on average by a single case. R0 varies by disease, and hence the herd immunity threshold also varies, from 83–85% for rubella and diphtheria to 92–94% for measles (80–85% for smallpox, the only vaccine-preventable disease to be eradicated to date) (Box).15 As rubella and diphtheria vaccines are both highly efficacious (> 95% protective efficacy at the individual level for the recommended schedule), vaccine coverage of 85–90% should be adequate to maintain herd immunity for these diseases. The national 95% coverage target has therefore been chosen specifically with measles control in mind. As 95% of measles vaccine recipients develop immunity after one dose, and 99% after two doses,16 95% coverage should theoretically result in population-level immunity comfortably exceeding the 92–94% herd immunity threshold for measles. However, 95% vaccine coverage in children is not a magic threshold at which all cases and outbreaks of measles, and other diseases, suddenly cease. As well as vaccine coverage in specific geographic areas and subpopulations, outbreak risk is also influenced by immunity in other age groups (eg, immunity is lower in young adults as there was poorer vaccination coverage when they were children but also less circulation of wild-type measles), population density, and level of migration and travel. Measles outbreaks in recent years have not been concentrated in areas with the lowest levels of coverage and highest levels of vaccine refusal, but rather in highly populated urban areas with overall vaccination rates of over 90%.17 This is probably due to both greater population density and likelihood of travel-related importation in such areas.
The ability to achieve herd immunity and prevent outbreaks is also influenced by vaccine characteristics. For example, although highly effective against severe disease in the short term, acellular pertussis vaccines have relatively low (71–78%) efficacy against milder disease, and immunity wanes relatively rapidly.16 As a result, even if 100% of children were fully vaccinated against pertussis, this would not generate strong herd immunity comparable to that achieved by high coverage of measles or rubella vaccine.
Although 95% vaccination coverage in children is a reasonable goal, it is more than is required for some diseases but, at the same time, is no panacaea for highly infectious diseases (measles, pertussis), waning immunity (pertussis) and disease importations (measles). The effort and resources required to achieve incremental improvements in vaccine coverage are proportionately much greater when coverage is already over 90%. Similarly, at such high levels, under-ascertainment of vaccine coverage on the ACIR by only a few percentage points may have a substantial impact on measurement of improved coverage.18
Is No Jab, No Pay a proportionate response to the threat posed by vaccine refusal?
The importance of vaccine refusal as a potential contributor to disease transmission is mainly limited to relatively small geographic areas where levels of vaccine refusal are high. The proportion of the overall population strongly opposed to vaccination is small, with little evidence that it is increasing. This is fortunate, as the scope for attitudinal change among entrenched vaccine refusers is minimal. In contrast, vaccine-hesitant parents can be influenced by appropriate clinician communication, reducing the chance of their hesitancy becoming refusal. Levels of vaccine hesitancy in the population should be closely monitored to allow early detection of significant increases, such as those arising from vaccine safety scares. These scares occur when an adverse event is attributed to vaccination and, regardless of the quality of evidence supporting such a link, becomes broadly disseminated in mainstream and social media. The most widely known example of a vaccine safety scare is that surrounding the subsequently retracted Lancet study that linked measles–mumps–rubella (MMR) vaccine with autism, which, in the United Kingdom (but notably not in Australia), led to falls in MMR vaccine coverage sufficient to cause measles outbreaks.19 Such scares should be identified early so that relevant stakeholders can be engaged and coordinated communication strategies implemented.
