I became Ombudsman to the Lancet journals at the start of 2015, taking over the post from Wisia Wedzicha, who, having been appointed editor of the American Journal of Respiratory and Critical Care Medicine, had stepped down at the end of the previous year. To my knowledge I am the first holder of this post not resident in the UK—I was based in Malawi during most of 2015, but relocated to the UK in December.
Preference: Law
558
Compensated transnational surrogacy in Australia: time for a comprehensive review
Reproductive desire, domestic legal restrictions and cost have made transnational surrogacy a lucrative industry.1 Arrangements usually proceed smoothly, but ethical and legal scrutiny of this practice is ongoing. Commissioning parents have allegedly abandoned well2 and unwell3 children born to surrogates overseas. Investigations into transnational surrogacy are numerous, yet we are no closer to an answer as to whether the current status quo is acceptable.
Surrogacy involves a woman (the surrogate) undertaking a pregnancy and giving birth where another individual or couple (the commissioner[s] or intended parent[s]) will parent the child. Where the pregnancy involves the surrogate’s oocyte, it is termed genetic, partial or traditional surrogacy.4 Gestational or full surrogacy occurs when gametes from the intended social parents or a separate donor are used. Surrogacy arrangements that do not result in net financial gain for the surrogate are referred to as altruistic (or non-commercial4), although the distinction between reimbursement and payment is easily blurred. Altruistic surrogacy is rare in Australia, with only 36 live births in 2013.5 Compensated or commercial arrangements involve payment (beyond mere expenses) in exchange for services. This practice is precluded by law or regulation in all Australian jurisdictions.6
All forms of surrogacy give rise to ethical issues.6 Compensated surrogacy is, however, more ethically contentious than altruistic surrogacy, owing to concerns over exploitation and commodification of women, intended parents and children.4 Concerns about socioeconomic disparities exacerbate these issues. This article focuses on the ethics, law and policy of surrogacy as it applies to Australians commissioning a pregnancy in low-income countries for a fee: a practice that can be termed transnational compensated surrogacy.
Regulation of transnational compensated surrogacy in Australia
Surrogacy is not regulated uniformly in Australia,1 and state and territory regimes have been criticised for the complexities that current oversight gives rise to.7
Altruistic surrogacy is permitted in all Australian states and the Australian Capital Territory, albeit with restrictions in some jurisdictions. Commercial surrogacy is prohibited by statute in all states and the ACT, although payment for reasonable expenses is allowed.8 The Northern Territory has no statutes governing surrogacy, although in order to gain accreditation from the Reproductive Technology Accreditation Committee (RTAC), clinics need to adhere to National Health and Medical Research Council (NHMRC) guidelines that veto commercial surrogacy.6 Draft revisions to the NHMRC guidelines say little about transnational surrogacy other than to stipulate practice standards for Australian clinicians.4
Residents in New South Wales, Queensland and the ACT are liable to be charged with an offence if they engage in compensated surrogacy overseas.9 However, this does not appear to act as a deterrent10 and is difficult to enforce.1 Destination countries include Nepal, Mexico and the Ukraine. Thailand has recently restricted compensated surrogacy to heterosexual couples married for more than 3 years; one of the couple also requires Thai nationality (http://www.sbs.com.au/news/article/2015/07/31/new-thai-surrogacy-law-bans-foreigners). India has recently initiated similar legal reforms.11
Transnational surrogacy also has legal complexity for citizenship and legal parentage. Examples of children ending up stateless have been discussed in the literature.12 Obtaining legal parentage following surrogacy can also be complex and there is potential for legal disputes to arise.1,13
The question of exploitation
The NHMRC’s draft revised ethical guidelines on assisted reproductive technology cite concerns over exploitation to condemn commercial surrogacy.4 The concern here is the wrongful or unfair use of a woman to have a child for another for payment.14,15 Focusing on women’s reproductive labour to benefit a commissioning couple may also fail to show appropriate respect,16 particularly given the vulnerability and unequal bargaining power of those who act as surrogates.17
The financial gain from commercial surrogacy could also unjustifiably induce participation, particularly if there is evidence that financial rewards mean poorer women participate when they would not otherwise.17,18 This could also be framed as a concern over “an unfair ‘disparity of value’”15 between the payment made and risks encountered.
A response might be that surrogacy is a contract just like any other, and we only need to ensure the arrangement is entered into autonomously and fairly, including appropriate consent. However, the practicalities of ensuring valid consent in a social context of deprivation and inequality are not simple.14 Further, a contract in which the subject of the exchange is a reproductive service may be ethically distinct from contracts that do not involve this type of exchange. Surrogacy impacts bodily integrity, is a constant commitment for the period of gestation, restricts behaviour, is risky (with potential lasting physical and emotional effects) and leads to the birth of a new individual.
It is also interesting to consider whether exploitation should be objectively or subjectively determined. Whittaker’s work examining surrogacy in Thailand, for example, suggests that women do not see their role as exploitative; surrogacy is “described as a selfless act of Buddhist merit”.19 However, Whittaker also comments that framing commercial surrogacy as meritorious may merely be a new form of exploitation. Any influence that payment has on these attitudes may also be relevant.
Evidence also suggests that there are practices that exploit women acting as surrogates in some overseas countries. Accounts describe unscrupulous operators motivated by profit,20 contracts being worded to exclude surrogate women from decision making,21 and there are concerns about ongoing medical care and advocacy during pregnancy and after the birth.19 There is some evidence of pressure being applied to women to act as surrogates to help provide for their families.21 Around two-thirds of the fees paid for transnational surrogacy goes to agents.22
It therefore seems that at least some current practices of compensated transnational surrogacy have legitimate exploitation concerns, which will render them ethically problematic if not addressed. On the other hand, surrogacy is but one example of wider problems of exploitation in the face of global inequities.14 We need to ask both whether (and if so, how) we can improve equality and women’s status in transnational surrogacy contracts and how we can also improve surrogates’ material circumstances,17 including ensuring the utmost medical care and appropriate action if harm occurs.
The question of commodification
Commodification can be defined as occurring when surrogates, the services they provide or the children who are born through surrogacy are wrongfully treated as commodities (a product that can be bought and sold).15 The draft NHMRC guidelines cite this as the second main ethical justification for condemning compensated surrogacy.4 Commodification questions arise in all paid surrogacy, but are particularly prevalent in transnational surrogacy due to disparities in relative wealth. Two main questions arise. First, is compensated transnational surrogacy “baby selling”? Second, does it commodify women?
Critics of compensated surrogacy often turn to claims based on “buying children”. Article 2a of an Optional Protocol to the United Nations Convention on the Rights of the Child (ratified by Australia) includes any act of child transfer for remuneration in its definition of the sale of children,23 and some have suggested that legal difficulties in separating payment for a child and payment for reproductive services mean that surrogacy has to be a form of child purchase.15 Additionally, surrogacy contracts often include clauses such that less is paid if a live baby is not surrendered to the commissioning couple.
Wilkinson rejects the claim that surrogacy is “baby selling” on numerous grounds.14,15 One is that a surrogate does not own the baby (insofar as anyone can do this); the commissioning parents do. A handover clause also does not make surrogacy baby selling; it makes it a service contract with a success clause.
As to commodification, conceiving and bearing a child is an intimate process.24 Adding a price could mean that women become mere “wombs for rent” by their commissioners. Wilkinson replies that including a fee-paying aspect does not preclude treating surrogate women with respect. It is the inappropriate use of compensated surrogacy that is commodifying, not compensated surrogacy itself.
It might also be claimed that reproductive labour is just one of many processes for which financial exchange often takes place without demeaning outcomes. Placing children into the care of others, for example, is an intimate and valuable parenting activity for which payment is made. Moreover, not all women may value the intimacy of gestation and labour; or, if they do, they are willing to relinquish this value to another.
Welfare concerns and obligations
Concerns exist around parental obligation and child welfare after transnational surrogacy. For example, if an overseas surrogate is found to be carrying twins, should a commissioning couple take both children? What should happen when a commissioning couple separates during the pregnancy and neither wants the child?
The best interests of the child standard might help answer these kinds of questions. However, the standard itself is liable to criticisms, such as it being vague, or setting a standard that is too high, or being too relative to a particular culture — leaving no room for objective assessment.25 It is difficult to define what is in the best interests of a child conceived via transnational compensated surrogacy. And it could also be claimed that meeting basic interests is enough.
