Health, as befits one of the major functions of Government, is shaping as a key battleground in the 2016 Federal Election.
In its first term in office, the Coalition Government has left no area of health policy untouched. Medicare rebates have been frozen, there is a thoroughgoing review of 5700 MBS items underway, Medicare Locals have been replaced by Primary Health Networks, Health Care Homes and the My Health Record are being trialled, national agreements on public hospital funding were abandoned as part of plans to renegotiate the Federation, and the role of the private sector, especially health insurers, in providing health services is being examined.
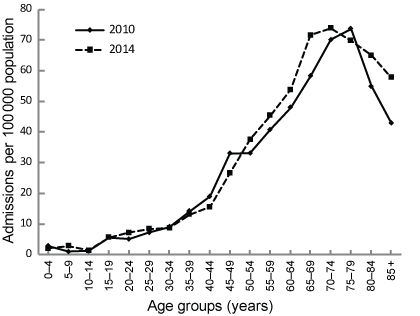
These changes have come against the backdrop of steadily increasing demand for health services. Advances in health care and medicine have meant that Australians are living longer than ever, and as lives extend, the number of patients living with multiple chronic health conditions has risen. Caring for these patients is imposing ever-increasing demands on GPs, specialists and hospitals.
Coincidentally, advances in medical science are delivering new and more effective treatments that are saving and improving lives – but often at a hefty cost.
In this Australian Medicine special, each of Health Minister Sussan Ley, Shadow Health Minister Catherine King, and Australian Greens leader Senator Richard Di Natale lays out their broad vision for health policy.
These should be seen as their first, rather than final, word on health during this Federal Election, and Australian Medicine will provide comprehensive coverage of the detailed policy pronouncements as they are made during the course of one of the longest campaigns in Australia’s recent political history.

Health Minister Sussan Ley
Building a 21st century health system for all Australians
The health policy directions we have outlined in the recent Federal Budget are underpinned by a key and very important objective; to ensure patients and consumers are at the centre of all our decision making.
Ultimately, we are all here to ensure patients have a better health outcome, and this can only be achieved by working together to make sure our service delivery is well-integrated, efficient and focused.
It is well documented that the Commonwealth needs to spend its health dollar wisely, landing that funding as close to patients as possible.
Simply throwing more money at the system is tantamount to ‘placebo policy’: it may make some feel better but it won’t treat the cause.
In the last 12 months, through the Council of Australian Governments, (COAG), every State and Territory has had significant input into what the primary and health care sector needs to look like in coming years.
Central to these discussions is our desire to reduce the barrier patients face across a fragmented system, with an aim of keeping people well at home and, where possible, out of hospital.
Since becoming Health Minister, I have consulted widely with many of you on the ground, and we are now undertaking important reforms like Health Care Homes, not only because it is the right policy but as a show faith for your co-operation and support in this process.
Health Care Homes will trial a new way of funding chronic and complex care, which will ensure patients receive integrated, coordinated care to better meet their needs.
It’s important to note in addition to the $21 million already committed to complete trials over two years, bundled payment models during this period will be funded as certain Chronic Disease Management MBS items and cashed out to support this initiative.
Moving closer to a national rollout, we will obviously assess what further funds may be required in consultation with you and your representatives.
There are a number of other integrated reforms that we are undertaking to help build a Healthier Medicare and put patients first.
Our clinician-led review of all 5700 items on the MBS is also progressing steadily, under the careful consideration and advice of your peers.
At the most recent COAG, it was agreed an additional $2.9 billion in Commonwealth investment for public hospitals was required for ongoing needs, but with a greater focus on patient outcomes, quality and safety, particularly for those being treated for a chronic illness.
All children and concession card holders will now be eligible for affordable access to dental care through a new national public dental scheme, which will see the Commonwealth double its contribution towards frontline public dental services from July this year.
Australians with mental health issues will also begin receiving the integrated care they need from 1 July, as we begin trialing new once-a-new generation reforms providing patients with personalised care packages.
Our world-class Pharmaceutical Benefits Scheme gives Australians access to affordable medicines, with the Government’s reforms saving patients as much as $20 per script on common everyday medicines, with further price cuts to come.
We’ve also ensured savings to taxpayers are being reinvested in new innovative medicines, with the Turnbull Government making nearly 1000 listings on the PBS over the past three years – triple that of the previous Government.
This includes our watershed commitment of over $1 billion to eradicate hepatitis C within a generation.
This is being supported by new reforms announced in the Budget, allowing patients to get faster access to life-saving medicines and medical devices up to two years earlier, by breaking down international trade barriers and red tape.
We are actively working to protect and increase immunisation rates against deadly and debilitating viruses, with incentives for GPs to catch up overdue children, a national all-age vaccination register and ‘no-jab, no pay’ deterrents.
Also, with an eye to the future, we want patients to find it easier to navigate the health system through the digital ‘My Health Record’, which will allow everything from a patient storing prescription information, through to doctors having life-saving access to someone’s allergies in a medical emergency.
There are many more initiatives, and I encourage you to visit www.health.gov.au to find out more at
Can I take this opportunity to acknowledge your outgoing AMA President, Professor Brian Owler. While we have not always arrived at the same position in relation to health policy, I acknowledge his fierce advocacy on behalf of the AMA and its members.
I look forward to a collegial working relationship with his forthcoming successor and hope we can work together to develop policies which ensure every dollar ‘works’ in a constrained budgetary environment.
The Turnbull Government also appreciates the efforts of many GPs to keep costs down during the current Medicare rebate indexation pause, which was first introduced under the previous Government back in 2013-14.
I would like to reaffirm my commitment to the possibility of a review of this pause as further improvements and inefficiencies are identified through our Healthier Medicare reforms.
In closing, be assured across all areas of the health sector I continue to have an open ear, open door approach, and welcome constructive dialogue in balancing our joint desire to maintain and build a progressive health system for all Australians.
My email is Minister.Ley@health.gov.au if you would ever like to raise any ideas or questions.