Most parents of incompletely vaccinated children in Australia do not disagree with immunisation, but have been unable to overcome a range of logistic and access barriers.20 It follows that measures to improve access to services, assist families challenged by logistic issues, and minimise missed opportunities to vaccinate are the most important means to raise levels of complete immunisation. Measures shown to be effective, both overseas and in Australia, include client reminder and recall systems, incentives, enforcing childcare entry vaccination requirements, audit and feedback of health professionals, opportunistic vaccination in primary, secondary and tertiary care, catch-up plans, standing orders, home visiting, and minimising out-of-pocket expenses to access services and vaccines.21,22
Based on the above considerations, we believe that the stated intent of No Jab, No Pay and of state-based No Jab, No Play legislation — to target vaccine refusal and, in turn, the spread of vaccine-preventable diseases — may prove to be misplaced for two reasons. First, vaccine refusal is the least important of the three factors (refusal, hesitancy and barriers to access) contributing to lower vaccine coverage. Second, there is limited evidence that monetary sanctions are effective in this context of families receiving government assistance,21 among whom the potential for unintended impacts on the health and welfare of children may be greatest. Unintended adverse impacts are arguably even more likely from the highly restrictive Victorian legislation reducing access to appropriate early childhood education. Given the unique nature of these initiatives, and uncertainty about both their effectiveness in reducing disease transmission and potential for adverse impacts, it will be particularly important to carefully evaluate both No Jab, No Pay and No Jab, No Play. Evaluation should focus on identifying differential effects on vaccine uptake, as well as any unintended adverse consequences, among the three key groups (children of vaccine-refusing parents, vaccine-hesitant parents and parents affected by access or logistic issues). As conscientious objection is no longer recorded in the ACIR, national surveys will be required to monitor levels of vaccine refusal.
In summary, unlike in the 1990s when the Immunise Australia Program was introduced, vaccination rates in Australian children are relatively high and at least comparable with similar developed countries. Vaccine refusal is only one of a range of factors relevant to further improvements in vaccine coverage and disease control. The greatest yield is likely to come from first implementing measures already shown to be effective in improving accessibility and minimising logistic barriers to vaccination, and second, from well structured research and evaluation of new interventions to overcome vaccine refusal and hesitancy.
Box –
Herd immunity threshold for selected vaccine-preventable diseases15
|
Infection |
Basic reproduction number* |
Herd immunity threshold |
|||||||||||||
|
|
|||||||||||||||
|
Diphtheria |
6–7 |
83–85% |
|||||||||||||
|
Measles |
12–18 |
92–94% |
|||||||||||||
|
Mumps |
4–7 |
75–86% |
|||||||||||||
|
Pertussis |
5–17 |
92–94% |
|||||||||||||
|
Polio |
2–20 |
50–95% |
|||||||||||||
|
Rubella |
6–7 |
83–85% |
|||||||||||||
|
Smallpox |
5–7 |
80–85% |
|||||||||||||
|
|
|||||||||||||||
|
* Basic reproduction number is a measure of transmissibility and is calculated as the number of people who will be infected on average by a single case. |
|||||||||||||||
Failing to plan is planning to fail: advance care directives and the Aboriginal people of the Top End
Advance care directives can enable Aboriginal people to fulfil their end-of-life wishes to die in their community
The United Kingdom’s great wartime Prime Minister, Sir Winston Churchill, once said “he who fails to plan is planning to fail”. These prescient words resonate for advanced care planning and end-of-life decision making.
Advance care directives (ACDs) are used in all Australian states and territories, but take different forms and names. In the Northern Territory, they are known as advance personal plans (APPs).1 An APP allows not only for advanced consent decisions in relation to life support and palliative care, but also the appointment of a substitute decision maker. The powers of the substitute decision maker under the Advance Personal Planning Act 2013 can include health and financial matters.1
ACDs have a valuable role for Aboriginal and Torres Strait Islander (respectfully referred to hereafter as Aboriginal) Australians for two important reasons. First, Aboriginal people suffer from higher rates of life-limiting conditions and burden of disability approaching end of life.2 Second, because of their strong connections to land and community, Aboriginal people from rural and remote regions have a strong preference to “die at home connected to land and family”.3 McGrath outlined a fear of dying away from home for Aboriginal patients from remote communities and outstations, who were relocated to tertiary facilities often hundreds of kilometres away.3 Early discussion of end-of-life preferences, with the use of an ACD, could play an important part in preventing unnecessary displacement of patients by allowing those who wish to die in their community to do so.
