Most glomerulonephritides, even the more common types, are rare diseases. They are nevertheless important since they frequently affect young people, often cannot be cured, and can lead to chronic kidney disease, including end-stage renal failure, with associated morbidity and cost. For example, in young adults, IgA nephropathy is the most common cause of end-stage renal disease. In this Seminar, we summarise existing knowledge of clinical signs, pathogenesis, prognosis, and treatment of glomerulonephritides, with a particular focus on data published between 2008 and 2015, and the most common European glomerulonephritis types, namely IgA nephropathy, membranous glomerulonephritis, minimal change disease, focal segmental glomerulosclerosis, membranoproliferative glomerulonephritis, and the rare complement-associated glomerulonephritides such as dense deposit disease and C3 glomerulonephritis.
Preference: Infectious Diseases and Parasitology
434
[Perspectives] Vaccination: a vexatious history
An unanticipated effect of the success of mass immunisation campaigns in western countries, no less than in Asia and the global south, is the more that vaccines have reduced the incidence of formerly deadly childhood diseases, the harder it becomes to convince parents that it is necessary for their own child to be vaccinated. This is particularly the case with a new generation of parents too young to have experienced measles or mumps for themselves, never mind diseases such as polio that cast a shadow over their grandparents’ childhoods.
[World Report] Can open-source drug development deliver?
Open-source drug development involves open data sharing, collaboration, and results sharing. The aim is to produce new drugs for neglected diseases. But can it work? Tatum Anderson reports.
Ebola crisis: the world must do better
The reputation of the global system for preventing and responding to infectious disease outbreaks has taken a battering in the wake of the west African Ebola epidemic.
Yet a prestigious Independent Panel believes it is possible to rebuild confidence and prevent future disasters, releasing a roadmap of 10 interrelated recommendations for national governments, the World Health Organisation, non-government organisations and researchers.
The Independent Panel on the Global Response to Ebola, launched jointly by the Harvard Global Health Institute and the London School of Hygiene and Tropical Medicine, spent months reviewing the worldwide response to the outbreak that began in 2013.
“The west African Ebola epidemic … was a human tragedy that exposed a global community altogether unprepared to help some of the world’s poorest countries control a lethal outbreak of infectious disease,” the Panel wrote in The Lancet.
“The outbreak continues … It has infected more than 28,000 people and claimed more than 11,000 lives, brought national health systems to a halt, rolled back hard-won social and economic gains in a region recovering from civil wars, sparked worldwide panic, and cost several billion dollars in short-term control efforts and economic losses.”
See also: AMA pressure on government to act
The Panel said its goal was to convince high-level political leaders worldwide to make necessary and enduring changes to better prepare for future outbreaks while memories of the human costs of inaction remained vivid and fresh.
It identified four key phases of inaction:
- December 2013 to March 2014, when Guinea’s lack of capacity to detect the virus allowed it to spread to neighbouring Liberia and Sierra Leone;
- April to July 2014, when intergovernmental and non-government organisations started to respond, health workers struggled to diagnose patients and provide effective care, national authorities played down the scope of the outbreak, and WHO and the US CDC sent expert teams but withdrew them prematurely;
- August to October 2014, when global attention and responses grew, but so did panic and misinformation, leading to unnecessary and harmful trade and travel bans; and
- October 2014 to September 2015, when cases began to decline, and large-scale global assistance started to arrive, albeit with weak coordination and a lack of accountability for the use of funds.
“This Panel’s overarching conclusion is that the long-delayed and problematic international response to the outbreak resulted in needless suffering and death, social and economic havoc, and a loss of confidence in national and global institutions,” the Panel said.
“Failures of leadership, solidarity and systems came to light in each of the four phases. Recognition of many of these has since spurred proposals for change. We focus on the areas that the Panel identified as needing priority attention and action.”