Shadow Health Minister Catherine King
General practice is the heart of Medicare and deserves respect
One of the most disappointing aspects of Malcolm Turnbull’s election manifesto is its continuing attack on primary care.
After being devalued in the Coalition’s first two Budgets by the GP Tax and then the four year freeze, the profession could have been forgiven for hoping a change of leader marked a change in approach to general practice.
Sadly, as we now know, this was not the case, and the shock decision to extend the freeze out to six years effectively signals that under the Coalition, Medicare rebates are now effectively locked at their current rates.
The signal this sends is that the Coalition does not value general practice, and does not believe the services rendered by GPs are worth being properly renumerated for.
I can give you an assurance that Labor most emphatically does not share this view, and a Shorten Labor Government will place general practice at the forefront of Australia’s healthcare system.
By the time voters go to the polls, our health policy will leave the profession and their patients in no doubt about the contrast between Labor’s respect for general practice, and the Coalition’s approach of the last three years.
That is because Labor believes general practice is the heart of Medicare, acting as the first line of preventive health care, catching and managing illness and disease before far worse outcomes lead to greater costs for both patients and the health system.
Indeed, all of the evidence internationally is that the stronger a country’s primary health care system, the better its health outcomes are.
We know from a number of studies that “health systems with strong primary health care are more efficient, have lower rates of hospitalisation, fewer health inequalities and better health outcomes including lower mortality, than those that do not”.
That is why, when last in Government, Labor did introduce a number of measures to improve general practice, including continuing incentives that improved access and increased bulk billing rates; being properly renumerated for the treatment of chronic disease; provided incentive payments for the treatment of practice nurses and a number of other measures.
But as we look to the future of general practice, we are also conscious of the way Medicare has evolved over more than 30 years now.
No serious health expert disputes the need for Australia’s health system to better manage patients with chronic conditions, and Labor welcomes the proposals of the Primary Health Care Advisory Group to better manage the care of the one-in-five Australians living with two or more chronic health conditions.
Last year’s OECD Health Care Quality Review warned Australia’s ageing population will lead to a growing burden of chronic disease, and highlighted the need for greater investment in primary care to tackle the rise in chronic disease.
But unlike the current Government, a Shorten Labor Government will pay more than lip service to general practice being central to care coordination, as will be made clear in our primary care policy.
Labor understands these reforms can only be achieved in co-operation with doctors, and that co-operation can never succeed if the profession is constantly blindsided by Budget night surprise raids and politically inspired attacks on the integrity of doctors.
I know doctors want to be a major part of the solution.
So too does Labor, and if Labor is elected to Government I can assure you we would want to be advised by you as GPs about what the best system should look like, and how patients can best be looked after.

Australian Greens leader Dr Richard Di Natale
Investing in health care
The Greens believe good health care is an investment, not a cost. As a wealthy country we are lucky to have the opportunity and the means to make high-quality healthcare available to everyone.
Of course we should always seek to ensure we get the best value for our money, but as effective new treatments become available we believe securing affordable, universal access should be the objective.
Spending that leads to better health outcomes and longer lives represents good value for money, and should be prioritised. Australia’s health spending is not unusual by comparable global standards. Among OECD countries, the average spend on health is about 9 per cent of gross domestic product – not much different from where Australia sits now. By contrast, the European average is greater than 11 per cent, and the United States spends 17.1 per cent of GDP on health in a system that delivers worse outcomes.
And yet under this Government, which sees health merely as a cost to the bottom line, the harsh cuts continue. This year’s Budget has seen the Government extend the freeze on indexation of the MBS. This is a co-payment by stealth, which we recognise will force doctors to make a difficult choice about passing on the costs to patients, knowing that hitting patients will almost certainly lead to avoidable and costly presentations to hospital in some cases.
Deeper cuts to the Flexible Funds, with still no certainty about where the axe will fall, is leaving providers of essential services vulnerable and patients at risk.
There is so much to do to extend true universal access to all, including in particular to Aboriginal and Torres Strait Islander Australians whose health outcomes continue to lag behind the rest of the nation. We need secure, targeted investment, not cutbacks, and it was a huge disappointment to see the Government commit no funding at all for the Implementation Plan of the National Aboriginal and Torres Strait Islander Health Plan in this year’s Budget.
The Greens believe in a system which meets the challenges of changing demographics and rising chronic disease. It is time for a real plan for the future of our primary care system, which puts patients at the centre of their care, with continuity of care and appropriate funding. The Government’s Healthcare Homes plan risks this important reform by under-resourcing the trial.
The Greens have long championed the Denticare scheme, believing that the mouth should be treated like any other part of the body in terms of access to the health system. We continue support its expansion, seeking universal dental care for all Australians over time.
Spending more on health care is not unsustainable – it is a matter of priorities, and the Greens choose to prioritise good health care.
The Greens are committed to maintaining a health care system that is publicly funded, of the highest quality, and available to all. We want Australians to have access to the latest drugs and treatments that medical science has to offer. All Australians, no matter where they live, should share equally in the benefits of our health system.
The Greens will be announcing a suite of fully costed health policies throughout the election campaign, setting out our vision for the health system in Australia. We encourage AMA members to watch out for our announcements – which will provide a positive, equitable plan for the future.

 more_vert
more_vert