Nevertheless, the sparse research in this area suggests that advanced care planning is not common place for most Aboriginal people.2,4 Some of the reasons for this include the taboo of death talk, communication barriers, presence of multiple clinicians (with no single professional taking on the responsibility for initiation of discussion), uncertainty in prognosis, availability of family (often limited by distance), scarcity of Aboriginal health practitioners, and the formal, structured approach of an ACD. Regardless, Sinclair and colleagues demonstrated acceptance for ACDs in their qualitative study of Aboriginal people in the Great Southern region of Western Australia.2 Their patients outlined the potential for the ACD to ameliorate family disputes. The authors called for an increased role for the family, use of Aboriginal health practitioners, and a whole-of-community approach in implementing ACDs.2
The NT APP is a formal, structured document, which necessitates English language proficiency and health literacy. Previous authors have suggested that these characteristics make ACDs an ineffective document for many Aboriginal patients.2 Despite the nature of the population of the NT and the Royal Darwin Hospital (RDH), its Aboriginal health practitioners are not required to undertake training in the use of the APP as part of their curriculum. It is these same individuals who have been delegated the task of helping Aboriginal patients to complete their ACDs.2 In a Canadian context, Kelly and Minty have called for less formal documentation of aboriginal patients’ wishes.5 A culturally appropriate, less formal document that allows for immediate and future planning may also be most pertinent in an Australian context. However, this carries with it the peril of operating outside the legal protections afforded by the APP. Perhaps, an option for the NT is the creation of an educational document to help inform Aboriginal people about APPs. Similar documents exist in other states, such as Advance care yarning in South Australia.6 The cultural diversity among the Aboriginal peoples of Australia behoves the development of such a document in the NT.
To further examine ACDs for the Aboriginal people of the Top End, especially in the context of life-limiting illness, Territory Palliative Care, Program of Experience in the Palliative Approach (PEPA) and the Aboriginal Medical Services Alliance Northern Territory plan to conduct focus groups with key stakeholders in the NT. Focus group sessions will be run in conjunction with PEPA workshops over the next 12 months. Focus groups will be scheduled in Darwin, Alice Springs, Katherine, Tiwi Island, Gove, Wadeye, Maningrida and Groote Eylandt. Key issues to be examined include the applicability of the current APP for Aboriginal people, education of Aboriginal health practitioners, the utility of a Top End-specific educational document, and the suitability of a less formal document such as a personal portfolio. Funding is being sought for the focus groups and creation of a culturally appropriate education document. In the interim, a steering committee has been created by the RDH to consider the key issues.
[Seminar] Crohn’s disease
Crohn’s disease is a chronic inflammatory disease of the gastrointestinal tract, with increasing incidence worldwide. Crohn’s disease might result from a complex interplay between genetic susceptibility, environmental factors, and altered gut microbiota, leading to dysregulated innate and adaptive immune responses. The typical clinical scenario is a young patient presenting with abdominal pain, chronic diarrhoea, weight loss, and fatigue. Assessment of disease extent and of prognostic factors for complications is paramount to guide therapeutic decisions.
[Seminar] Ulcerative colitis
Ulcerative colitis is a chronic inflammatory disease affecting the colon, and its incidence is rising worldwide. The pathogenesis is multifactorial, involving genetic predisposition, epithelial barrier defects, dysregulated immune responses, and environmental factors. Patients with ulcerative colitis have mucosal inflammation starting in the rectum that can extend continuously to proximal segments of the colon. Ulcerative colitis usually presents with bloody diarrhoea and is diagnosed by colonoscopy and histological findings.
[Editorial] An ounce of prevention
The Robert Wood Johnson Foundation has released its fourth annual National Health Security Preparedness Index report for the USA, and while there is slow improvement, the results still contain warnings for the state of health security in the USA. The index uses over 200 individual measures across six domains. They range from incident and information management to environmental and occupational health, in order to take a snapshot of the state of preparedness for a health crisis; from an outbreak of expanding infectious diseases, such as Zika or a severe influenza outbreak, to climate-change-fuelled floods and droughts that might displace large numbers of people.

 more_vert
more_vert