An alternative approach might be to focus on parental obligations. These are applicable to those “who assume the role of a parent” or a person “who has a continuing obligation to direct some important aspect (or aspects) of a child’s development”.26 They include duties such as supporting a child’s development, fulfilling the child’s needs, showing respect, providing primary goods, fostering autonomy and providing advocacy.26,27
Commissioning parents would be subject to these parental obligations, as they have assumed a parental role. The obligation could also be said to be continuing, given that their actions have had a direct causal relationship to the child being born. Commissioning parents who have more children than they can look after or who abandon a child arguably have failed to uphold their parental obligations. The only way parental obligations might end is if a commissioning parent makes appropriate and legal arrangements for another to take on the role instead.
Domestic compensated surrogacy?
Proposed revisions to NHMRC guidelines maintain opposition to compensated surrogacy.4 However, Everingham and colleagues have claimed that the resulting exodus of Australians abroad is a failure of domestic policy.10
How might we respond to this? First, it might be claimed that the status quo could be preserved, perhaps with increased visibility of altruistic surrogacy. However, this would mean that Australians continue to travel for surrogacy, with the risks that this entails,28 the ethical problems it results in and the possibility of prosecution.
An alternate option is to better regulate transnational surrogacy. But we know this is not acting as a deterrent and is poorly enforced.1,18 It may also lead to risks through concealing travel if it were enforced and would require complex agreements between nations.
Third, domestic compensated surrogacy could be sanctioned as a harm-minimisation approach.14,18 Supporters point to factors such as payment being just one factor involved in surrogacy and the inherent commercialisation of assisted reproduction in Australia.18 Regulations could be developed to regulate brokering, fair wages and advertising; the latter is already under consideration in NSW.29
A final option is to take a different ethical approach; for example, by promoting national self-sufficiency.24 This is based on ethical principles such as societal responsibility, solidarity and justice and would involve treating surrogacy in a manner similar to organ donation. However, promoting self-sufficiency does not address the existing low numbers of altruistic donors.
In 2015, the NHMRC invited public comment on fixed payment to Australian oocyte donors beyond reasonable expenses.4 The justification was that many Australians are now travelling abroad and are liable to receive risky or poor-quality treatment. This justification could be said to be a similar harm-minimisation approach to that suggested for surrogacy.14,18 We can therefore question why fixed payment is being considered for oocyte donation in Australia, but not surrogacy.
A nationally coordinated approach to surrogacy may now be on the horizon, with the announcement of a Commonwealth inquiry into surrogacy.30 The inclusion of “compensatory payments” in the terms of reference for the inquiry will hopefully facilitate a thorough and in-depth discussion of these issues nationally. The inquiry is due to report by 30 June 2016.
Conclusion
Transnational compensated surrogacy raises significant ethical and legal issues. It involves balancing surrogates’ and children’s welfare with commissioners’ desires to parent. The present status quo in Australia, with its varying regulations, complexity over legal parentage and concerns over welfare, is problematic. Under both present and proposed regulations, compensated transnational surrogacy will likely continue. Australia needs to do more to ensure that transnational surrogacy is not exploitative or commodifying of surrogates, commissioning parents and children. Parental obligations should also be emphasised in debates over this practice.
Reporting of health practitioners by their treating practitioner under Australia’s national mandatory reporting law
In 2010, the Australian states and territories adopted a national law requiring health practitioners, employers and education providers to report “notifiable conduct” by health practitioners to the appropriate National Health Practitioner Board through the Australian Health Practitioner Regulation Agency (AHPRA). Notifiable conduct encompasses four behaviours: (1) practising while intoxicated by alcohol or drugs; (2) sexual misconduct during the practice of the profession; (3) placing the public “at risk of substantial harm” because of an impairment; or (3) placing the public at risk because of a “significant departure from accepted professional standards”.1 Details of these rules have been published elsewhere.2,3
The mandatory notification law was received with some concern, particularly by doctors and medical professional bodies.2,4 A particularly controversial aspect was its application to practitioners who, in the course of providing care to another practitioner, form a belief that notifiable conduct has occurred. The versions of the law enacted in Western Australia and Queensland allow certain exemptions for practitioners treating other practitioners, but those in force in the other states do not.3
Critics of extending mandatory reporting to care relationships object to the perceived assault on the time-honoured ethics principle of patient confidentiality; they also worry that it will deter impaired practitioners from seeking assistance.5–7 Defenders of the rule argue that treating practitioners have a valuable vantage point from which to identify impaired colleagues, and that requiring them to do so protects the public and enhances trust in the health system.8
Our earlier study of 816 mandatory reports received by AHPRA over a 14-month period2 found that around 8% were made by treating practitioners. In recognition of the importance of these “treating practitioner reports” for policy and practice, we collected and analysed additional data on this subset of reports, and the outcomes of their investigation by AHPRA.
Methods
As part of a larger study of mandatory notification,2 we reviewed all reports received between 1 November 2011 and 31 January 2013. Access to the reports was subject to strict conditions guaranteeing privacy and confidentiality, and study team members signed non-disclosure agreements. The study was approved by the Human Research Ethics Committee at the University of Melbourne (reference, HREC 1239183.2).
The examined reports were from all states and territories except New South Wales, and had been lodged with AHPRA either in a notification form available on the AHPRA website or in letter form. The layout and content of the reports have been previously described.2 Although health practitioners in NSW are subject to the same reporting requirements as those in other states, AHPRA has a more limited role in relation to notifications made in NSW.2
The reports were reviewed between April and June 2013 at the AHPRA head offices in Melbourne. Three trained reviewers extracted de-identified information about the statutory grounds for notification, the type of problem reported, and practitioner characteristics and demographics. This information was supplemented with data from the national register of health practitioners, including information on sex, age, practice location, profession, and the specialties of both the reporter and the subject of the report.
All reports lodged by a treating practitioner about a practitioner-patient were flagged for more detailed review; they formed the focus of our analysis.
A senior investigator (MB) examined each flagged report to verify that it had been submitted by a treating practitioner. She also extracted any free text that discussed the health condition treated, the nature of the treatment relationship, the perceived risk, and steps the reporter took before lodging their report.
Using a grounded theory approach,9 two investigators (MB, DS) reviewed a subsample of the extracts and developed a coding scheme for deriving information on six variables from the free text: primary health condition for which the patient was being treated; the reporter–patient relationship; the timing of the risk; impediments to risk reduction; advice sought on reporting obligations; and disclosure to the patient of the intent to report. Using the finalised coding scheme, one investigator and a second, legally trained reviewer independently coded the textual extracts for all reports.
Comparison of the data coding by the two coders found inter-rater reliability that ranged from good to very good, depending on the variable. For example, the kappa (κ) score for the variable “impediments to risk reduction”, which probably involved more implicit judgment than the other variables, was 0.77.
In November 2014, the outcomes of the response by AHPRA to each case were obtained and added to the analytic dataset. This allowed 18 to 36 months to elapse after the report lodgement dates.
Statistical analyses were conducted with Stata 13.1 (StataCorp).
Results
Of 846 mandatory reports made to National Boards through AHPRA during the study period, 64 (8%) were lodged by health practitioners who had a treating relationship with the subject of the report. The others were lodged by non-treating practitioners, managers, employers or educators. All results reported here relate to the treating practitioner reports.
Sample characteristics
A large majority of the reporters (57 of 64) were doctors, and most of the practitioner-patients were nurses (41 of 64) (Box 1). Two-thirds of the reports by doctors were made by psychiatrists (26 of 57) or general practitioners (16 of 57).
