In The Lancet, Andrew Appelboam and colleagues1 present the findings of a simple but clinically relevant investigation of a safe and non-invasive treatment for patients with stable supraventricular tachycardia who present to emergency departments. This topic is important because patients with supraventricular tachycardia are common, often recurrent, emergency department attenders, and can require critical care interventions. A Cochrane review2 did not find sufficient evidence to support or refute the effectiveness of the Valsalva manoeuvre to end supraventricular tachycardia.
Preference: Emergency Medicine
202
Dementia ‘flying squads’
Mobile ‘flying squads’ of clinical experts will soon be on-call nationwide to help aged care homes confronting crisis situations because of the violent or extreme behaviour of residents with dementia.
Health Minister Sussan Ley has announced $54.5 million will be used to establish Severe Behaviour Response Teams which can be called in on four hours’ notice to help aged care providers trying to cope with residents posing a significant risk to either themselves or others.
The Minister said the initiative was intended to help minimise the number of times aged care home residents with dementia are “unnecessarily” transferred to higher security or acute facilities.
“Like all of us, aged care residents are most comfortable in a familiar environment and this program will provide that helping hand to better manage people in their current community who exhibit severe behaviour because of their dementia,” Ms Ley said.
“This initiative will provide additional support in a crisis situation to residents, who may be hitting out at people around them, and manage their behaviour so they can remain in their familiar aged care home.”
Under the program the teams, to operate between 7am to 7pm seven days a week, will contact the aged care within four hours of receiving a call to discuss interim action, and within 48 hours will hold either a face-to-face or telehealth conference to work on immediate and longer-term care plans.
The support from the teams is in addition to the work done by the existing Dementia Behaviour Management Advisory Services, and is intended to focus solely on residents that pose a threat to themselves or others, such as hitting out at other patients or staff, breaking furniture or windows, ongoing aggressive behaviour and a history of attempting to leave.
The service, which will cover all Commonwealth-funded residential aged care facilities, will be established and operated by HammondCare, which Ms Ley said had a successful history of providing dementia care to high-need residents.
Under the contract, HammondCare is required to provide the same level of service across the country, regardless of location.
Despite the company’s expertise, the Government has emphasised that the teams will not be a substitute for existing emergency and mental health services.
“As is currently the case, all emergencies will be referred to the appropriate state-based paramedic service, who are responsible for providing an immediate emergency response,” the Health Department said.
More information about the Severe Behaviour Response Teams can be found at: https://www.dss.gov.au/ageing-and-aged-care/older-people-their-families-and-carers/dementia/severe-behaviour-response-teams-information-pack
Dementia research boost
The Federal Government has announced a second round of grants worth $43 million to fund research into the causes, effects, treatment and prevention of dementia.
Health Minister Sussan Ley said the grants, shared among 76 researchers, would help keep Australia at the forefront of international efforts to understand and tackle the devastating disease, which currently afflicts about 330,000 Australians.
Ms Ley said the $43 million was in addition to $35 million already committed to dementia research in August, and was jointly funded by the National Health and Medical Research Council and the Australian Research Council.
The Shadow Minister for Ageing, Shayne Neumann, said the research funding boost was welcome, but called on the Government to release the results of a review into publicly-funded dementia programs that was due to report in June.
Mr Neumann said that, in addition to funding research, the Government should also be investing more into supporting those currently living with dementia and their carers.
Adrian Rollins
AMA in the News
Your AMA has been active on policy and in the media on a range of issues crucial to making our health system better. Below is a snapshot of recent media coverage.
Print/Online
Baby shaking on par with road toll, The Australian, 10 September 2015
New research shows shaking kills as many Australian babies and toddlers as car crashes. AMA President Professor Brian Owler said The Children’s Hospital at Westmead in Sydney was treating a case every month.
AMA urges surgeons to cut bullying, The Age, 11 September 2015
A Sydney senior surgeon whose comments on sexual harassment helped draw attention to widespread bullying in the profession has warned that it will be difficult to fix the problem. AMA President Professor Owler said it would be up to the current generation of surgeons to ‘‘break the cycle’’ of bullying, harassment, and discrimination in the profession.
Calling for review of health fund crisis, The Daily Telegraph, 12 September 2015
Health bodies are demanding a radical review of the private health system as health fund premiums skyrocket, hospital price gouge, and funds slash benefits. AMA President Professor Brian Owler demanded Federal Government intervention as he revealed NIB had removed more than 225 items from its schedule of medical benefits.
Boxer dies after title fight at RSL club, Sydney Morning Herald, 16 September 2015
A 28-year-old Australian boxer has died in a Sydney hospital after being knocked out in an IBF regional title fight. The AMA has released a position statement calling on boxing to be banned from the Olympic Games and the Commonwealth Games.
Medicare review placates AMA by agreeing to stagger changes, The Australian, 17 September 2015
The powerful AMA has won an early concession out of much-anticipated Medicare reforms, with the head of a review taskforce agreeing that recommend changes should be staggered to protect doctor and practice incomes.
