According to life history theory, increased investment in reproductive function (physiology and behaviour) at different times throughout the life course affects the risk of many diseases and, ultimately, longevity. Although genetic factors contribute to interindividual and interpopulation variation in reproductive traits, the dominant source of variability is phenotypic plasticity during development and adult life. Reproductive traits in both sexes evolved sensitivity to ecological conditions, as reflected in contemporary associations of hormone concentrations with geographical setting, nutritional status, and physical activity level.
Preference: Physiology and Anatomy
894
Blitzed: Drugs in Nazi Germany
Book Review
Blitzed: Drugs in Nazi Germany
Reviewed by Simon Tatz
The rise of Adolf Hitler and Nazi Germany has been analysed, documented and researched for almost a century now, and until recently one assumed there was little if any new evidence to be uncovered.
Blitzed: Drugs in Nazi Germany, by Norman Ohler, became an international sensation when it was published last year. Ohler’s ground-breaking and cleverly written research centres on two aspects of the Third Reich: the use of methamphetamine by the German military, and the role of Adolf Hitler’s personal physician, Dr Theodor Morell.
German pharmaceutical companies such as Merck, IG Farben and Bayer were world leaders prior to WWII, and Germans were huge consumers of what are now illicit drugs, including cocaine and heroin. Three German pharma companies (Merck, Boehringer and Knoll) controlled 80 per cent of the world cocaine market in the 1920. But it was the Temmler factory that Blitzed focus on. Tremmler began producing Pervitin, a methamphetamine pill, in 1937. It soon became a staple of German civilians, then the military. They even manufactured a ‘meth’ brand of chocolates to make ‘housework more fun.’ Each chocolate was equivalent to a modern day ‘hit’ of crystal meth.
Dr Otto Ranke, who became a meth addict himself, oversaw the widespread supply of Pervitin to the Wehrmacht and Luftwaffe. According to Ohler, it was the use of methamphetamine that allowed German tanks to sweep through France as troops stayed awake for two to three days and required little, if any food. The Blitzkrieg was supported by the enormous consumption of these Pervitin meth pills. In the Battle of Britain, Germany’s airpower inferiority was countered by providing their pilots with tablets that kept them awake for days on end. German pilots flew endless mission until they ‘burnt out’ and suffered the effects well known about excessive methamphetamine use.
Pervitin doses to the military ran to over one million per month in 1941, with civilian use put at 1.5 million units per year. Dr Ranke, Director of the Research Institute of Defence Physiology, ordered 35 million Pervitin tablets for the Western Front campaign, while the German Labour Front placed orders for 260 million, then 390 million, Pervitin tablets.
Nazi doctors knew the dangers of meth use and addiction, however they ignored the warnings because it enabled the Nazi war machine, at least initially, to sweep through Europe.
The more fascinating part of Blitzed is the role of Hitler’s personal physician, the mysterious Dr Morell. Despite being interrogated by the Americans after the war, his scrawled personal notes on Hitler haven’t been fully examined. Morell concocted a substance called ‘Vitamulin’, which was derived from rosehip powder, dried lemon, yeast extract, refined sugar and skimmed milk. He marketed this to Hitler and the SS. Hitler, a vegetarian whose diet was mainly salads and vegetables, apparently gained little benefit from the vitamin tablets (and later intravenous injections) but he certainly relied on the Eukodal (Oxycodon) as well as methamphetamine and cocaine his physician prescribed. Hitler was obsessed with his own health and ensuring he had the stamina to lead the war, and Blitzed describes the descent into increasing drug addiction.
In August 1941 Hitler first became seriously ill, and Dr Morell’s vitamin concoctions failed to improve his health. Here is the point where steroids are first used, followed by dolantin, an opioid similar to morphine. Dr Morrell is described as a proponent of polypragmasia – the use of multiple therapeutic modalities to manage a single condition.
Blitzed provides a wealth of fascinating medical research material, much of which lay hidden in archives and not assessed until recently, on the way hard drugs affected decision making by Hitler and the SS. One example is Dunkirk, where Goring’s morphine addiction is attributed to his delay in pursuing the British, thus allowing the famous Dunkirk evacuation.