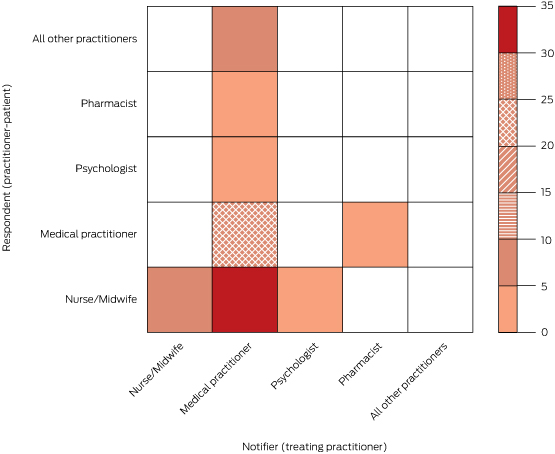
The most common dyads were doctors reporting nurse-patients (35 of 64 cases) and doctors reporting doctor-patients (15 of 64 cases) (Box 2). Nurse reports about nurse-patients were relatively uncommon (5 of 64 cases), although every nurse report involved a nurse-patient.
Grounds for report
Three-quarters of the reports (47 of 64) indicated that the practitioner-patient had placed the public at risk of substantial harm because of an impairment (Box 3). One-fifth of the reports (14 of 64) indicated that the practitioner had practised while intoxicated. Only three reports were triggered by departures from professional standards or sexual misconduct.
Health condition being treated
Practitioner-patients were primarily being treated for mental illnesses (28 of 64), substance misuse disorders (25 of 64) or neurological conditions (9 of 64) (Box 3). The most common forms of mental illness were psychosis, mania and depression. The most commonly misused substances were opiates, benzodiazepines, alcohol and amphetamines.
Nature of treatment relationship
The reporter for one in five reports (14 of 64) was the patient’s regular care provider (Box 4); the others involved treatment encounters with a non-regular care provider. The most common scenario was that the reporter had assumed the role of treating practitioner in the context of an acute presentation to hospital (38 of 64 cases), usually a psychiatric admission (27 of 38 cases). The other scenarios were that the reporter was seeing the patient for the first time (9 of 64 cases) or that the treatment relationship had been established indirectly through an informal corridor consultation (3 of 64 cases).
Other aspects of reports
In most reports (46 of 64 cases), the reporter mentioned discussing the mandatory notification requirement with the patient before the report was lodged. Most reporters (56 of 64) also mentioned that they had sought advice from an indemnity insurer, lawyer, manager or professional peer before making the report.
Twenty-six of the 47 reports of impairment described a risk of harm to the public; 12 of these reports discussed only future risks, six discussed only past risks, and eight discussed both.
Nearly four in five reports (50 of 64) described an impediment to risk reduction. There were four main types of impediment. The most commonly described was that the practitioner-patient lacked insight into the risks posed to patients by conditions such as mania, psychosis, or dementia (29 of 50 cases). A second impediment was deliberate dishonesty with the treating practitioner; this most commonly arose in cases where a practitioner-patient had an addiction and intentionally provided false information to the treating practitioner in an attempt to obtain drugs of misuse (12 of 50 cases). A third impediment was deliberate disregard for treatment advice or patient safety (5 of 50 cases); for example, when a practitioner would not adhere to prescribed medicines or comply with a plan intended to protect patients during the recovery of the treated practitioner. The final impediment to safe management was an ongoing intention to self-harm with medicines that could be obtained in clinical practice (4 of 50 cases).
The 14 reports that did not describe impediments to risk reduction either contained statements indicating that the practitioner-patient had insight into their health condition and was cooperating with treatment (two of these patients had already notified themselves to AHPRA), or there was no relevant information that enabled coding of this variable.
Reponses of reports
By November 2014, National Boards had made a final decision on 86% of the treating practitioner reports (55 of 64). Boards took immediate action in 19 cases. Immediate action is a formal measure that involves placing interim restrictions on practice; it is imposed when this is considered necessary to protect the public pending further investigation.
The final outcomes were: no further regulatory action by a Board (24 of 55 cases); voluntary agreements with the Board and AHPRA regarding appropriate monitoring, treatment or practice restrictions (16 of 54); imposition of formal conditions on the practitioner’s licence (12 of 55); a fine or formal reprimand (2 of 55); and referral to another body for resolution (1 of 55). Although the most common adjudication was to take no further action, it would be erroneous to infer that reports with this outcome were inappropriate or unfounded; steps may have been taken to redress a legitimate concern after the report had been lodged and before the Board’s final decision.
Discussion
Our study of mandatory reports of notifiable conduct by treating practitioners found that 90% were made by doctors, usually psychiatrists or general practitioners, and were typically related to a practitioner-patient who was experiencing mental illness, substance misuse problems or a neurological condition. Relatively few reports were made by regular care providers. Most reports were linked with situations in which the treating practitioner was struggling to safely manage the risk that the practitioner-patient posed, and reporters usually discussed the report with the patient before submitting it.
Australia’s requirement that treating practitioners notify regulators of practitioner-patients with impairments is not unprecedented. New Zealand has required health practitioners to report impaired peers since 2003,10 and several American states have mandatory reporting obligations that extend to treating practitioners.11 However, the Australian legislation is unusually far-reaching in two respects. First, it imposes a duty to report not only health impairments, but also certain concerns about performance. Second, it does not explicitly shield treating practitioners from the obligation to report if the practitioner-patient is participating in an approved program of treatment.
Opponents of mandatory reporting argued that the new requirements would open the floodgates to over-reporting.2 This has not occurred. Mandatory reports are rare events,2 and mandatory reports by treating practitioners are especially infrequent — so infrequent, in fact, that under-reporting is probably a more justifiable concern.
The prevalence of impairment in the health workforce is unknown, but conservative estimates suggest that at least 1000 doctors (about 1% of Australia’s 90 000 registered medical practitioners) are impaired in their ability to practise at some stage in the course of any given year.12–14 Our 15-month sample contained reports on only 16 doctors, and only 20% of the reports were made by the practitioner-patient’s usual care provider. Previous research in the United States and New Zealand suggests that under-reporting of impaired colleagues is widespread,15 even in the context of mandatory reporting laws. Barriers are likely to include loyalty to colleagues, concerns about over-reacting to a situation, and uncertainty about the reporting obligation.16–18
A second objection to the extension of mandatory reporting into the patient–doctor relationship is that it breaches a cornerstone of medical ethics: patient confidentiality. However, the duty to maintain patient confidentiality is not absolute. It is widely accepted that it should yield to obligations to report serious problems or risks that come to light during treatment, including certain infectious diseases, health conditions that imperil driving, and signs of child abuse.19 Whether impairments that pose risks to safe clinical practice are so different from these accepted forms of reporting is debatable. Addressing this issue is beyond the scope of our study, but several aspects of our findings should inform the debate. In particular, the infrequency of treating practitioner reports and the perceived seriousness of the impairments disclosed make it difficult to distinguish the risks associated with practitioner-patient impairment from those of other accepted categories of mandatory reporting by treating practitioners.
Perhaps the most serious charge levelled at the mandatory reporting of practitioner-patients is that it will discourage medical practitioners from seeking assistance.5 This objection involves an empirical question: do the harms that result from treatment foregone because of the law exceed the harms averted by identifying impaired practitioners who would not otherwise have been recognised? Such counterfactuals are difficult to assess. Anecdotal reports suggest that the Doctors’ Health Advisory Services in some states experienced a decline in referrals after the law was enacted.6 But it is not clear whether there was a net decrease across all relevant health services; the question of causality is even less certain. Further, the deferred treatment argument presumes that impaired practitioners would still seek care in the absence of the possibility that they might be reported, but the available evidence suggests that health practitioners may have been reluctant to do so even before the introduction of the law.17,20
When discussing concerns about seeking help, it is worth noting how the reporting behaviour by treating practitioners observed in our study deviated from the exact requirements of the law. The statutory duty to report refers to a past risk of harm and, unlike mandatory reporting programs elsewhere, there is no safe harbour for cases where a practitioner-patient subsequently seeks care and takes appropriate steps to protect patient safety. The pattern of reporting we observed did not correspond with these legal requirements. When explaining their decision to report, treating practitioners were more likely to refer to a future risk of harm than to a past risk. Further, treating practitioners frequently emphasised factors that reduced their ability to work with the practitioner-patient to mutually manage the risk to the public (eg, the patient’s lack of insight, dishonesty or recklessness). Caution is required when making inferences about notifiable conduct that was not reported on the basis of what was reported, but these aspects of the reports, coupled with the very low overall rate of reporting, clearly suggest that treating practitioners resisted reporting their practitioner-patients in circumstances where their treatment was on an appropriate and promising path.