‘Junk policies’: the private health cover ripoff, Sydney Morning Herald, 24 September 2015
Fewer than half of all private health insurance policies offer adequate cover for private hospital care, and many patients have no idea what their insurance includes, new figures show. AMA President Professor Brian Owler said policies that insured private patients in only public hospitals were junk policies and should not be allowed.
$20bn addiction to Medicare, Adelaide Advertiser, 28 September 2015
The cost of procedures covered by the Medicare Benefits Schedule has more than doubled to $20 billion a year over the past decade despite much smaller increases to Australia’s population. AMA President Professor Brian Owler said he agreed that Medicare needed to be modernised.
Authorisation to sedate ice addicts welcomed by the AMA, The Age, 28 September 2015
The AMA has welcomed new powers for emergency doctors and nurses to subdue violent ice addicts. AMA president Professor Brian Owler said doctors had already called for all hospitals to have appropriate security to deal with the increasing number of patients affected by ice.
BUPA, nib, Medibank back health review, Australian Financial Review, 29 September 2015
Health Minister Sussan Ley has dismissed the doctors’ lobby’s objections to a review of Medicare, saying the health care system is plagued by ineffective and unnecessary medical procedures and desperately needs reform. AMA President Professor Brian Owler accused Ms Ley of using the review to “cut health funding and health services” and “publicly attack the medical profession”.
Playing doctors and curses, Courier Mail, 29 September 2015
The Turnbull Government has cautioned patients against diagnosing themselves on “Dr Google” and then demanding unnecessary and costly treatments from medicos. AMA president Professor Brian Owler said it was wrong to attack doctors to try to justify cuts to Medicare.
Fees for all finished as uni plan gets the third degree, Adelaide Advertiser, 2 October 2015
Tony Abbott and Christopher Pyne’s controversial plan to allow universities to set their own fees has been dumped, in one of the first major policy shifts of the new Turnball Government. AMA president Professor Brian Owler welcomed the decision, and called on the Government to give students more certainty that degrees will not be priced out of reach.
Backing for RCH doctors, The Herald Sun, 12 October 2015
Victoria’s Health Minister Jill Hennessy has led a resounding show of support for the Royal Children’s Hospital’s demands that children be removed from immigration detention centres. AMA President, Professor Brian Owler, urged Mr Turnbull and Immigration Minister Peter Dutton to intervene.
Surgeon’s road safety plea, The Daily Telegraph, 17 October 2015
AMA President Professor Brian Owler said every new car should by law have autonomous emergency braking to stop rear-end car crashes.
Brain-injury teen stranded by beds deficit, Canberra Times, 23 October 2015
A teenage boy with a critical brain injury was blocked access to the Sydney Children’s Hospital for four days because there were not enough beds, his family was told. AMA President Professor Brian Owler said the incident highlighted that there was an issue with capacity in paediatric hospitals, both at Westmead and the Sydney Children’s Hospital.
Doctors resist camp return of asylum pair, The Age, 12 October 2015
Doctors at Melbourne’s Royal Children’s Hospital refused to discharge an asylum seeker and her child because the immigration department would have sent them back to detention at the expense of their health. AMA Vice President Dr Stephen Parnis said the association had a fundamental problem with keeping children in detention, and had been urging governments to look for any alternative to it for years.
Codeine medicines to be prescription-only next year, The Age, 2 October 2015
Common painkillers such as Nurofen Plus and Panadeine could soon require a doctor’s prescription after a shock decision by Australia’s drug regulator. AMA Vice President Dr Stephen Parnis backed the TGA’s judgement.
Radio
Professor Brian Owler, 2UE Sydney, 10 September 2015
AMA President Professor Brian Owler discussed new research which indicated that shaking kills as many Australian babies and toddlers as car crashes. Professor Owler said the Westmead Children’s’ Hospital treated a case every month.
Professor Brian Owler, 2UE Sydney, 28 September 2015
AMA President Professor Brian Owler talked through his concerns about the upcoming Medicare review and the approach that the Government was taking. Professor Owler believed it would lead to a cut to the number of services patients can access.
Professor Brian Owler, Radio National, 1 October 2015
AMA President Professor Brian Owler talked about the Turnbull Government shaking up the Medicare Benefits Schedule, with Health Minister Sussan Ley launching consultations on a review of nearly 6000 taxpayer-subsidised items on the schedule
Dr Stephen Parnis, 774 ABC Melbourne, 2 October 2015
AMA Vice President Dr Stephen Parnis talked about the rules changing around getting codeine from the chemists. Dr Parnis said the TGA, which determines what things need to put on prescription, has had an inquiry about over-the-counter medications which contain codeine.