The evils of Nazi Doctors have been well documented before, however this research has been on their victims and the inhumane experiments carried out in concentration camps and elsewhere. Blitzed – which reads more like a thriller – reveals the role of the personal physician and military doctors in disseminating methamphetamine, steroids, cocaine and morphine to both the architects of the Final Solution and the Third Reich, and the troops who carried out their orders.
[Correspondence] Stroke in ICD-11: the end of a long exile
In 1955, cerebrovascular diseases were reclassified as circulatory system diseases in the 7th edition of the International Classification of Diseases and Related Health Problems (ICD). WHO’s idea then was that stroke is a condition affecting blood vessels. This decision to reclassify cerebrovascular diseases seemed contrary to the pathophysiology and symptoms leading to mortality and morbidity, which are those of brain dysfunction. Moreover, the decision deviated from the principle of ischaemia of other organs (such as the intestines, kidneys, and the eye), which were listed under their respective organs in ICD-7.
[Perspectives] Hypertension
For most of its history medicine has not been a matter of numbers. Just as an early modern physician felt entirely justified in diagnosing without a fine-level grasp of anatomy, so he could confidently prognosticate and prescribe without a great deal of quantifying. Although the classical tradition took a close interest in the movement of blood, seeing it as a kind of nutritious tide originating in the liver, practitioners were more concerned with pulse rate and quality—hard, soft, languid—as markers of general health.
[Editorial] Diabetes: a dynamic disease
The distinction between type 1 and type 2 diabetes was described as early as 500–600 BC by Indian physicians Sushruta and Charaka—type 1 being associated with onset in youth, and type 2 linked to obesity. Today, diabetes is recognised as a complex and heterogeneous disease that can affect people at different life stages. As such, the classic phenotypes of age of onset and metabolic features that once helped to define the types of diabetes are now far less useful clinical indicators. Modern appreciation of the heterogeneity of diabetes is not simply a product of a deeper understanding of the genetics, risk factors, and pathophysiology of the disease.
Art and Medicine
By Dr Jim Chambliss
It is often said that a picture speaks a thousand words.
Contemporary medical technology provides incredibly intricate pictures of external and internal human anatomy.
However, technology does not communicate holistic representations of the social, behavioural and psychosocial impacts associated with illness and the healing process.
Studies have shown that increased reliance on reports from expensive laboratory tests, radiology and specialised diagnostic technology has resulted in inadequacy of physical examination skills; decline in patient empathy, and less effective doctor/patient communication.
Having commenced in May this year and continuing until July 8, continuing professional development workshops which explore and promote the value of art expression in the development of observation skills, human sensitivity and relevant healthcare insights will be presented at the National Gallery of Victoria exhibition of the original works of Vincent van Gogh.
The program will incorporate empirical research to illustrate the way neuropsychological conditions can influence art and creativity. The objectives of the workshops are to:
• advance understanding of the impact of medical, psychological and social issues on the health and wellbeing of all people;
• promote deeper empathy and compassion among a wide variety of professionals;
• enhance visual observation and communication skills; and
• heighten creative thinking.
Over the last 15 years, the observation and discussion of visual art has emerged in medical education, as a significantly effective approach to improving visual observation skills, patient communication and empathy.
Pilot studies of implementing visual art to teach visual diagnostic skills and communication were so greatly effective that now more than 48 of the top medical schools in the USA integrate visual arts into their curriculum and professional development courses are conducted in many of the most prestigious art galleries and hospitals.
The work of Vincent van Gogh profoundly illustrates the revelations of what it means to be uniquely human in light of neurological characteristics, behavioural changes and creative expression through an educated, respectful and empathic perspective.
The exact cause of a possible brain injury, psychological illness and/or epilepsy of van Gogh is unknown.
It is speculated by numerous prominent neurologists that Vincent suffered a brain lesion at birth or in childhood while others opine that it is absinthe consumption that caused seizures.
Two doctors – Felix Rey and Théopile Peyron – diagnosed van Gogh with epilepsy during his lifetime.
Paul-Ferdinand Gachet also treated van Gogh for epilepsy, depression and mania until his death in 1890 at the age of 37.