Our study has three main limitations. First, we were unable to directly measure over- and under-reporting. Second, Australia’s mandatory reporting law was implemented in concert with a variety of other major changes to health practitioner regulation, so it was not feasible to assess changes in the rate or nature of treating practitioner reports before and after the introduction of the new law. Finally, we relied on information provided in the reports for most of the variables of interest. To save time or protect confidentiality, some treating practitioners may have omitted or altered salient details. Consequently, the counts we report, particularly for variables that relied on being mentioned in the reports, should be interpreted as lower bound estimates.
Much of the policy debate on the merits of mandatory reporting by treating practitioners has been based on certain implicit assumptions. The standard narrative involves an impaired patient who recognises their illness and seeks treatment from their usual care provider, who must then reluctantly take the contentious step of reporting their patient. Our findings suggest a different picture. The debate should acknowledge several realities. In particular: treating practitioner reports are rare, very few are made in the context of an established treatment relationship, and they tend to occur in situations where there is an identified impediment to safely managing a future risk of harm within the confines of the treating relationship.
Box 1 –
Characteristics of treating practitioners and practitioner-patients involved in mandatory reports
|
|
Practitioner making the notification (treating practitioner) |
Practitioner subject to the notification (practitioner-patient) |
|||||||||||||
|
|
|||||||||||||||
|
Total number |
64 |
64 |
|||||||||||||
|
Profession |
|
|
|||||||||||||
|
Medical practitioner |
57 |
16 |
|||||||||||||
|
Nurse |
5 |
41 |
|||||||||||||
|
Pharmacist |
1 |
2 |
|||||||||||||
|
Psychologist |
1 |
1 |
|||||||||||||
|
Other* |
0 |
4 |
|||||||||||||
|
Status |
|
|
|||||||||||||
|
Practitioner |
64 |
59 |
|||||||||||||
|
Student |
0 |
5 |
|||||||||||||
|
Sex |
|
|
|||||||||||||
|
Male |
40 |
20 |
|||||||||||||
|
Female |
23 |
44 |
|||||||||||||
|
Data missing |
1 |
0 |
|||||||||||||
|
Mean age (range), years |
46 (24–62) |
41 (20–81) |
|||||||||||||
|
|
|||||||||||||||
|
* Dentist, physiotherapist, medical radiation practitioner. |
|||||||||||||||
Box 2 –
Frequency of notifications, by professions of treating practitioner and practitioner-patient
Box 3 –
Statutory grounds for reporting, and health conditions mentioned, for 64 mandatory reports by treating practitioners
|
Statutory grounds for report |
Number of reports |
||||||||||||||
|
|
|||||||||||||||
|
Have an impairment |
47 |
||||||||||||||
|
Practised while intoxicated |
14 |
||||||||||||||
|
Departure from professional standards |
2 |
||||||||||||||
|
Sexual misconduct |
1 |
||||||||||||||
|
Health condition being treated |
|
||||||||||||||
|
|
|||||||||||||||
|
Mental illness |
28 |
||||||||||||||
|
Psychosis/mania |
16 |
||||||||||||||
|
Depression/attempted suicide |
10 |
||||||||||||||
|
Eating disorder |
1 |
||||||||||||||
|
Obsessive–compulsive disorder |
1 |
||||||||||||||
|
Substance misuse |
25 |
||||||||||||||
|
Opiates |
8 |
||||||||||||||
|
Benzodiazepines |
6 |
||||||||||||||
|
Alcohol |
5 |
||||||||||||||
|
Amphetamines |
5 |
||||||||||||||
|
Other (cannabis, cocaine or LSD) |
3 |
||||||||||||||
|
Neurological condition |
9 |
||||||||||||||
|
Dementia/cognitive impairment |
7 |
||||||||||||||
|
Seizures |
2 |
||||||||||||||
|
Unclear |
2 |
||||||||||||||
|
|
|||||||||||||||
Box 4 –
Relationship between treating practitioner and the practitioner-patient for 64 mandatory reports by treating practitioners
|
Treating relationship of reporting practitioner to practitioner-patient |
Number of reports |
||||||||||||||
|
|
|||||||||||||||
|
Regular care provider |
14 |
||||||||||||||
|
General practice |
9 |
||||||||||||||
|
Psychiatry practice |
4 |
||||||||||||||
|
Infectious disease practice |
1 |
||||||||||||||
|
Non-regular care provider |
50 |
||||||||||||||
|
Acute care provider |
38 |
||||||||||||||
|
Psychiatric admission |
27 |
||||||||||||||
|
General medical admission |
2 |
||||||||||||||
|
Emergency department admission |
9 |
||||||||||||||
|
First assessment |
8 |
||||||||||||||
|
Psychiatrist |
4 |
||||||||||||||
|
Physician |
3 |
||||||||||||||
|
Pharmacist |
1 |
||||||||||||||
|
Psychologist |
1 |
||||||||||||||
|
Informal consultation with colleague |
3 |
||||||||||||||
|
|
|||||||||||||||
[Correspondence] Systematic reviews and research waste
In their letter,1 Ian Roberts and Katharine Ker made three assumptions: that small clinical trials are all of poor quality; that all large, multicentre, well funded trials are of exemplary quality; and that meta-analysis cannot ameliorate the low power of small trials. None of these assumptions are documented. Although many clinical trials do have methodological flaws, many do not, and this issue is addressed in systematic reviews with sensitivity analysis. Certainly, the aims of meta-analysis are to achieve increased statistical power and better quality assessment and to obtain a summary statistic.
Anti-vax dodge a dubious legal ploy
Doctors are being urged not to sign a form being circulated by anti-vaccination campaigners attempting to circumvent new ‘No Jab, No Pay’ laws.
The AMA’s senior legal advisor John Alati said the form, which asks doctors to acknowledge the ‘involuntary consent’ of a parent to the vaccination of their children, used unusual, confusing and misleading wording, and was of dubious legal status.
“This is not a Government-issued form, and there is no legal obligation whatsoever on a doctor to sign it, or even consider it,” Mr Alati said. “It is likely to be meaningless in the legal sense.”
The form has been circulated among anti-vaccination groups ahead of the 2016 school year following Federal Government welfare changes aimed at denying certain welfare payments to parents who refuse to vaccinate their child.
Under the No Jab, No Pay laws, from 1 January this year parents of children whose vaccination is not up-to-date will not be eligible for the Family Tax Benefit Part A end-of-year supplement, or for Child Care Benefit and Child Care Rebate payments. The only exemption will be for children who cannot be vaccinated for medical reasons.
The new laws are aimed at penalising parents who claim a conscientious objection to vaccination, and to provide an incentive for parents who have neglected their child’s vaccination to bring it up-to-date.
The new laws were introduced amid mounting concern that vaccination rates in some areas were slipping to dangerously low levels, increasing the risk of a sustained outbreak of potentially deadly diseases such as measles.
The Australian Childhood Immunisation Register shows there has been a sharp increase in the proportion of parents registering a conscientious objection to the vaccination of their child, from just 0.23 per cent in late 1999 to 1.77 per cent by the end of 2014.
In all, around a fifth of all young children who are not fully immunised are that way because of the conscientious objection of their parents.
The form being circulated by anti-vaccination groups, headed “Acknowledgement of involuntary consent to vaccination”, is intended to circumvent the No Jab, No Pay laws and allow conscientious objectors to receive Government benefits without allowing the vaccination of their children.
But Mr Alati said the dubious nature of the document made it highly unlikely it would be effective in achieving its goal.
He said the very claim of ‘involuntary consent’ in the form’s title was muddled.
“[Consent] may be grudging or doubtful, but if it is given by a person with capacity, apprised of relevant facts, it is consent,” Mr Alati said. “If it is not voluntary, it is presumably not consent.”
In the form, the doctor is asked to sign a statement that “consent provided by (name of parent) is not given ‘voluntarily in the absence of undue pressure, coercion or manipulation’, and hence that, according to Section 2.1.3 Valid Consent of the Australian Immunisation Handbook 10th edition, the consent is not legally valid. Given the absence of valid consent, I am/am not willing to proceed with the vaccination of (name of child).”
Mr Alati said the wording of the acknowledgment was “confusing, to say the least”.
But he warned that although the form was likely to be legally meaningless, its wording was concerning.