Dr Brian Morton, ABC Gippsland, 7 October
AMA Chair of General Practice Dr Brian Morton talked about Mental Health Day and said that all employees were allowed to have ten sick days per year. Dr Morton said but it will still depend on the reason and what you will do with the sick days you will take.
Dr Stephen Parnis, 612 ABC Brisbane, 9 October 2015
AMA Vice President Dr Stephen Parnis discussed calls from health academics to ban energy drinks for people younger than 18 years of age. Dr Parnis said stimulants in the products could cause heart rates to reach dangerously high levels, arrhythmias, problems to blood vessels, difficulties sleeping or anxiety.
Dr Stephen Parnis, 3AW Melbourne, 11 October 2015
AMA Vice President Dr Stephen Parnis talked about Royal Children’s Hospital doctors protesting the detention of children in Australian detention centre. Dr Parnis said the AMA is very supportive of getting all children out of immigration detention and says they can’t see any good coming out of the situation.
Dr Brian Morton, Radio National. 21 October 2015
AMA Chair of General Practice Dr Brian Morton talked about the idea of shared doctor appointments. Dr Morton said privacy could be an issue in shared appointments.
Professor Brian Owler, ABC NewsRadio, 23 October 2015
AMA President Professor Brian Owler talked about a new domestic violence campaign being launched by the AMA. Professor Owler said doctors are being encouraged to report domestic violence.
Professor Brian Owler, 2UE Sydney, 23 October 2015
AMA President Professor Brian Owler discussed the Sydney Children’s Hospital turning away a teenage boy with a brain injury because there were not enough beds.
Television
Professor Brian Owler, Sky News Sydney, 27 September 2015
AMA President Professor Brian Owler talked about the Federal Government reviewing the Medicare system. Dr Owler said the AMA were willing to engage with the Federal Government, but says their discussion paper does not allow new procedures to be added.
Professor Brian Owler, Channel 9, 12 October 2015
AMA President Professor Brian Owler speaks to the Today Show about the Royal Children’s Hospital in Melbourne remaining locked in a bitter dispute with the Federal Government over their refusal to discharge asylum seeker children.
Professor Brian Owler, ABC News 24, 23 October 2015
AMA President Professor Brian Owler talked about the AMA launching a new domestic violence campaign, including a video encouraging patients to confide in their GPs. Professor Owler said there were “far too many” cases of domestic violence, affecting both women and children.
Dr Stephen Parnis, ABC News 24, 28 September 2015
AMA Vice President Dr Stephen Parnis discussed a Four Corners investigation that claimed the medical profession was over-servicing patients and ordering wasteful and potentially dangerous scans. Dr Parnis denied that doctors were over-servicing, but said there was a lot the AMA agrees with when it comes to more judicious care.
Decline in alcohol related injuries thanks to CBD lockout laws, research finds
The CBD lockout laws were a controversial move when they were introduced in February 2014. However research published in the Medical Journal of Australia has found they have been successful in reducing alcohol related injuries at St Vincent’s hospital.
The NSW Government banned the sale of alcohol from 10pm, stopped the service of shots from midnight and introduced a 1:30am lockout law with alcohol being stopped at 3am at most hotels, pubs and clubs.
Injuries classified under Australasian triage categories 1 (immediately life-threatening) and 2 (imminently life-threatening, important time-critical treatment, very severe pain) were analysed from St Vincent’s Emergency Department Information System data for the 12 months before and the 12 months after the lockout law changes.
Of 13 110 category 1 and 2 presentations during the 2-year period, 1564 (4.3%) involved patients with an alcohol-related serious injury: 318 (4.9% of all presentations) before the introduction of the new regulations and 246 (3.7%) in the subsequent 12 months.
Professor Gordian Fulde, Director of the Emergency Department at St Vincent’s says the laws may be working to reduce alcohol related injuries.
“After the introduction of the regulatory changes, there was a significant decrease in the number of seriously injured patients during HAT, from 140 presentations (10.4% of presentations) before the change to 106 (7.8%) after their introduction, a relative reduction of 24.8%.
“This change was seen throughout the week, but was especially marked at weekends.”
Visit the Medical Journal of Australia to read the research.
Latest news:
- Falls a costly health burden
- Emergency doctors as stressed as soldiers
- Testing times! Choosing Wisely when it comes to monitoring type 2 diabetes
Photo: attila dudas / Shutterstock.com
Presentations with alcohol-related serious injury to a major Sydney trauma hospital after 2014 changes to liquor laws
A number of recent studies have reviewed aspects of the complex questions associated with alcohol consumption, particularly with the misuse of alcohol.1–4 The impact of alcohol on emergency services has also been examined.5–10 It was found that drinking a single glass of wine doubled the risk of presentation to an emergency department; after three glasses, there was a 5-fold increase.11 The same study found that, after 10 standard drinks, the risk of needing to attend an emergency department was increased 10-fold for men and 14-fold for women.