The Panel made 10 recommendations:
- develop a global strategy to invest in, monitor, and sustain national core capacities;
- strengthen incentives for early reporting of outbreaks and science-based justifications for trade and travel restrictions;
- create a unified WHO Centre for Emergency Preparedness and Response with clear responsibility, adequate capacity, and strong lines of accountability;
- broaden responsibility for emergency declarations to a transparent, politically protected Standing Emergency Committee;
- institutionalise accountability by creating an independent Accountability Commission for Disease Outbreak Prevention and Response;
- develop a framework of rules to enable, govern and ensure access to the benefits of research;
- establish a global facility to finance, accelerate, and prioritise research and development;
- sustain high-level political attention through a Global Health Committee of the Security Council;
- a new deal for a more focused, appropriately financed WHO; and
- good governance of WHO through decisive, time-bound reform, and assertive leadership.
“The human catastrophe of the Ebola epidemic that began in 2013 shocked the world’s conscience and created an unprecedented crisis,” the Panel concluded.
“The reputation of WHO has suffered a particularly fierce blow. Ebola brought to the forefront a central question: is major reform of international institutions feasible to restore confidence and prevent future catastrophes? Or should leaders conclude the system is beyond repair and take ad hoc measures when the next major outbreak strikes?
“After difficult and lengthy deliberation, our Panel concluded major reforms are warranted and feasible.”
Maria Hawthorne
Cheaper drugs a path to better health
Medicines save lives and improve health and wellbeing when they are available, affordable, and properly used.
With Aboriginal and Torres Strait Islander people experiencing double the rate of chronic illnesses than their non-Indigenous peers, access to affordable prescription medicines is essential. Unfortunately, Aboriginal and Torres Strait Islander people are not accessing medicines at a level that is appropriate to their needs, with cost being reported as a major barrier.
As evidenced by the Closing the Gap (CTG) Pharmaceuticals Benefits Scheme (PBS) Co-payment measure, reducing out-of-pocket costs for medications increases access to, and use of medications, ultimately resulting in improved health outcomes.
Since its inception in 2010, the CTG PBS Co-payment measure has increased access to medicines for more than 280,000 Aboriginal and Torres Strait Islander people in urban and rural areas, by reducing or removing the patient co-payment for PBS medicines. Substantial reductions in hospitalisations have also been seen in areas with the greatest uptake of the CTG PBS Co-payment incentive.
While the outcomes under this measure have been encouraging, there is still a long way to go until we achieve equality in access to medicines for Aboriginal and Torres Strait Islander people.
A good starting point is to promote the CTG PBS Co-payment more widely to all prescribing doctors across Australia, to increase awareness and uptake of the initiative and build on its success.
In August 2012, Australian Doctor reported that, alarmingly, thousands of doctors were unaware of the existence of the CTG PBS Co-payment measure – an important initiative that has the potential to make a real contribution to closing the gap.
With chronic diseases being one of the main reasons for the life expectancy gap between Indigenous and non-Indigenous people, it is unacceptable that so many Australian doctors are unaware of such an important scheme.
Doctors working in Aboriginal and Torres Strait Islander Community Controlled Health Services are generally aware of this initiative, and regularly prescribe medications covered by the CTG PBS Co-payment measure for the benefit of their patients. However, many doctors working in mainstream general practice may not be aware of this scheme.
To participate in the CTG PBS Co-payment measure, practices must be able to first identify eligible Aboriginal and Torres Strait Islander patients. All patients across Australian medical practices should be asked whether they identify as being of Aboriginal and Torres Strait Islander origin by asking the National Standard Identification question – ‘Are you of Aboriginal or Torres Strait Islander origin?’ Once Indigenous patients are recognised, they are eligible to be registered for co-payment assistance.
Improved access to medicines is critically important if we are to see generational change in health outcomes for Aboriginal and Torres Strait Islander people.
The Australian Medical Association encourages all medical practitioners to increase their awareness of the CTG PBS Co-payment measure to improve health outcomes for Aboriginal and Torres Strait Islander patients.