He said the fact that it did not include a statement that the doctor had outlined the risks and benefits of vaccination may be used as evidence that the patient was not properly informed of the implications of not being immunised.
And he said the wording of the line “I am/am not willing to proceed with the vaccination of…”, created the false impression that the choice of whether or not to proceed with the vaccination lay with the doctor, not the parent.
Mr Alati said where there was no medical reason for exemption, the doctor’s job was to outline the relevant facts about immunisation and to provide vaccination where consent was given. Where it was withheld, “the doctor should not perform the procedure as it might constitute trespass to the person”.
The AMA legal expert advised doctors presented with the form not to sign it.
“Given the unusual, confusing and misleading wording of the form and its dubious legal status, we do not recommend that any doctor sign it,” he said. “Doctors should explain to the parent or carer that it is their choice whether to proceed with the vaccination, based on what they have been told, and note the situation on the patient’s health record.”
He said any doctor considering signing the form should “carefully weigh up the potential risks of doing so”.
Adrian Rollins
Ley tries to stymie opposition with hep C link
Health Minister Sussan Ley has attempted to stifle opposition to controversial pathology and diagnostic imaging bulk billing incentive cuts by linking the changes to plans to eradicate hepatitis C within a generation.
The Health Minister said a $1 billion initiative to publicly subsidise access to breakthrough hepatitis C drugs had been “fully accounted for” in the mid-year Budget update unveiled on 15 December, but had not been announced at the time to enable confidential price negotiations with the drug companies to be finalised.
Ms Ley confirmed to the Adelaide Advertiser that axing and winding back bulk billing incentive payments for pathology and diagnostic imaging tests – collectively expected to save $650 million over four years – would help fund the subsidy for hepatitis C drugs.
“This demonstrates that the Government is prepared to make the tough decisions to prioritise where we should put our health dollar in Australia,” the Minister said.
By linking the two measures, Ms Ley will make it harder for political opponents of the bulk billing incentive cuts to block the measures in the Senate, where many previous health measures have foundered – most recently proposed changes to the Medicare safety net.
But, while he was “really pleased” hepatitis C patients would get access to potentially life-saving drugs, AMA President Professor Brian Owler warned the Minister she would be “on dangerous ground” if she sought to trade the interests of one group of patients against those of another.
Shadow Health Minister Catherine King told the Adelaide Advertiser that, while she welcomed the decision to list hepatitis C treatments on the PBS, it was “an absurd proposition” to make patients with cancer, diabetes and other serious health conditions pay for the treatment of other seriously ill people.
Professor Owler has criticised the bulk billing cuts, warning that they amounted to a “co-payment by stealth” because they would force pathology companies to begin charging patients a fee.
One of the nation’s largest providers, Sonic Healthcare, has already warned that patients could be charged $20 for a blood test.
Professor Owler said such a co-payment would hit chronically ill patients in need of frequent pathology tests particularly hard, and would discourage many from having diagnostic tests, increasing the risk of more serious health problems later in life.
But Ms Ley has vowed to confront providers over any plans to introduce a co-payment, claiming such a move was “not appropriate”.
She has argued that competitive pressures in the pathology industry meant that companies should absorb the cut, rather than passing it on to patients.
But the pathology market is dominated by two major providers, and the fact that they are contemplating introducing a co-payment suggests the Government’s analysis of the dynamics of the market is flawed.
But the Minister appears confident that she has the upper hand in the politics of the debate, particularly given her move to link the bulk billing incentive cuts to the hepatitis C announcement.
“I have every expectation that Labor will pass these savings, as they make perfect sense – and, particularly, in the context of an announcement like [the hepatitis C initiative],” she told the Australian Financial Review.
Under the measure, the Government will list four new frontline drugs for the treatment and cure of hepatitis C, including sofosbuvir with ledipasvir (Harvoni), sofosbuvir (Sovaldi), daclatasvir (Daklinza), and ribavirin (Ibavyr), on the Pharmaceutical Benefits Scheme from March next year.
The move is expected to benefit around 233,000 people currently infected with the blood-borne virus that attacks the liver causing serious illness, including cirrhosis and cancer. Around 10,000 people are diagnosed with the disease each year, and it responsible for about 700 deaths annually.
The Government’s decision came eight months after the Pharmaceutical Benefits Advisory Committee recommended that sofosbuvir be listed on the PBS because of “high clinical need”.
This overturned advice from the PBAC a year earlier, in which it recommended against listing the drug because it was likely to have “a high financial impact on the health budget”.
In recommending the drug’s listing, the PBAC warned it was likely to cost taxpayers $3 billion over five years to put 62,000 chronic hepatitis C patients through a course of treatment – three times the Government’s current budgeting.
Though sofosbuvir has been hailed as a “game-changing” medicine that can cure hepatitis C in as little as 12 weeks, its prohibitive price – a course of treatment can cost more than $110,000 – has meant that until now it has been out of the financial reach of most sufferers.
Listing on the PBS means a prescription will cost as little as $37.70 for general patients and $6.10 for concession card holders.
Ms Ley said the combination therapies listed on the PBS had a 90 per cent success rate, and caused fewer side effects than current treatments. She said in most cases patients will only need to take the drug as a pill.
The fact that the Government has budgeted just $1 billion for the measure suggests either that it has managed to negotiate a significant discount with the drug companies, or will eventually need to allocate more money to the effort.
Adrian Rollins
Tribunal snuffs out latest bid against plain packaging
The tobacco industry has lost out in its latest attempt to kill off Australia’s world-leading plain packaging laws.
A bid by tobacco giant Philip Morris to have plain packaging ruled invalid under the terms of Australia’s bilateral investment treaty with Hong Kong has been rejected by the Permanent Court of Arbitration sitting in Singapore.
The ruling is the latest setback for tobacco companies fighting a rearguard action against plain packaging measures, which are being adopted by a growing number of countries, including Britain and Ireland, after coming being enacted in Australia in 2012.
Under the laws, tobacco products must be sold in plain packets carrying graphic health warnings.
The measure has been vehemently opposed by the tobacco industry, which has claimed it infringes on copyright and will drive an increase in trade in illicit tobacco products.
The arbitration ruling means the tobacco industry is running out of legal options to challenge plain packaging.
Soon after the legislation was passed in late 2011, British American Tobacco launched action in the High Court, but its bid was rejected.
Several tobacco-producing countries have also launched action against the legislation under the auspices of the World Trade Organisation, and this bid remains outstanding.
In its latest Position Statement on Tobacco Smoking and E-cigarettes, the AMA said tobacco companies had used packaging to convey messages around social status, values and character, and there were signs that forcing producers to use plain packaging was having an effect rates of smoking.
Related: MJA – The Australian’s dissembling campaign on tobacco plain packaging
A group of studies published in the British Medical Journal found that plain packaging reduced brand appeal and image, and indicated that the proportion of smokers who wanted to quit jumped 7 percentage points following the introduction of plain packaging.
The AMA said that although the measure has not been in place long enough to establish strong evidence of effectiveness, “preliminary research is very promising”.
In addition, it said there was no evidence that plain packaging had led to an increase in the consumption of illicit tobacco.
Adrian Rollins
Latest news:
Deadly attacks raise fears of breakdown in rules of war
Picture credit: IgorGolovniov / Shutterstock.com
Governments and armed groups are being pressured to ensure the safety of patients and health workers in conflict zones amid a spate of high-profile attacks that have left dozens dead and injured.
The World Medical Association, the International Committee of the Red Cross, the World Health Organisation and several other peak health groups have jointly called on national governments and non-state combatants to adhere to international laws regarding the neutrality of medical staff and health facilities, and ensuring this commitment is reflected in armed forces training and rules of engagement.
The call follows an admission by the US military that a deadly attack on a Medecins Sans Frontieres (MSF) hospital in Kunduz in which 30 people were killed – including 13 staff and 10 patients – was a tragic mistake.
“This was a tragic and avoidable accident caused primarily by human error,” the US’s top commander in Afghanistan, General John Campbell, said, adding that the error was “compounded by systems and procedural failures”.
Though the location of the MSF hospital was widely known, a series of technical and operational errors led the crew of the US gunship that launched the devastating attack to mistake the hospital for the headquarters of the Afghan security service, which had been briefly seized by the Taliban.