There have been few well designed studies of alcohol-related injuries, and they often rely on emergency department data. Although of some value, such data have significant limitations if not collected prospectively and their acquisition appropriately resourced.12
On 24 February 2014, the New South Wales Government introduced changes to liquor regulations in the central district of the City of Sydney, the so-called “party precinct”. These legislative changes were enacted in response to community outrage after a series of adverse events reported in the media, particularly the deaths of two young men associated with alcohol-fuelled violence.
Many of the changes were based on successful strategies in the nearby Australian city of Newcastle, which had experienced similar alcohol-related serious injury problems.7,8 Some of the core changes are listed in Box 1. Several other, possibly key, initiatives were introduced in Sydney during the first year of the changed regulations. These included:
-
visibly increased police presence and monitoring;
-
introduction of identity document scanning on entry into some venues; and
-
sharing of information by venues to prevent intoxicated persons who have been refused entry at one site from gaining access to another.
In addition to the legislative changes, volunteer nocturnal patrols, usually under the auspices of non-government organisations, also commenced activities in the precinct.
Some of the initiatives were controversial in both the medical literature and the broader media.7–9,13 Our study was undertaken to assess the impact of these measures on alcohol-related serious injury, and also to determine the possible impact on emergency services in the relevant catchment area. Our study is timely in view of the review process currently being undertaken by the Australian Government on the impact of the lockout laws.14
Methods
To determine whether the strategy adopted to reduce alcohol-related injury in central Sydney has been successful, we undertook a 2-year retrospective analysis of alcohol-associated serious presentations to the emergency department of St Vincent’s Hospital, a major teaching hospital in the heart of the area where the changes were instituted. We analysed patient data stored on the hospital’s emergency department patient information computer system (EDIS).
Patient records for two periods were analysed: the 12 months preceding the introduction of the new alcohol laws (24 February 2013 – 23 February 2014; period 1) and the 12 months after their introduction (24 February 2014 – 23 February 2015; period 2). To avoid any bias, the researchers were blinded to which year was being analysed. One of the authors (G F) was assigned as the sole assessor who identified cases of alcohol-related serious injury.
Our search was restricted to persons with injuries classified under Australasian triage categories 1 and 2, as our attention was focused on the seriously or critically injured (Box 2). De-identified, routinely obtained demographic data included time and day of the week of the relevant injury. Other key data fields that were extracted and analysed were presenting symptoms and triage assessment.
In order to identify patients injured by serious assault, but also those suffering other serious injuries and major traumas associated with alcohol (such as vehicular and pedestrian injuries, or falls from a height), the presenting symptoms, triage assessment and diagnosis of all patients who presented as a result of serious trauma during the periods of analysis were examined for any reference to alcohol. All patients identified in this manner were included in this study.
The Fisher exact test was used to compare categorical outcome data, with statistical significance defined as P < 0.05. Confidence intervals (95%) for proportions were calculated with the standard assumption of normally distributed logarithms of the relative risk. There were no missing data for the analysed variables. Data analysis was performed with Stata 13 (StataCorp).
Ethics
Ethics approval was obtained for the study from the St Vincent’s Hospital Human Research Ethics Committee (ref. HREC/LNR/15/SVHA/62).
Results
During the 2-year study period, there were 13 110 Australasian triage category 1 and 2 presentations to the St Vincent’s Hospital emergency department: 6467 patients during period 1 and 6643 during period 2.
Of these presentations, 564 (4.3%) were identified as alcohol-related serious injuries: 318 during period 1 (4.9% of presentations during this period) and 246 during period 2 (3.7%). This decrease was statistically significant (P < 0.05), and occurred gradually during period 2 (Box 3).
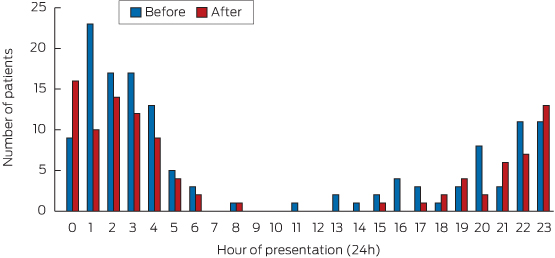
Given the nature of the problem, we examined the high alcohol time (HAT) separately; ie, the weekend, from 6 pm Friday to 6 am Sunday. The proportion of alcohol-related serious injury presentations in triage categories 1 and 2 was much higher during HAT (9.1%) than the rest of the week (3.1%; P < 0.05). There was a significant decrease in the total number of seriously injured patients during HAT after the introduction of the various control measures in 2014: from 140 presentations (10.4%) in the 12 months before the changes to 106 (7.8%) in period 2 (P < 0.05). This was a relative risk reduction of 24.8% (95% CI, 4.3%–40.9%).
