A gender imbalance has been noted at medical conferences internationally, with typically more male than female speakers.1–3
We conducted a retrospective observational study to assess the proportion of female program speakers and the time allocated to them at the annual scientific meetings (ASMs) of six Australasian specialty colleges from 2012 to 2014 (n = 17). For 2013, female ASM representation was compared with published data on female workforce participation for each specialty.4 The six colleges evaluated were the Australasian College for Emergency Medicine (ACEM), Australian and New Zealand College of Anaesthetists (ANZCA), College of Intensive Care Medicine of Australia and New Zealand (CICM), Royal Australasian College of Physicians (RACP), Royal Australasian College of Surgeons (RACS) and Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG).
We audited official ASM programs and included all sessions with allocated speaking times. We compared distributed data using the Mann–Whitney U test and categorical variables using a χ2 test. A two-sided P < 0.05 was taken to indicate statistical significance.
The proportion of male speakers exceeded the proportion of female speakers at every conference (Box). The proportion of female speakers ranged from 8% (3/37) at CICM 2012 to 42% (39/93) at RANZCOG 2012. At seven of the 17 ASMs (all RACS ASMs, CICM 2012 and 2014, ANZCA 2012 and RANZCOG 2013), the median time allocated per speaker was significantly higher for male than female speakers. At the other ten conferences, there was no statistically significant difference.
In 2013, for all colleges except RACS, the proportion of female speakers was lower than the proportion of female doctors in the corresponding specialty workforce; however, this did not reach statistical significance. In contrast, the proportion of female speakers at RACS 2013 exceeded the proportion of women in the surgical workforce (P < 0.001).
Our results indicate that the gender imbalance among college ASM speakers largely reflects gender representation in the specialty workforce.
The longer median speaking time for male speakers may reflect the greater proportion of men at senior levels in the specialty workforce. As ASM programs did not always distinguish between invited speakers and those selected from abstract submissions, we could not compare these selection pathways. A limitation of the workforce comparison is that each specialty workforce includes practitioners who do not undertake research and are unlikely to speak at conferences; conversely, ASM speakers are not exclusively drawn from the specialty workforce.
Our findings raise an important question — should the proportion of female speakers at conferences reflect their representation within the college membership? Or should conference organisers be striving for greater female representation? Improving the balance of male and female speakers at conferences may improve workforce gender balance by encouraging women to pursue research and advancing the careers of female speakers. Colleges represent themselves to the medical community through their ASM programming choices. Efforts to improve gender balance in the medical community should therefore include consideration of speakers at medical conferences.
Box –
Proportion of annual scientific meeting (ASM) speakers, by gender
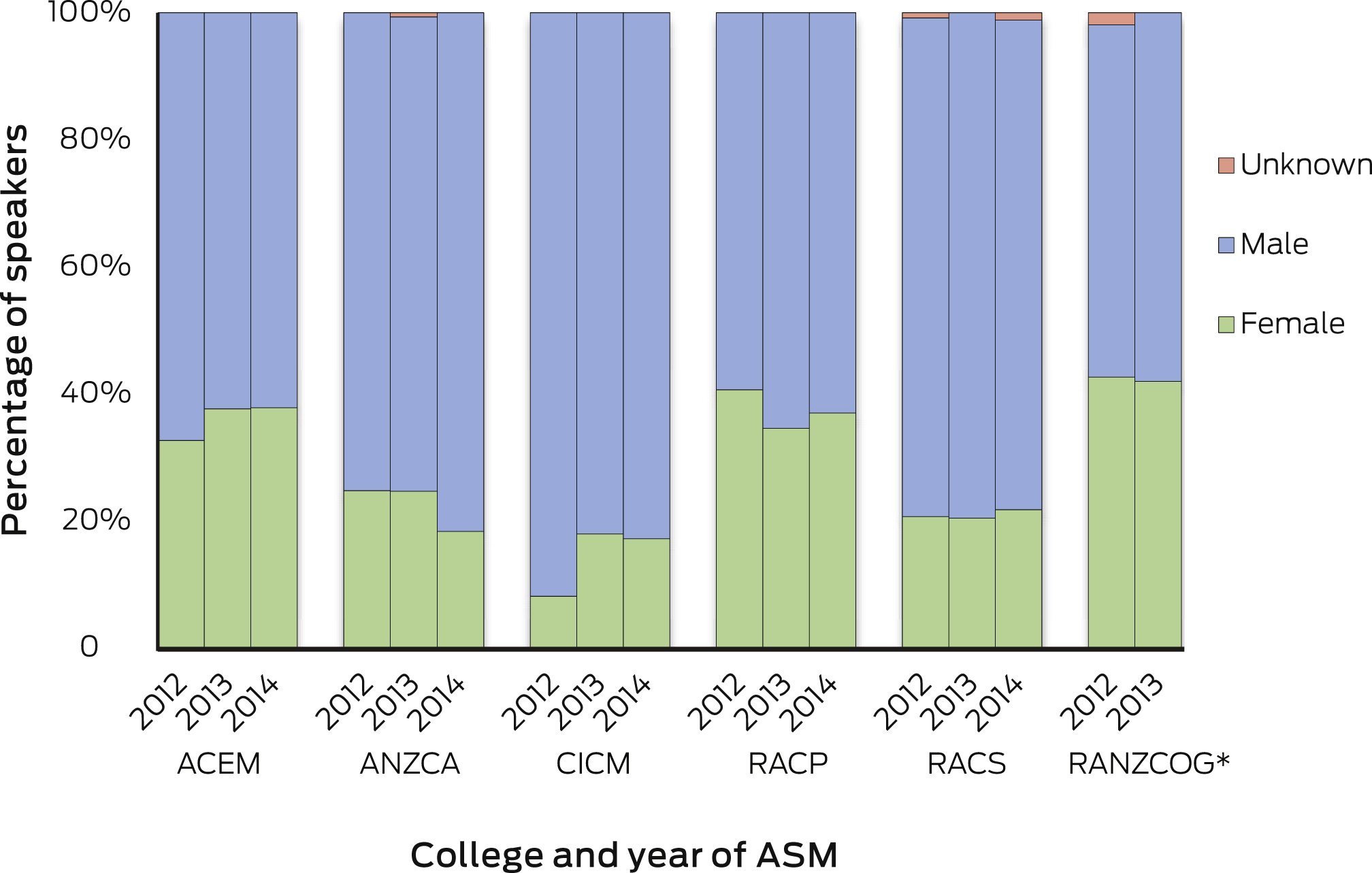
ACEM = Australasian College for Emergency Medicine. ANZCA = Australian and New Zealand College of Anaesthetists. CICM = College of Intensive Care Medicine of Australia and New Zealand. RACP = Royal Australasian College of Physicians. RACS = Royal Australasian College of Surgeons. RANZCOG = Royal Australian and New Zealand College of Obstetricians and Gynaecologists. * RANZCOG did not hold an ASM in 2014.

 more_vert
more_vert