The strike co-ordinates for the security building took the aircraft to an open field, so the aircrew decided to launch the attack on the nearest building that matched the description they had been given, which turned out to be the MSF hospital. The aircrew, and the operational command in Kabul, did not check the co-ordinates of the planned target against a “no-strikes” list.
MSF International President Dr Joanne Liu said the incident showed the deadly consequences of any ambiguity about how international humanitarian law applied to medical work in war.
“We need a clear commitment that the act of providing medical care will never make us a target. We need to know whether the rules of law still apply,” Dr Liu said.
The Kunduz attack has added to the urgency for action to be taken to ensure the safety of medical staff and hospitals in combat zones.
The International Committee of the Red Cross (ICRC), through its Health Care in Danger project, recorded 2398 attacks on health workers, facilities and ambulances in just 11 countries between January 2012 and the end of last year.
Policy and Political Affairs Officer for the ICRC’s Australian mission, Natalya Wells, said such attacks were not new, and were virtually a daily occurrence.
Ms Wells often health workers were caught in the cross-fire, particularly as a result of indiscriminate attacks in urban areas.
But she said that on occasion they were also being deliberately targeted, underlining the need for all combatants to respect the Geneva Conventions.
Ms Wells said that through the Health Care in Danger project, the ICRC was working with governments, armed forces and non-state combatants to improve awareness of, and respect for, laws and conventions around the protection of patients, health workers and medical facilities, particularly in conflict zones.
As part of the effort, governments attending the 32nd International Conference of the Red Cross and Red Crescent between 8 and 10 December were expected to back a resolution reaffirming their commitment to international humanitarian law and a prohibition on attacks on the wounded and sick as well as health care workers, hospitals and ambulances.
In addition, Ms Wells said the ICRC had held meetings with 30 non-state combatant groups from four continents about international humanitarian law and the rules of armed conflict.
The discussions have included incorporating knowledge of these conventions into their training, backed by sanctions for any breaches.
Promisingly, Ms Wells said that so far “one or two” non-state armed groups, though not signatories to the Geneva Conventions, have discussed creating a similar code of conduct for their forces.
Adrian Rollins
MJA reviewers
Reviewers (submitted between 31/10/2014 and 1/11/2015)
Penelope A Abbott
Ehtesham A Abdi
Sarah J Abrahamson
Leon A Adams
Barbara-Ann Adelstein
Stephen Adelstein
Michael A Adena
Roman A Ahmed
Philip D Aitken
Karyn E Alexander
Charles Algert
Roger WG Allison
Steve J Allsop
Craig S Anderson
Ian P S Anderson
Warwick H Anderson
David Andresen
Gavin Andrews
Anders Aneman
Rachel A Ankeny
John S Archer
Nigel R Armfield
Bruce K Armstrong
Carolyn Anne Arnold
Peter C Arnold
Constantine N Aroney
Rosalie Aroni
Peter Arvier
Michael A Ashby
Eugene Athan
John J Atherton
David N Atkinson
Peter D Baade
Rodney J Baber
Leon A Bach
Tim Badgery-Parker
Peter A Baghurst
Paul M Bailey
Rob Baird
Deborah F Baker
Ross I Baker
Mohammed S Ballal
Zsolt J Balogh
Lilon G Bandler
Michael Barakate
Amanda Barnard
David J Barnes
Andrew Bartholomaeus
Harold Bartlett
Michael B Barton
Darryl L Bassett
Robert G Batey
Malcolm W Battersby
Peter E Baume
Justin J Beilby
Anthony J Bell
Narelle Bell
Christine C Bennett
Jill Benson
Roy G Beran
Yemima Berman
Martin Berry
Andrew D Bersten
James D Best
John B Best
JH Nicholas Bett
Laurent Billot
Sara Bird
Roderick O Bishop
Renee Bittoun
Deborah A Black
David J Blacker
Christopher F Bladin
Neville Board
Felix Bochner
E Leslie Bokey
Stephen N Bolsin
Patrick GM Bolton
Chelsea J Bond
Michael A Bonning
Barbara J Booth
Robert Booy
Craig S Boutlis
Steven J Bowe
Simon D Bowler
Anne-Marie Boxall
Steven C Boyages
Ian W Boyd
Frances M Boyle
Michael J Boyle
Clare E Bradley
George Braitberg
Jeffrey Braithwaite
Annette J Braunack-Mayer
Bruce J Brew
David B Brieger
Esther Briganti
Nancy E Briggs
Julie K Brimblecombe
Helena C Britt
Henry Brodaty
Wendy E Brodribb
Julia ML Brotherton
Jamie Bryant
David J Buckley
John F Buckley
Stephen R Buckley
Michael D Buist
Chris Bullen
Jonathan GW Burdon
Paul Burgess
John Burke
Bryan H Burmeister
John R Burnett
Colin D Butler
Julie E Byles
Joshua Byrnes
Petra T Bywood
John F Cade
Dominique A Cadilhac
J William F Cairns
W Ian Cameron
David G Campbell
Dianne Campbell
Patricia Campbell
Terence J Campbell
Gideon A Caplan
Magnolia Cardona-Morrell
Marion G Carey
John B Carlin
John Carmody
Vaughan J Carr
Gerard E Carroll
Phillip J Carson
Owen BJ Carter
Ian D Caterson
Steven J Chadban
Leanne Chalmers
Alex J Chamberlain
Albert KF Chan
Lewis Chan
Raymond C Chan
Michael G Chapman
Alex Chaudhuri
Ruchir Chavada
Celia S-W Chen
Allen C Cheng
Ian R Cheong
Derek PB Chew
Cherie Ying Chiang
E Mary Chiarella
Jun Chih
Tanya N Chikritzhs
James YJ Choi
Patty Chondros
Tim Churches
Flavia M Cicuttini
Jonathan Clark
Stephen L Clark
Caroline F Clarke
Stephen J Clarke
Moira A Clay
Alan R Clough
Stephen Colagiuri
Justin J Coleman
Peter J Collignon
Veronica R Collins
Brian T Collopy
David M Colquhoun
Tracy Comans
Elizabeth J Comino
Jennifer J Conn
Mark Connor
Matthew C Cook
Michael D Coory
William Coote
Charles F Corke
Marcello Costa
Sophia Couzos
Brendon J Coventry
Terry J Coyne
Shona Crabb
Maria E Craig
Pippa Craig
Helen M Creasey
T John Croese
Louise Cullen
Anthony L Cunningham
Frances C Cunningham
Bart J Currie
David Currow
Eleonora Dal Grande
Luciano Dalla Pozza
Andrew Dalton
Seamus E Dalton
ER David Dammery
Santosh Daniel
John Daniels
Lynne A Daniels
Anthony M Dart
Mike Daube
Sandra K Davidson
Lucy Davies
Gavin A Davis
Ian D Davis
Joshua S Davis
Andrew H Dawson
Carolyn A Day
Richard O Day
John F de Campo
Caroline M de Costa
Nicholas H de Klerk
Christopher B Del Mar
Geoff Delaney
Martin B Delatycki
Apo Demirkol
Justin T Denholm
Catherine A D’Este
Karen M Detering
Peter G Devitt
Jan E Dickinson
Hugh G Dickson
Paul M Dietze
John B Dixon
Gordon Doig
Xenia Dolja-Gore
Leo T Donnan
Kirsty Douglas
Jo A Douglass
Susan M Dovey
Michael A Downes
Robert P Dowsett
Tim R Driscoll
Dino Druda
Olaf H Drummer
Stephen J Duckett
Michael J Dudley
Anne E Duggan
James A Dunbar
Peter Dwyer
John R Dyer
Peter R Ebeling
Matthew Edwards
Paul V Effler
Sam Egger
John A Eisman
Elif I Ekinci
Diann S Eley
Jaklin A Eliott
Steven R Ellen
Pete M Ellis
David A Ellwood
Adam G Elshaug
Jon D Emery
Michael WN Epstein
Sue M Evans
Mark Everard
Ben D Ewald
Daniel P Ewald
Paul A Fagan