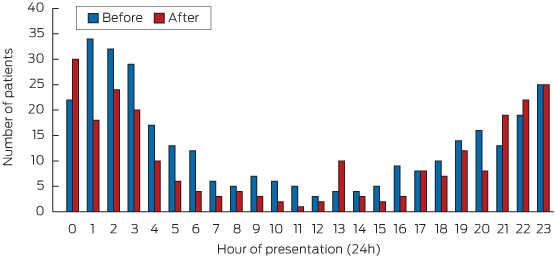
Analysis of the numbers of alcohol-related injuries by time of day found a consistent decrease in the number of presentations of seriously injured patients with alcohol-related injuries between 1 am and noon after the introduction of the new regulations. There was, however, a small increase in the number of patients presenting with alcohol-related injuries between 9 pm and midnight, as well as a small spike around 1 pm (Box 4).
These trends were even clearer when analysis was restricted to HAT (Box 5). During this time period, large reductions in serious injuries associated with alcohol-related violence were seen after 1 am.
Discussion
Our analysis has identified some significant positive results that followed the 2014 changes to the liquor laws and associated measures.
The clear decrease in serious injuries related to alcohol took some time to occur (Box 3); the gradual implementation of the policies may have led to a delayed decline in alcohol-related serious injuries. The small increase in alcohol-related injuries between 9 pm and midnight after the changes were introduced may have been related to increased alcohol intake earlier in the evening (“preloading”), before the times when the various bans take effect; the 1 pm spike may reflect lunchtime alcohol consumption.
The new measures were focused on curbing excessive drinking and violent behaviour after midnight, which could also explain some of our findings. Other indicators outside the scope of this study also support the success of the combined measures during their first 12 months of operation. Neurosurgeons at St Vincent’s Hospital reported a decrease in the numbers of patients presenting between 8 pm and 8 am with serious head injuries, which often require immediate surgery, from 26 patients during period 1 to 11 in the 12 months after the changes. Intensive care use also decreased; notably, there was not a single admission associated with alcohol-related violence during the first New Year’s Eve after the changes.16 The NSW Bureau of Crime Statistics reported a 32%–40% drop in assaults across the CBD Entertainment Precinct, and there was no increase in the number of assaults in neighbouring police command areas during the 12 months after the changes.17
There is significant controversy and discussion about which elements of the interventions may have been effective. Because of the non-specific nature of the data recorded, our study could not examine the effects of individual measures. The cost–benefit relationship of changes introduced to reduce alcohol-related serious harm has also been debated, as income, jobs and businesses have been lost as a result of the changes.4,10 This is especially relevant because the NSW Government is reported to be considering widening the regulations to include other geographical areas.
The precise costing of any reduction in the need for hospital care can be difficult,18 but the resources needed to treat critically ill, seriously injured patients, often after regular operating hours, and other associated costs are significant. The burden to both the patient and the community must be considered alongside the morbidity and mortality data.1,19
There are many limitations inherent to this and similar studies.8–10,13 Our methods cannot accurately capture complete data on the intake of alcohol. They rely on voluntary information provided by the patient and enquiries by health care workers; the information is recorded as free text in the EDIS system, without specific details about a number of relevant factors, such as the precise details of the reported injury or accident. The involvement of alcohol in trauma cases is almost certainly underestimated to a considerable extent, as blood alcohol testing may not be routinely undertaken in all unconscious or severely injured patients. Further, it was beyond the scope of our study to correct for potentially relevant demographic or ecological variables during the period of the study, such as population volumes.
Published research on acute alcohol harm relies heavily on information from emergency departments.5,11,20 This approach to data collection is not methodologically designed, and, being retrospective, is especially limited when trying to establish any causal relationships. In response to this, an Australia-wide research and data collection initiative has been established, and this collaboration between researchers, health organisations and the Australasian College of Emergency Medicine should facilitate a formal, more robust approach to data collection (personal communication, Associate Professor Peter G. Miller, School of Psychology, Deakin University, June 2015).
This study found a significant decrease in the number of patients presenting to a major trauma and teaching hospital with critical or seriously injuries related to alcohol use following the 2014 changes to regulations in the inner-city precinct of Sydney, Australia. The reduction was most marked in the period after midnight, which corresponds with the main thrust of the changed regulations.
Box 1 –
Key changes to alcohol laws for the Sydney CBD Entertainment Precinct, 2014
- All takeaway alcohol sales stop at 10 pm.
- No service of “shots” (alcoholic spirits) after midnight.
- 1.30 am–3.30 am “lockouts” at hotels, registered clubs, nightclubs and licensed karaoke bars. No entry for patrons, or re-entry for those who exit during the lockout period.
- 3.00 am “last drinks”. All alcohol service ceases.
CBD = central business district, central Sydney.