After the epilepsy diagnosis by Dr Rey, van Gogh stated in a letter to his brother Theo, dated 28 January 1989: “I well knew that one could break one’s arms and legs before, and that then afterwards that could get better but I didn’t know that one could break one’s brain and that afterwards that got better too.”
Vincent did not, by any account, demonstrate artistic genius in his youth. He started painting at the age of 28 in 1881.
In fact, his erratic line quality, compositional skills and sloppiness with paint were judged in his February 1886 examinations at the Royale Academy of Fine Arts, Antwerp to be worthy of demotion to the beginners’ painting class. His original drawings and paintings were copies from others’ art, while his sketches in drawing class showed remarkably different characteristics.
Increased symptoms of epilepsy and exposure to seizure triggers (absinthe and sleep deprivation) ran parallel with van Gogh’s most innovative artistic techniques and inspirations following his move to Paris in 1886 to 1888.
These symptoms increased, accompanied by breathtaking innovation following his move to Arles, France in 1888 and his further decline in mental and physical health.
In Paris he was exposed to the works of many of the most famous impressionistic and post impressionistic painters, but so much of his new techniques and imagery were distinctly innovative in detail without traceable influences from others.
While in Paris his work transitioned from drab, sombre and realistic images to the vibrant colours and bold lines.
His ebb-and-flow of creative activity and episodes of seizures, depression and mania were at their most intense in the last two years of his life when he produced the greatest number of paintings.
His works are among the most emotionally and monetarily valued of all time. Vincent’s painting of Dr Gachet (1890) in a melancholy pose with digitalis flowers – used in the treatment of epilepsy at that time – sold for $US82.5 million in May, 1990, which at the time set a new record price for a painting bought at auction.
Healthcare professionals and art historians have written from many perspectives of other medical and/or psychological conditions that impacted van Gogh’s art and life with theories involving bipolar disorder, migraines, Meniere’s decease, syphilis, schizophrenia, alcoholism, emotional trauma and the layman concept of ‘madness’.
What was missing as a basis to best resolve disputes over which mental or medical condition(s) had significant impact on his life was a comprehensive foundation of how epilepsy or mental illness can influence art and possibly enhance creativity based on insights from a large group of contemporary artists.
Following a brain injury and acquired epilepsy I gained personal insight into what may have affected the brain, mind and creativity of van Gogh and others who experience neurological and/or psychological conditions.
The experience opened my eyes to the medical, cognitive, behavioural and social aspects of two of the most complex and widely misunderstood human conditions.
Despite having no prior experience or recognisable talent, I discovered that my brain injury/epilepsy had sparked a creative mindset that resulted in a passion for producing award-winning visual art.
I enrolled in art classes and began to recognise common topics, styles and characteristics in the art of contemporary and famous artists who are speculated or known to have had epilepsy, such as Vincent van Gogh, Lewis Carroll, Edward Lear and Giorgio de Chirico.
Curiosity for solving the complex puzzle of how epilepsy could influence art led me to pursue a Masters in Visual Art which included a full course exclusively about Vincent van Gogh.
I subsequently obtained the world’s first dual PhD combining Visual Arts, Medicine and Art Curation at the University of Melbourne.
The PhD Creative Sparks: Epilepsy and enhanced creativity in visual arts (2014) was based on the visual, written and verbal insights from more than 100 contemporary artists with epilepsy and provided:
• objective and subjective proof that epilepsy can sometimes enhance creativity – supported by brain imaging illustrating how that can occur;
• a comprehensive inventory of the signature traits of neurological and psychological conditions that have significant interpretive value in healthcare practice and consideration in art history;
• the largest collection of images of the visual narratives from people with epilepsy;
• comparative data to distinguish epilepsy from other medical and mental conditions; and
• the Creative Sparks Art Collection and Website – artandepilepsy.com.
Interest in these research discoveries and art exhibitions provided opportunities for me to deliver presentations at national and international universities, hospitals and conferences. Melbourne University Medical School sponsored an innovative series of workshops through which to teach neurology and empathy by an intriguing new approach.
Jim Chambliss has a dual PhD in Creative Arts and Medicine and has explored the ways epilepsy and other health conditions can influence art and enhance creativity.