Paul P Fahey
Christopher K Fairley
Michael Falster
Elizabeth A Farmer
Anne-Maree Farrell
Michael Farrell
A Michael Fasher
Thomas A Faunce
Steven G Faux
Michael R Fearnside
John K Ferguson
David W Firman
Kenneth D Fitch
Gerard J FitzGerald
Mark C B Fitzgerald
Paul B Fitzgerald
Arthas Flabouris
Jeff Flack
Maree Flaherty
Louisa Flander
John I Fleming
John P Fletcher
Leon Flicker
Eleanor M Flynn
Brett H Forge
S Lesley Forster
Craig L Fry
Gordian WO Fulde
John S Furler
Belinda J Gabbe
Jamie Gaida
Alexander S Gallus
Glenn J Gardener
Alan Garner
Paul H Gavel
Kurt Gebauer
Charles RP George
Emma Gibbs
John Gibson
Heather F Gidding
Gwendolyn L Gilbert
Marisa T Gilles
Rodney C Givney
Nicholas J Glasgow
Katie Glass
Sharon R Goldfeld
John M Goldsmid
Phillip D Good
J Jill Gordon
Louisa Gordon
Alexandra S Gorelik
C Roger Goucke
Linda V Graudins
Angus J Gray
Timothy J Gray
M Lindsay Grayson
Anthony J Green
Shaun L Greene
David Greenfield
Jerry R Greenfield
Paul F Gross
Russell L Gruen
Sylvia Guenther
Charles S Guest
Hasantha Gunasekera
Leena Gupta
Steven L Guthridge
Paul S Haber
Sandra M Hacker
Kay Haig
Ian E Haines
George Halasz
Sally J Hall
Wayne D Hall
P Shane Hamblin
Ian R Hamilton-Craig
Alan W Hampson
Graeme J Hankey
Terry J Hannan
Richard W Harper
Todd Harper
David C Harris
Ian A Harris
John Harris
Mark F Harris
Phillip J Harris
Gunter Hartel
Mary Anne Hartley
Melissa Haswell-Elkins
Andrew Hayen
Noel E Hayman
Christopher H Heath
Debra Hector
William F Heddle
Edward B Heffernan
Delia V Hendrie
Geoffrey Henley
Ana Herceg
Wayne M Herdy
Richard P Herrmann
Ian B Hickie
David R Hillman
Sara Hitchman
Christopher D Hogan
Patrick G Hogan
John D Horowitz
Robert L Horvath
Kenneth F Hossack
Anthony K House
Benjamin P Howden
Laurie G Howes
Wendy E Hoy
Rae-Lin Huang
Ben Hudson
Bernard J Hudson
J Nicoll (Nicky) Hudson
Lisa Hui
John S Humphreys
Joseph Hung
Roger W Hunt
David Hunter
Ernest M Hunter
Jennifer Hunter
Elizabeth Hurrion
Sarah J Hyde
Zoe Hyde
Susan Ieraci
Warrick J Inder
Timothy JJ Inglis
Timothy W Isaacs
Geoffrey K Isbister
James P Isbister
Alan F Isles
Rebecca Q Ivers
Claire L Jackson
Paul Jagals
Ian James
Stephen Jan
Tania Janusic
George Javorsky
Gary P Jeffrey
V Michael Jelinek
Paul Jennings
George Jerums
Ian Johnson
Paul DR Johnson
Renea Johnston
Barbara F Jones
D Gareth Jones
D Brian Jones
Mark A Jones
Michael Jones
Penelope Jones
Anthony F Jorm
Matthew D Jose
Rodney T Judson
Stephen M Jurd
Jon N Jureidini
Ian J Kamerman
Leah Kaminsky
Melissa S-L Kang
Andrew H Kaye
Damien Kee
Marc JNC Keirse
Margaret A Kelaher
Heath A Kelly
Lisa Kelly
Robert I Kelly
Michael C Kennedy
Peter G Kerr
Ian H Kerridge
Alison M Kesson
Michael R Kidd
Monique Kilkenny
Thomas E Kimber
Stuart A Kinner
Adrienne C Kirby
Stephen Kleid
Timothy Kleinig
Christopher S Kneebone
Andrew W Knight
Bogda Koczwara
Ann P Koehler
Jen Kok
Pieter J Koorts
Steven Kossard
Joe M Kosterich
Gabor T Kovacs
Emma E Kowal
Vicki L Krause
Edwin Kruys
Paul A Kubler
Dennis L Kuchar
Maarit Laaksonen
Matthew M Large
Sarah L Larkins
Ann-Claire Larsen
Murray Laugesen
Gillian A Laven
Amanda J Leach
Karin Leder
Katherine Lee
Richard P Lee
Peter A Leggat
James Leigh
Christopher Lemoh
Nat P Lenzo
David E Leslie
Lucy N Lewis
Simon Lewis
Steven J Lewis
Shu Qin Li
Wenbin Liang
Ee Mun Lim
Wendy L Lipworth
Mark Little
Sing Kai Lo
Bebe Loff
David FM Looke
Charles W Lott
Clement Loy
Michaela Lucas
Kehui K Luo
Sharyn Lymer
Kristine Macartney
Graeme A Macdonald
Peter S MacDonald
Jennifer H MacLachlan
William (Bill) J Madden
Guy J Maddern
Ian Maddocks
Dianna J Magliano
Roger S Magnusson
Graeme P Maguire
Donna B Mak
Lynette M March
Peter G Markey
Tania Markovic
Guy B Marks
Alexandra L Markwell
Julia V Marley
Andrew J Martin
Alison Marwick
Colin L Masters
John D Mathews
John JS Mattick
Jeremy M McAnulty
Grant McArthur
Brian R McAvoy
Kristin E McBain-Rigg
W John H McBride
Geoffrey W McCaughan
Kieran A McCaul
Geoffrey J McColl
Judith McCool
Joseph G McCormack
Robyn Anne McDermott
Peter J McDonald
Michael A McDonough
Neil W McGill
Diana R McKay
Joanne E McKenzie
Mary-Louise McLaws
Hamish McManus
Donald McNeil
Barbara McPake
Jacqueline K Mein
Craig Mellis
Muhammed A Memon
Richard M Mendelson
J Alasdair Millar
Jeremy L Millar
Belinda R Miller
Emma R Miller
Graeme C Miller
Roger Laughlin Milne
I Harry Minas
Adrian Mindel
Philip B Mitchell
Mohammadreza Mohebbi
Michael Montalto
A Rob Moodie
David J Moore
Elizabeth M Moore
Rachael Moorin
Susan J Morgan
Robert FW Moulds
Alison M Mudge
Sandy Muecke
Wendy Muircroft
H Konrad Muller
Raymond J Mullins
Kevin Murray
Richard B Murray
Arthur (Bill) W Musk
Ludomyr J Mykyta
Balakrishnan (Kichu) R Nair
Mark R Nelson
Peter W New
Jonathan W Newbury
Louise K Newman
Harvey H Newnham
Ainsley J Newson
Hanh TT Ngo
Peter K Ngo
Cattram Nguyen
Kathleen M Nicholls
Marcus Nicol
Suzanne Nielsen
Paul Nisselle
Theophile (Theo) Niyonsenga
Antony Nocera
David A Nolan
Terence M Nolan
Don Nutbeam
Cornelius (Kees) M Nydam
Diana O’Halloran
Paula O’Brien
Dianne L O’Connell
Rachel L O’Connell
Nicholas J O’Connor
Kerin O’Dea
Jake Olivier
Ian N Olver
Susanne P O’Malley
Liliana Orellana
Peter K O’Rourke
Matthew O’Sullivan
Donald R Packham
Colin B Page
Pamela Palasanthiran
Neil R Parker
William A Parsonage
Sally Partridge
Dennis R Pashen
Anushka Patel
Jillian Patterson
Brian B Peat
David P Peiris
Carmelle Peisah
Brita AK Pekarsky
Stella Pendle
David G Penington
Andrew G Penman
Roger J Pepperell
Martin Pera
Vlado Perkovic
Andrew Perry
Alexandra Phelan
Christine B Phillips
Avinesh Pillai
S Praga Pillay
Hans C Pols
Rene G Pols
P Gawaine Powell Davies
Jennifer R Powers
Douglas A Pritchard
Anthony M Proietto
Brendan Quinn
Michael A Quinn
Janette C Radford
Shripada Rao
William D Rawlinson
Tim RH Read
Andrew M Redmond
Anne Rees
Carole Reeve
Glenn EM Reeves
Alun H Richards
Bernadette J Richards
Brian H Richards
Gary E Richardson
Jeffrey R Richardson
Geoffrey J Riley
Malcolm D Riley
Matthew Rimmer
Ian T Ring
Darren M Roberts
Iain K Robertson
J Owen Robinson
Monica C Robotin
David M Roder
Gary D Rogers
Bronwen Ross
Glynis P Ross
Nicola Ross
Elizabeth E Roughead
George L Rubin
Anthony W Russell
Lesley M Russell
Christopher J Ryan
Louise M Ryan
Michael Ryan
Sabe Sabesan
Gary Sacks
Salih A-S Salih
Shahneen Sandhu
Michael J Sandow
W Peter Saul
Leslie Schrieber
Brenton L Schuetz
Rosalie Schultz
Anthony Scott
Ian A Scott
David J Scrimgeour
Clair Scrine-Bradfield
Paul A Scuffham
Katrina J Scurrah
Eva Segelov
Warwick S Selby
Tarun Sen Gupta
Tim Senior
Jillian R Sewell
William A Sewell
Anurag Sharma
Rashmi Sharma
Mary-Jane S Sharp
Harshvardhan Sheorey
Rupendra N Shrestha
Stephen P Shumack
Kenneth A Sikaris
Morry Silberstein
Gregory Siller
Leon A Simons
Rodney D Sinclair
Andrew H Singer
Dan J Siskind
Freddy Sitas
Peter Sivey
Tim Slade
Adrian Sleigh
Richard A Smallwood
Dale C Smith
David E Smith
David W Smith