Box 2 –
Australasian triage categories relevant to serious or critical injuries15
|
|
|||||||||||||||
|
Category 1 |
Immediately life-threatening: conditions that are threats to life (or imminent risk of deterioration) and require immediate aggressive intervention. |
||||||||||||||
|
Category 2 |
Imminently life-threatening: condition is serious enough or deteriorating so rapidly that there is the potential of threat to life, or organ system failure, if not treated within 10 minutes of arrival in the emergency department; orImportant time-critical treatment: the potential for time-critical treatment (eg, thrombolysis, antidote) to make a significant effect on clinical outcome depends on treatment commencing within a few minutes of the patient’s arrival in the emergency department; orVery severe pain: humane practice mandates the relief of very severe pain or distress within 10 minutes. |
||||||||||||||
|
|
|||||||||||||||
Box 3 –
Alcohol-related serious injury presentations to the emergency department of St Vincent’s Hospital, Sydney, by calendar month, before and after changes to alcohol regulations.
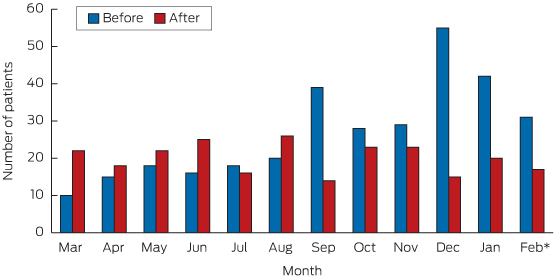
*February 2014: 26 cases to 23 February, 5 for 24–28 February; February 2015: cases until 23 February (study end).
Car technology can make zero road toll a reality: AMA President
Advances in car safety technology mean achieving a zero road toll is now within the nation’s grasp, AMA President Professor Brian Owler has told a road safety conference.
Urging government and consumers to demand that the latest life-saving equipment be fitted as standard to all new cars, Professor Owler told the Australasian Road Safety Conference on the Gold Coast that although motorists needed to drive with greater care, the widespread adoption of proven technologies that improved car safety and mitigated human error was “the future of road safety”.
“It is the game changer that mitigates our human faults,” he said. “It is the tool we have to truly move towards zero fatalities and serious injuries on our roads.”
Earlier this year the AMA and the Australian New Car Assessment Program (ANCAP) jointly called for autonomous emergency braking (AEB) – in which the brakes are automatically applied if the driver fails to take action to avoid an impending collision – to be fitted to all new cars.
Evidence indicates the technology cuts the incidence of rear-end collisions by more than 38 per cent.
Professor Owler, who is the public face of New South Wales’ successful Don’t Rush road safety campaign, told the Conference that developing safer cars did not lessen the need to improve driver behaviour.
He took particular aim at what he saw as societal acceptance of risky behaviour on the roads.
“There are cultural issues, and even rites of passage, that make some young people think that speeding and disobeying the road rules is something tough, something cool or something to be admired.
“There are no survivors of road trauma who think this way.”
The AMA President said compulsory seatbelt and drink-driving laws, complemented by education and awareness campaigns, had shown that modifying driver behaviour was possible, though the process was lengthy and difficult.
And, he added, improving driver behaviour and choices did not eliminate the capacity for human error, which contributed to 90 per cent of crashes.
Professor Owler said people should not die, or endure life-long pain and impairment, because of a split-second mistake, which was why there should be widespread adoption of proven life-saving technology in cars.
Car companies are fitting AEB as standard equipment in Europe, the United States and Japan, and the AMA President said there was no reason why Australia should be left behind.
There have been objections that making AEB mandatory will increase the cost of new cars – industry estimates an additional cost of up to $200 per vehicle.
But Professor Owler said this was little price to pay for technology that would save lives, and asked why Australian life should be valued any less than one in Europe or North America.
“Australians,” he declared, “should be driving the safest vehicles on our roads”.
Related: MJA – Open speeds on Northern Territory roads: not so fast
ANCAP aims to pressure car companies to fit AEB in Australia vehicles by making it impossible from 2018 for a car to get a five-star crash rating without the technology.
Professor Owler said consumers needed to exert similar pressure.
“The fastest way to have vehicles with these features as standard is through consumer demand,” he said, urging large fleet purchasers in particular to demand advanced life-saving equipment as standard in their vehicles.
The AMA President said it was not good enough to aim simply at reducing road fatalities and injuries.
Advances in technology meant the elimination of road trauma was a practical goal.
“There is no acceptable number of deaths, as there is no acceptable number of serious injuries,” he said. “Towards zero is not an aspirational target. For Australia, we must make zero the reality. We have the ability to do this.”
Adrian Rollins
Latest news:
•The 12 mental health indicators we should be focusing on
•MBS Review a quick and nasty cost-cutting exercise
•Troponin test concerns
Signs workforce planning getting back on track
It’s been a chequered time for medical workforce planning in recent years.
Health Workforce Australia (HWA) was a Commonwealth statutory authority established in 2009 to deliver a national and co-ordinated approach to health workforce planning, and had started to make substantial progress toward improving medical workforce planning and coordination. It had delivered two national medical workforce reports and formed the National Medical Training Advisory Network (NMTAN) to enable a nationally coordinated medical training system.