A patient with sarcoidosis and a cryptococcal infection of the skull
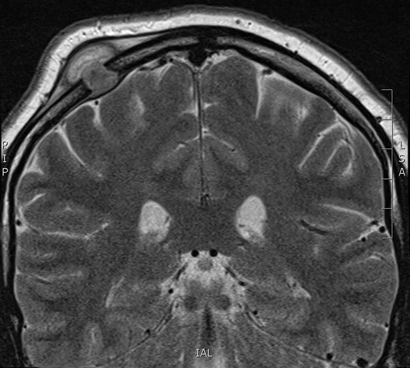
A 29-year-old man of European ancestry, with a history of sarcoidosis treated with low-dose steroids, presented with a progressive swelling of the skull which had appeared 3 weeks earlier.
Physical examination revealed a 2.5 cm soft swelling of the right parietal part of the skull. A contrast-enhanced magnetic resonance imaging scan of the head showed a solitary lesion of the right parietal bone measuring 9 mm × 17 mm.
After neurosurgical resection, pus cultures grew Cryptococcus neoformans.
In the absence of disseminated cryptococcosis, the patient was treated successfully with oral fluconazole. Current literature suggests sarcoidosis as a risk factor for cryptococcosis, independent of the use of immunosuppressive agents.1,2
News briefs
Parechovirus warning from ASID
The Australasian Society for Infectious Diseases (ASID) has found that more than 100 Australian infants had developed brain damage and developmental delays 1 year after they were hospitalised with the virus in 2013 and 2014, according to a report in The Straits Times. The symptoms include rashes, irritability, muscle twitches and seizures, fever and diarrhoea, said ASID. In severe cases, it can cause hepatitis or encephalitis. Parechovirus is spread like the common cold, by direct contact with nose and throat discharges from sneezing, coughing, saliva, nasal mucus or faeces. There is no vaccine or treatment at present. Starting in December 2013, it spread quickly through parts of Queensland, including Brisbane and the Gold Coast, and over 100 newborn babies were hospitalised. They refused to eat, were lethargic and had high temperatures. The new study followed up on 46 out of 79 of the babies. Half of them showed developmental problems and nearly 20% had significant neurological problems by the time they were 1-year-old. In March, two infants from Toowoomba almost died from the virus. Left fighting for life in intensive care, one of them had to be given painful spinal taps and have her chest cut open.
Soap operas play role in mental health understanding
According to a report in The Guardian, soap operas involving storylines about mental health can play a valuable role in increasing understanding of depression, anxiety and schizophrenia, and in encouraging people with problems to seek help. UK charity Mind conducted a survey of more than 2000 people, which found that half of the respondents who had seen a storyline involving a character with mental health problems said it had helped their understanding of the issues. Nearly a third of people with a mental health problem said they were encouraged to seek help after seeing or reading a news story, while a quarter were prompted to get assistance after seeing a soap opera or drama involving a character with mental illness. Mind, along with Bipolar UK, and Action on Postpartum Psychosis, worked with the soap EastEnders for a storyline over Christmas and the new year about a character with postpartum psychosis, a severe mental illness that normally occurs shortly after giving birth.
[Correspondence] Challenges of rare diseases in China
In 2010 and 2011, two publications1,2 in The Lancet discussed policy making on rare diseases in China. After almost 5 years, some progress has been made, but much more needs to be done.
[Comment] Mind the gap: jumping from vaccine licensure to routine use
The contribution of immunisation to improving childhood survival is one of the great achievements of global health. Driving down further infectious disease burden will require new vaccines, many of which have taken decades to develop. We are entering an era where the path from licensure to widespread routine vaccine implementation requires more than efficacy and safety data; policy recommendations for new vaccines may only be realised through implementation research to determine how to most effectively ensure widespread use.
Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011
This report analyses the impact of nearly 200 diseases and injuries in terms of living with illness (non-fatal burden) and premature death (fatal burden). The study found that chronic diseases such as cancer, cardiovascular diseases, mental and substance use disorders, and musculoskeletal conditions, along with injury contributed the most burden in Australia in 2011. Almost one third of the overall disease burden could be prevented by removing exposure to risk factors such as tobacco use, high body mass, alcohol use, physical inactivity and high blood pressure.

 more_vert
more_vert