Julian A Smith
Karen Smith
Mitchell M Smith
Richard S W Smith
William B Smith
Tim J Smyth
Ann C Solterbeck
Ernest R Somerville
Richard Speare
Denis Spelman
Allan D Spigelman
Geoffrey K Spurling
Piyush M Srivastava
Rosemary A Stanton
David G Steel
Amanda M Stephens
Matthew Stevens
Christopher E Stevenson
Mark Stevenson
Jessica M Stewart
Johannes U Stoelwinder
Mark Stoove
H Victor Storm
Nicholas W Stow
Roger P Strasser
Alison Street
Allan D Sturgess
Danny H Sullivan
David R Sullivan
Suresh Sundram
Rajah Supramaniam
Tatiana Surzhina
Tom R Sutherland
Jeffrey Szer
Michael L Talbot
Chun Wah M Tam
Colman B Taylor
Hugh R Taylor
Peter L Thompson
Sandra C Thompson
James Tibballs
Sean Tobin
Shilu Tong
Steven YC Tong
Robyn Toomath
Adrienne J Torda
Huy A Tran
Brian M Tress
Stephen C Trumble
Philip G Truskett
Bernard E Tuch
Robin M Turner
Ida Twist
Jason A Tye-Din
Flora Tzelepis
Shahid Ullah
Edward Upjohn
Lydia Upjohn
Tim Usherwood
Mieke L van Driel
Helen J Van Gessel
Paul Varghese
Phillip C Vecchio
Mark GK Veitch
Elmer V Villanueva
Ioana Vlad
Russell G Waddell
Victoria (Tori) A Wade
Mark L Wahlqvist
Jennifer Walker
Thomas D Walker
Merrilyn M Walton
Han Wang
Joanna JJ Wang
Zhiqiang Wang
Michael R Ward
Vicki-Ann Ware
Orli Wargon
Lachlan J Warren
D Ashley R Watson
Bruce P Waxman
Peter Wein
Leo Westbury
R Michael Whitby
Andrew V White
Ben White
Ian M Whyte
Bridget Wilcken
Kay A Wilhelm
Garry J Wilkes
Lesley M Wilkes
Dominic JC Wilkinson
Amanda Wilson
Ian G Wilson
Ingrid Winship
Erica M Wood
Fiona M Wood
Peter Wood
Richard J Woodman
Michael C Woodward
Paul S Worley
Roxanne L Wu
Rosemary Wyber
Fenglian Xu
Ian A Yang
Mark W Yates
Bu B Yeap
Josephine Yeatman
Sonia Yip
Doris YL Young
Bing Yu
Kally Yuen
Farhat Yusuf
Jeffrey D Zajac
John R Zalcberg
Nikolajs Zeps
Yuejen Zhao
John B Ziegler
Nicholas A Zwar
Building on the rich heritage of the Medical Journal of Australia
My professional interests span clinical practice, medical education and research, medical leadership, health policy and social justice. My goals as editor are to build on the outstanding DNA of the Journal, further increasing its relevance and readability, and attracting the highest quality submissions. We will aim to build on the Journal’s rich heritage by continuing our practice of publishing the best clinical science papers that have the potential to transform practice, including clinical trials and comparative effectiveness research. We will also aim to inform readers on advances in medical education, and cover issues from medical leadership to re-engineering our health system. We will continue to seek expert reviews, editorials and commentaries, meta-analyses and guidelines, and the latest news and information that everyone in practice needs to know. It is my goal to reinforce the unique role that the Journal plays as the pre-eminent publisher of Australian medical research and as a vital platform for translating research into practice, as well as helping to inform the broader health policy debate. This is part of the Journal’s success and why it is relevant to clinicians, researchers and academics across the nation.
The MJA is prestigious and influential, but another advantage to publishing with us is that much of the content including our research content is published freely on our website at mja.com.au, without the waiting period often imposed by other journals. I can also assure readers that as Editor-in-Chief, I have a guarantee of editorial independence and I will fiercely guard this independence on your behalf. For the nearly 32 000 subscribers who receive the MJA in print, and the many others who read the Journal online, the team will work tirelessly to provide the best medical journal experience possible.
We live in a world that, in terms of connectivity through social media, is rapidly shrinking, and the MJA has an important role to play not just nationally but globally. We will therefore now be encouraging locally relevant international articles. And we will continue to tackle in our pages articles that highlight the tough health issues we all face and provide possible solutions, from the health needs of Indigenous Australians to the health impacts of global migration, population growth, dwindling resources, an ageing population and climate change, to name a few. We will look both out to the world and across Australia to find the objective data that can help guide us all. We will seek balance among the many expert opinions and will aim at all times to be rigorous, evidence-based and transparent.
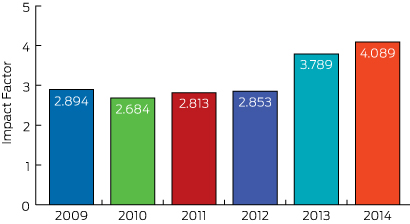
Whether any of us like it or not, our performance in medicine is being increasingly measured and critiqued, and it’s no different for medical journals. Clinicians and academics want to publish in the best medical journals and one metric applied universally is the impact factor, calculated by counting the mean number of citations received per article published during the previous 2 years. In the best journals, editors arguably “live and die” by the journal impact factor published each year. The impact factor is flawed (some argue fatally so) and is not used by the National Health and Medical Research Council; but it can’t be ignored either!1,2 In 2015, the MJA, your national journal, ranks in the top 20 general medical journals worldwide and has a highly respectable impact factor of 4.089 (Box, previous page). I am pleased to say that the impact factor of the MJA has risen and I anticipate over the coming years that it will continue to rise (as will other metrics of excellence) as we further increase the quality and reach of what we publish.
We welcome your best work being submitted for consideration. Our acceptance rate is currently falling (as marks all of the best medical journals) but I can pledge that your medical articles will be expertly peer reviewed and edited before publication. The editorial team will do its utmost to ensure it makes the best possible decisions, and we will work hard with authors to help them publish polished, excellent contributions.
Finally I would like to acknowledge and thank Professor Charles Guest in his capacity as Interim Editor-in-Chief for his stewardship of the Journal in the second half of 2015. He has been instrumental in supporting our editors and maintaining the continuity and the quality of the Journal.
Thank you for reading the MJA. You can expect that the Journal will be further increasing its scientific reputation and international presence over the next few years, and I hope you will be part of it if you have a contribution you wish to make. We welcome suggestions and feedback so we can further improve the Journal on your behalf. I am committed to strengthening your clinical practice through its pages and look forward to our journey together.

 more_vert
more_vert