Regrettably, before it could realise its full potential, the Government axed HWA in the 2014-15 Budget, and its functions were moved to the Health Department. This was a short-sighted decision, and it is taking time to rebuild the workforce planning capacity that was lost.
NMTAN is now the Commonwealth’s main medical workforce training advisory body, and is focusing on planning and coordination.
It includes representatives from the main stakeholder groups in medical education, training and employment. Dr Danika Thiemt, Chair of the AMA Council of Doctors in Training, sits with me as the AMA representatives on the network.
Our most recent meeting was late last month, and the discussions there make us hopeful that NMTAN is finally in a position where it can significantly lift its output, contribution and value to medical workforce planning.
In its final report, Australia’s Future Health Workforce, HWA confirmed that Australia has enough medical school places.
Instead, it recommended the focus turn to improving the capacity and distribution of the medical workforce − and encouraging future medical graduates to train in the specialties and locations where they will be needed to meet future community demands for health care.
The AMA supports this approach, but it will require robust modelling.
NMTAN is currently updating HWA modelling on the psychiatry, anaesthetic and general practice workforces. We understand that the psychiatry workforce report will be released soon. This will be an important milestone given what has gone before.
Nonetheless, it will be important to lift the number of specialties modelled significantly now that we have the basic approach in place, so that we will have timely data on imbalances across the full spectrum of specialties.
The AMA Medical Workforce Committee recently considered what NMTAN’s modelling priorities should be for 2016.
Based on its first-hand knowledge of the specialities at risk of workforce shortage and oversupply, the committee identified the following specialty areas as priorities: emergency medicine; intensive care medicine; general medicine; obstetrics and gynaecology; paediatrics; pathology and general surgery.
NMTAN is also developing some factsheets on supply and demand in each of the specialities – some of which now available from the Department of Health’s website (http://www.health.gov.au/internet/main/publishing.nsf/Content/nmtan_subc…). I encourage you to take a look.
These have the potential to give future medical graduates some of the career information they will need to choose a specialty with some assurance that there will be positions for them when they finish their training.
Australia needs to get its medical workforce planning back on track.
Let’s hope that NMTAN and the Department of Health are up to the task.
Medicare review taken off course
The AMA has demanded the Federal Government recast its approach to the Medicare Benefits Schedule Review as medical researchers have distanced themselves from claims doctors are routinely ordering ineffective and potentially harmful tests and procedures that are costing the nation cost the nation hundreds of millions of dollars each year.
The AMA has reasserted its support for the Medicare Benefits Schedule Review (and the accompanying Primary Health Care Review) as long as it not only about removing outdated services and procedures, but replacing them with items that reflect modern practice.
AMA President Professor Brian Owler told The Australian Financial Review the medical profession backed efforts to update the MBS but “we’re not going to have a Review that takes money away and puts it on the bottom line of the Budget, and the [Health] Minister [Sussan Ley] says that’s where it’s going. It takes services away from patients.”
The blame game
There has been mounting disquiet over the Government’s handling of the Review, including the depth of consultation with clinician representatives and claims that the vast majority of items were not backed by evidence, and around 30 per cent of all care was of little worth.
Fears about the direction the Government was taking were crystallised on 27 September when Ms Ley launched public consultations by arguing that only a tiny fraction of the 5769 items on the MBS had been assessed for effectiveness and safety, and “inefficient and unsafe Medicare services…cost the nation dearly”.
Issuing the call for consumers to participate in the Review, Ms Ley said that, “30 per cent of expenditure is not necessary, wasteful, sometimes even harmful for patients”.
Professor Owler said the claim was not only “factually incorrect”, but was being used by the Government and the Review Taskforce Chair Professor Bruce Robinson to try and frame the discussion around the idea that there were massive savings to be made because doctors were milking the system.
The AMA President said the figure had been uncritically imported form the United States and there had been no evidence to support it in the Australian setting.
Instead, he said, the Government’s real intention was to use the Review to make Budget savings.
“They need to be upfront about what this process is and that it’s a budget preparation measure,” he told the AFR. “We’re having this conversation and it’s ‘No, no, this is not a cost saving exercise’. But, ‘Yes, the cost savings are going to the bottom line of the budget’. They say ‘Yes, we will reinvest’, but it’s going to be a very protracted, drawn out process to get any money back into MBS.”
Follow the evidence
A day after the Government launched the consultation process, ABC television’s Four Corners program aired claims that doctors were ordering tests and performing procedures that were of little or no benefit for patients and cost the nation hundreds of millions of dollars each year, including scans for lower back pain, spinal fusion surgery, knee arthroscopies and inserting stents in patients with stable angina.
Ms Ley seized on the program, which she said had exposed “real – not perceived – waste in health spending”, and demonstrated the need for the MBS Review.
The Minister said medical specialists and health researchers appearing on the program had “put their professional reputations on the line to provide important insight into billions of dollars being spent on unnecessary, outdated, inefficient and even potentially harmful procedures”.