Information about his Art and Medicine Workshops involving Vincent van Gogh can be obtained by visiting artforinsight.com or artandepliepsy.com
.
[Seminar] Idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis is a prototype of chronic, progressive, and fibrotic lung disease. Healthy tissue is replaced by altered extracellular matrix and alveolar architecture is destroyed, which leads to decreased lung compliance, disrupted gas exchange, and ultimately respiratory failure and death. In less than a decade, understanding of the pathogenesis and management of this disease has been transformed, and two disease-modifying therapies have been approved, worldwide. In this Seminar, we summarise the presentation, pathophysiology, diagnosis, and treatment options available for patients with idiopathic pulmonary fibrosis.
[Perspectives] The Anatomy of Melancholy revisited
Dr Samuel Johnson struggled to get out of bed in the morning. This was a symptom of what he called his “black dog”—the depression of which he wrote one of the most memorable of all descriptions in a letter to Hester Thrale in 1783: “When I rise my breakfast is solitary, the black dog waits to share it, from breakfast to dinner he continues barking…After dinner what remains but to count the clock, and hope for that sleep which I can scarce expect.” But, according to his devoted biographer James Boswell, there was one book that gave Johnson the will to get up early: “Burton’s Anatomy of Melancholy, he said, was the only book that ever took him out of bed two hours sooner than he wished to rise.” Johnson also gave Boswell, who himself suffered from severe bouts of depression, a valuable piece of advice from Burton: “The great direction which Burton has left to men disordered like you, is this, Be not solitary; be not idle.” He added that the advice should be modified to the effect that those of an idle disposition should not be solitary and those who are solitary should not be idle.
[Comment] From arterial ageing to cardiovascular disease
Although cardiovascular disease is one of the most prevalent and studied diseases in high-income countries, its aetiology has not been fully unveiled. Study of its pathophysiology in other regions will help develop a greater understanding of the disease.
Regenerative neurology: meeting the need of patients with disability after stroke
If regenerative neurology restores function, it will meet a huge unmet need and change dogma
Treatment of stroke in the acute phase has come a long way with the development of paramedic, emergency department and stroke team pathways for hyperacute assessment and management with intravenous thrombolysis, endovascular clot retrieval and hemicraniectomy. Acute stroke units reduce mortality and morbidity by up to 20% or more.1 An estimated 80% of stroke patients survive for one year after stroke, with the large majority being left with chronic disability.2 In Australia and many other countries around the world, stroke is the leading cause of adult disability.3 It is estimated that up to 450 000 Australians have disability after stroke.4,5
The only intervention currently available to stroke survivors is rehabilitation. Increasing evidence suggests that rehabilitation complements the natural functional recovery process that can often continue for months or years after stroke.6 However, there are persisting gaps in our understanding of the basic biological pathways that drive post-stroke recovery, and these pose challenges in applying evidence-based rehabilitation strategies in the real world. This becomes especially critical as patients often need a combination of rehabilitation strategies that cater for their specific disability and complement their potential for long-term recovery. These are often required beyond the period for which rehabilitation services are currently made available due to resource constraints.7 So where does that leave us in 2017?
Regenerative neurology or stem cell therapy may provide an answer to this unmet need by potentially restoring neurological function in an individualised manner. Many stem cell researchers and clinicians hold the view that the field of regenerative medicine may have as large an impact on humanity as antibiotics.8
Basics of stem cells
Stem cells are unique in possessing two qualities — the capacity for self-renewal and the potential for multilineage differentiation. If a stem cell is pluripotent, it can give rise to cells derived from all three germ layers (ectoderm, mesoderm and endoderm) that differentiate into different tissues during embryonic development. On the other hand, a multipotent stem cell tends to generate limited cell types, often relevant to the organ from which the stem cell was derived — for example, haematopoietic stem cells (HSCs) tend to generate blood and immune cell types. Embryonic stem cells isolated from the very early embryo are pluripotent while adult somatic stem cells derived from adult organs, such as mesenchymal stem cells from bone marrow, are multipotent, similar to HSCs.
