BY PATRICK WALKER
Soft drinks are fast becoming our nation’s vice; our go-to drink choice that’s more bitter than it is sweet. Sugar-sweetened beverages (SSBs) are packed full of calories, yet provide no additional nutritional value or health benefits, and are a major factor driving obesity in Australia and overseas.
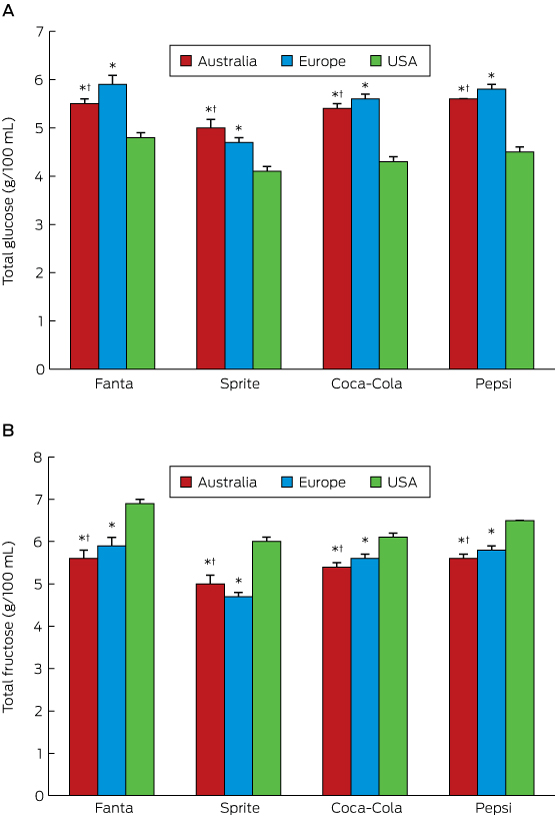
Consider your average 600ml bottle of Coca-Cola – for most people, a single serving. That bottle might cost you $3 from your local supermarket, and contains approximately 64g of sugar.
For the average person, this alone exceeds the WHO recommendation that no more than 10 per cent of your dietary energy should come from free sugars. Not that we’re paying much notice to this recommendation, though – most of us exceed it on a daily basis, and SSBs such as that $3 bottle of coke play a large role in this.
Sugar-sweetened drinks are Australians’ largest source of free sugar intake, perhaps adding flavour and energy to our day, but certainly nothing more. Sugar is only one factor of many that predispose to overweight and obesity, but plays a considerable role that merits attention. A 2006 systematic review, for example, found SSBs to be a ‘key contributor’ to the obesity epidemic, calling for prompt public health strategies to discourage consumption.
In total, 63 per cent of Australians are now overweight or obese, a staggering four-fold increase on 1980 levels. Perhaps more concerning is the fact that one in four children exceed the upper limit of normal for BMI, and many of these kids will continue on to become overweight or obese adults. Most people know that overweight and obesity lead to an increased risk of cardiovascular disease and stroke, diabetes, certain cancers, and a multitude of other diseases. But something that’s often overlooked is their economic toll.
In 2005, data from the Australian Diabetes, Obesity and Lifestyle study put the total direct cost at $21 billion, with the figure ballooning out to $56.6 billion when indirect costs are factored in. Other estimates are more moderate, but the evidence is clear: our waistlines are costing us billions.
Compare that to the $500 million in additional revenue that a well-designed SSB tax could raise annually, as well as bringing about a 15 per cent reduction in SSB consumption and a resulting 2 per cent reduction in the prevalence of obesity.
The link between SSBs and weight gain is well established, as is the link between weight gain and poor outcomes – both health and economic. But where does a tax fit in? And why target SSBs?
Let’s start with the first question. Put simply, price affects consumption. The more things cost, the less likely people are to buy them, particularly products with elastic demand such as SSBs. We saw this with tobacco and alcohol, with increased taxation dramatically reducing consumption. Now is the time to move this strategy to SSBs.
A 2013 meta-analysis on the impact of increased price on SSB consumption found that demand does indeed drop, leading to beneficial health outcomes. Further, the effect is more pronounced for people with low income, due to increased price elasticity. Given these people suffer disproportionately from overweight, obesity, and non-communicable diseases, this means they have the most to gain.
As a discrete and well-defined group of products that provide minimal nutritional value, SSBs are an easy practical target for sound fiscal policy. WHO has publicly recommended an SSB tax, and many countries, including Mexico, France, Denmark, Hungary, Norway, and the USA, have implemented a tax to generally good effect.
Data from Mexico is particularly promising, the tax reducing consumption by an average of 7.6 per cent a year since its introduction in 2010. In low SES households, this figure reached 17 per cent by the end of 2014. Back home, Australian modelling suggests that a 20 per cent tax could significantly reduce SSB consumption, and there is evidence to suggest that while SSB purchasing would drop, overall drink sales would be unaffected.
This is important for two reasons: first, it makes commercial cooperation significantly more likely, removing an important obstacle to implementation; but secondly, and perhaps more importantly, it means people of low SES wouldn’t simply have to fork out more money in their weekly shop, instead being able to switch to alternative, less sugary drinks.
Australia led the way on taxing tobacco and alcohol. We now have a chance to join other nations around the world, and take responsibility for the enormous impact SSBs have on our health. This alone won’t solve the obesity epidemic, but it is an important tool in the array of public health strategies we need. The AMA quite rightly advocates a ‘whole-of-society’, multi-measure approach to tackling the growing issue of obesity, and a tax on sugary drinks is an important part of this.
The health of our nation depends on us taking affirmative action in this space. The clock is ticking. We can’t afford to wait until it’s too late.
Patrick Walker is the 2017 Policy Officer for AMSA Global Health, and was a contributing author to the AMSA policy on Global Food & Nutrition (2016), which, amongst other recommendations, advocated for the implementation of a tax on SSBs.
Twitter: @patrickjbwalker
Email: patrick.walker@amsa.org.au

 more_vert
more_vert