But two researchers whose work was drawn on in the Four Corners program to help substantiate claims that doctors used inappropriate and unnecessary tests and procedures said their data had been misinterpreted and taken out of context.
Writing in Medical Observer, Associate Professor Helena Britt and Associate Professor Graeme Miller said that although their research showed GPs ordered imaging in about 25 per cent of new cases of low back pain, “conversely, we could equally state that 75 per cent of new cases were not sent for imaging”.
The researchers said that while they did conclude that the rate of imaging for back problems at the initial encounter was inconsistent with guidelines, this was only the case if there were no ‘red flag’ issues present, such as significant trauma, fever, weight loss, inflammatory conditions or advanced age.
“Unfortunately,” they said, “we cannot identify whether or not patients referred for imaging for back symptoms had any of these red flags, but the guidelines suggest that zero imaging for all cases would not represent best quality care.”
Ms Ley rejected claims the Government had launched an attack on the medical profession, and asserted that 97 per cent of MBS items had never been assessed for their clinical effectiveness or safety.
But Professor Owler said the Minister’s claim was “quite misleading”.
While just 3 per cent of items had been assessed through the Medical Services Advisory Committee process, the AMA President said, “but that doesn’t mean that there’s not evidence behind all of the other things that we do”.
He questioned the need for evidence-based reviews for performing life-saving operations: “I don’t need an evidence-based review to say that I should remove the tumour from a child that presents through the emergency department because I know they’re going to end up dead within the week if I don’t do it.”
“There are some things that, yes, we need to evidence-based review, but there are many on the schedule that don’t, and saying that 97 per cent doesn’t have evidence is quite misleading.”
MBS reviews nothing new
He said the medical profession had to be “vigilant” about the narrative being used to shape debate about the Review.
Professor Owler said the AMA not only supported the MBS reviews, but had been engaged with successive governments in undertaking them since 1990. He said in the last five years alone, the AMA had participated in reviews covering 26 areas of the MBS.
“Can we save money? Yes, and the AMA’s more than happy to engage in that process, but let’s actually go through and do the reviews and come up with the evidence before we actually pre-empt what the outcome is and what procedures might have conditions or be removed from the Schedule,” he said.
“The risks to patient care from an emasculated MBS are too great to allow this Review to go off the rails.”
Adrian Rollins
Warm temperatures put heat on ED
Heat-related emergency department visits and deaths surge when the mercury rises above 23 degrees Celsius, according to a US study.
Researchers at Brown University and the Rhode Island Department of Health undertook a detailed statistical analysis of emergency department visits, deaths and weather data, and included possibly confounding factors, such as ozone, to assess the effect of rising temperatures on presentations at hospitals. The ED records included information about whether doctors thought a patient’s condition was related to heat or dehydration.
The study suggested that if the population were living with the sort of temperatures the world is expected to reach because of climate change, there will be an appreciable increase in emergency department visits and deaths.
Lead author Samantha Kingsley said the primary finding was that as temperatures increase, the number of emergency room visits and deaths increase. But, she said, people were going to the hospital for heat-related reasons at temperatures below what would typically be considered extreme.
The researchers found that while the rate of heat-related ED visits jumped 3.3 per cent on days when the temperature reached 23 degrees compared with those with a high of 18 degrees, they jumped almost 24 per cent when the mercury reached 29 degrees compared with days when the high was 23 degrees. Overall, temperature began to play an independent role in increasing ED visits when the mercury reached or exceeded around 23 degrees.
Senior author and Associate Professor Gregory Wellenius said that people should be aware that heat represents a significant public health threat that needed to be taken seriously, even when authorities did not issue heat warnings.
Interestingly, the researchers found that 18 to 64 year olds made the most heat-related emergency department visits, rather than infants and the elderly, who are considered to be the most vulnerable to heat-related health problems. The researchers were unsure about the reason, but speculated it may be because people in this age group were more likely to be outdoors working or playing sport, and may pay less heed to heat warnings.
Previous studies have linked higher temperatures to increased hospital visits and deaths, but in heat waves the elderly have been most at risk. Earlier this year a heat wave killed about 2000 people in India, many of whom were elderly.
The researchers warned that their finding that ED visits and deaths are greater on warmer days, even if temperatures are only in the 20s, suggests that distress from the heat may become even more common as temperatures rise as a result of global warming.
Kirsty Waterford
[Series] Perforated peptic ulcer
Perforated peptic ulcer is a common emergency condition worldwide, with associated mortality rates of up to 30%. A scarcity of high-quality studies about the condition limits the knowledge base for clinical decision making, but a few published randomised trials are available. Although Helicobacter pylori and use of non-steroidal anti-inflammatory drugs are common causes, demographic differences in age, sex, perforation location, and underlying causes exist between countries, and mortality rates also vary.

 more_vert
more_vert