A significant clinical limitation to the use of embryonic stem cells therapeutically is the potential for them to form tumours, such as teratomas which have multiple cell types from the different embryonic lineages (hair, bone, teeth, heart muscle, etc).9 In contrast, to date, multipotent cells such as mesenchymal stem cells are considered safer, with animal studies reporting no increase in tumorigenicity.10
In 2006, Yamanaka (2012 Physiology or Medicine Nobel Laureate) showed that somatic cells (skin fibroblasts) could be engineered genetically by four genes (known as the Yamanaka factors) to produce pluripotent cells similar to embryonic stem cells.11 This third type of stem cell is termed an induced pluripotent stem cell (iPSC). This discovery has radically transformed stem cell research and proffers the concept of personalised regenerative medicine. Early clinical trials have already started deriving iPSCs from an individual’s fibroblasts for autologous (self-)treatment or personalised medicine.12 The findings of preclinical studies in stroke models have provided encouraging evidence for potential for neuroregeneration and useful insights into potential applicability in the future.13–15
Chronic stroke and local injection
Last year was an exciting one for stem cell therapy in stroke patients. There were two high impact publications documenting early phase clinical studies with two different multipotent stem cells, SB623 and CTX0E03. Both are genetically modified stem cell types, one isolated from fetal brain tissue16 and the other from adult bone marrow.17 Two independent research teams from reputable institutions in the United Kingdom and United States performed these studies with industry funding (ReNeuron and San Bio, respectively).
This research examined two key questions in relation to study design:
-
Is it potentially useful to treat stroke survivors in the chronic phase when their disability has plateaued, sometimes as long as 3 to 4 years after stroke?
-
Is intracerebral implantation of stem cells a feasible route of administration?
Published preclinical and preliminary clinical data indicate that the design of the studies was valid, although research opinion is often divided as to optimum timing and route of administration of cell transplantation.9
Why was stem cell therapy not administered in the acute phase after stroke in these studies? There may be a number of clinically pragmatic answers to this question — in the acute phase, patients may be too medically unstable to undergo neurosurgery. Moreover, patients are often still showing rapid improvement, so it would be problematic to measure any benefit above that of optimum acute stroke unit care, when disability has not yet plateaued.18
Why was a neurosurgical implantation chosen? “Functional neurosurgery” is a fast-developing specialty and these neurosurgeons routinely implant electrodes for deep brain stimulation to treat Parkinson disease. Thus they have the expertise to inject, via a narrow bore cannula, deposits of stem cells into multiple sites within the human brain. One benefit to the patient of intracerebral implantation is that the cells remain within the brain and can be imaged non-invasively.19 An alternative route of administration used in earlier clinical studies was intravenous injection.20 Initially, this approach was considered safer than intracerebral implantation, but it is now appreciated that there is a theoretical risk of distant tumorigenicity, in that stem cells injected intravenously may deposit widely throughout a number of organs within the body (ie, lung, liver, etc.) and may interact with presymptomatic tumours.20
Is it safe?
Early phase clinical trials characteristically involve small numbers of patients to minimise the number at risk if there is a serious treatment-related adverse event. In the two studies described above,16,17 27 patients were followed for 12 months after treatment, which is a generally accepted timeframe. The studies stated that no adverse event directly attributable to the stem cell therapy was found. However, the neurosurgical procedure of creating a burr hole and entering the brain to administer the cells did result in appreciable anticipated adverse events (ie, haematoma, headache and other symptoms related to the consequent reduction of intracranial pressure). It is noteworthy that both studies will continue surveillance of all patients after 12 months to detect any longer term adverse events.
We propose an alternate perspective with respect to the claims that no stem cell-related adverse events occurred. Stem cells implanted into the brain are known from preclinical data to differentiate into neural cells and probably integrate within the brain.9 In theory, this cellular behaviour has the potential to form an epileptogenic focus. A small number of patients in each of the two high impact studies16,17 were reported to have seizures. With this limited clinical dataset it cannot be concluded whether their seizures arose from the neurosurgical procedure, as suggested in the publications,16,17 or was related to the stem cells. We propose that larger phase 2/3 studies should incorporate electroencephalography investigations to better understand the association of seizures with intracerebral implantation stem cell therapy.
The clinical data in these two early phase clinical studies supports the clinical feasibility and safety of intracerebral implantation of stem cells in patients with chronic disability after stroke. Both studies used an escalating dose of stem cell therapy. Cell doses of up to 10 million SB623 and 20 million CTX0E03 stem cells may be used for future larger phase 2 studies.
So: does it work?
This question will not be answered with any degree of certainty for a number of years as we await the results from large, multicentre, multinational, double-blind, randomised controlled clinical trials. While preclinical data from animal studies suggest an overall functional improvement of 40.6%, the extrapolation of these findings to human stroke pathophysiology is limited by: (i) species-specific differences; and (ii) the fact that controlled induction of cerebral ischaemic lesions in animals is not fully representative of the heterogeneous lesion load seen with human stroke.9
Early clinical studies enrolled a heterogeneous mix of patient groups. Most of these studies were open label and single arm and thus not designed to answer the question of efficacy. Therefore, at present, it is difficult to postulate any differential benefit for specific patient or stroke subgroups.18 From a mechanistic perspective, there are a number of theories from preclinical data on how stem cell therapy may decrease post-stroke disability (Box), with neuroplasticity considered to be an important factor.21
An aspect of immense practical relevance is that standardised rehabilitation was not provided to participants in these studies. There is an ongoing debate about the potential confounding effect of rehabilitation on functional and structural outcomes. However, rehabilitation is accepted as a standard of care to optimise natural recovery, and guidelines for stem cell research such as Stem Cell Therapy as an Emerging Paradigm for Stroke (STEPS)22 recommend its inclusion in trial design. Stroke clinicians will know from everyday experience that significant improvement in neurological function many years after an ischaemic stroke is rarely observed. The two studies described above16,17 are very important in the field of regenerative neurology in that both found an associated improvement in function in the chronic phase of stroke among patients with different areas of stroke-induced injury. In light of the emerging evidence for long-term potential to relearn that can be harnessed by rehabilitation, stem cell implantation along with targeted and protracted rehabilitation could have a synergistic and biologically plausible impact on post-stroke recovery.
It is of fundamental interest that both studies described changes on magnetic resonance imaging (MRI) of the human brain after treatment. It was suggested that these MRI findings may not be explained by the neurosurgical procedure alone.17 These preliminary findings may present an opportunity for reverse translational research, from the clinic back into the research laboratory, to gain a better understanding of how changes in the human brain may occur after stem cell therapy.
At this juncture of stem cell research in stroke, there are three important points to be considered:
-
The preclinical and early clinical data which suggest that stem cell therapy may be helpful are becoming encouragingly robust.23
-
The preponderance of failed translation efforts from preclinical to clinical therapeutics in stroke highlights that continued exercise of scientific rigor is critical.
-
Ongoing stem cell tourism across the world and in Australia to reach centres that operate for financial gain without regard to research integrity or patient safety poses a significant danger to the credibility of this field.24
The current regulatory framework in Australia for oversight of cellular therapies has significant gaps in scope as well as implementation. It is a matter of urgency that our politicians and regulatory authorities collaborate with their counterparts in the US, European Union, Japan and other regions where innovative approaches are being implemented to develop the field while creating adequate safeguards to protect patient interests.25,26
Exciting scientific research is that in which the questions raised outweigh the answers. We suggest the quest to fulfil the unmet need for treating disability after stroke has taken a step forward.
Box –
Putative mechanisms of action of stem cells in stroke*
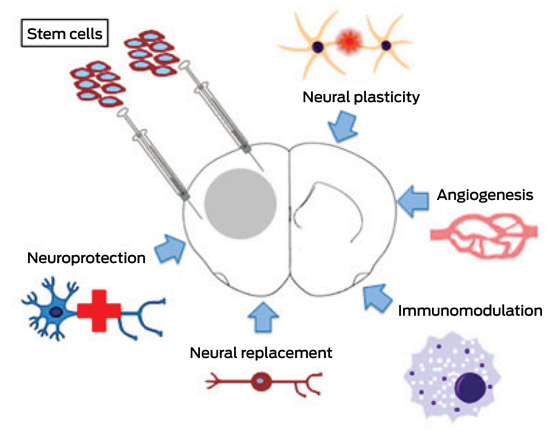
* Adapted with permission from Nagpal et al.21

 more_vert
more_vert