The use of comprehensive and meaningful summary metrics to track the performance of health systems worldwide in achieving universal health coverage, including access to high-quality health care, is ongoing.1–3 At least two summary metrics are available: the service coverage index, which includes a set of 14 essential health services,1 and the Healthcare Access and Quality (HAQ) Index, which focuses on amenable premature mortality of 32 causes of death (ie, death from causes that should not be fatal in the presence of effective medical care).
Preference: Administration and Health Services
2
[The Lancet Commissions] The Tsinghua–Lancet Commission on Healthy Cities in China: unlocking the power of cities for a healthy China
Over the past four decades, rapid urbanisation in China has brought unprecedented health benefits to its urban population, but has also created new challenges for protection of and promotion of health in cities. With the shift from rural to urban living, more people than ever enjoy the health advantages that cities can provide, such as better access to health services and improved sanitation. For example, the average life expectancy of male urban residents in 2010 was estimated to be 7·09 years longer than that of of their counterparts in rural China; urban females lived 6·64 years longer.
Excellent choice for Excellence in Healthcare Award
The recipient of the AMA Excellence in Healthcare Award 2018 wants to know how she can use it to build greater awareness for a very worthy cause.
Professor Elizabeth Elliott AM FAHMS was presented with her award by outgoing AMA President, Dr Michael Gannon, at the AMA National Conference in Canberra in May.
Professor Elliott is a pioneer in research, clinical care, and advocacy for Fetal Alcohol Spectrum Disorder (FASD) and was named the winner of the AMA Excellence in Healthcare Award 2018 during the opening session of the Conference.
FASD is caused by prenatal alcohol exposure and is recognised as the leading preventable cause of prenatal brain injury, birth defects, and developmental and learning disability worldwide. There are lifelong consequences for children born from alcohol-exposed pregnancies.
The AMA Excellence in Healthcare Award is for an individual, not necessarily a doctor or AMA member, who has made a significant contribution to improving health or health care in Australia. The person may be involved in health awareness, health policy, or health delivery.
Professor Elliott was nominated for the award by the National Organisation for Fetal Alcohol Spectrum Disorder (NOFASD), the first and largest organisation dedicated to FASD in Australia.
Over the past 20 years, FASD has evolved from being a little-known, poorly recognised, and misunderstood condition to becoming a major strategic focus for Commonwealth and State Health Departments.
“I am really delighted to be acknowledged, but I really accept the award on behalf of all the children and families I work with, and of course a lot of dedicated clinicians,” she told Australian Medicine.
“I guess for me it’s particularly nice that the group that nominated me was the national organisation.
“I read something that said this was an opportunity to highlight this cause so I’m very keen to find out how to use the AMA network to raise awareness.
“We need to raise awareness of (1) the fact that are still lots of women who drink during their pregnancy not knowing they might harm their unborn child, and (2) there are lots of doctors who are very reluctant to ask pregnant mothers about their drinking.
“They don’t want to upset the doctor-patient relationship, and yet women tell us they want to be asked. They want clear advice. In fact many of them tell us they want to be told not to drink during pregnancy. They want a clear message from doctors.”
Professor Elliott is a Distinguished Professor in Paediatrics and Health at The University of Sydney School of Medicine and a NHMRC Practitioner Fellow. She has been a passionate advocate for raising awareness of FASD for more than 20 years.
In presenting her the award, Dr Gannon said Professor Elliott played a significant leadership role in developing the Australian Guide to the Diagnosis of FASD and online training modules, new clinical services, a national FASD website, and a national FASD register.
“She chaired the Australian Government’s National FASD Technical Network and is Co-Chair of the NHMRC Centre of Research Excellence in FASD, and Head of the NSW FASD Assessment service,” Dr Gannon said.
“She was lead clinician in the Lililwan study on FASD prevalence in the Fitzroy Valley and has published extensively on FASD.
“She contributed to WHO, NHMRC, and RACP alcohol guidelines and has been a keynote, invited, or scientific presenter at more than 300 conferences nationally and internationally.
“Professor Elliott is a true pioneer in the FASD field and has contributed to the development of Australia’s response to FASD, through addressing aspects of health policy, health care delivery, education, and health awareness in the work she has undertaken.
“However, FASD is only one component of Professor Elliott’s work, which includes disadvantaged children in Immigration detention, with rare disorders, and living in remote Australia.
“In 2008, she was made a Member of the Order of Australia (AM) for services to paediatrics and child health and, in 2017, she received the Howard Williams Medal from the Royal Australasian College of Physicians (RACP) – its highest award – for her contribution to paediatrics in Australia and New Zealand.
“Much of her work has been undertaken voluntarily, and has strengthened Australia’s health systems and their capacity to respond to FASD.
“Her efforts have improved health care services in FASD and changed health outcomes for children and families living with, and affected by, FASD.
“She is a worthy recipient of the AMA Excellence in Healthcare Award.”
CHRIS JOHNSON
War zone gynaecologist named AMA Woman in Medicine
AMA Woman in Medicine 2018, Professor Judith Goh AO, has described receiving her award as a great honour and privilege.
Adding that it was acknowledgement for the work of a dedicated team of health professionals, Professor Goh told Australian Medicine the award would also help build awareness for the plight of women’s health.
“We often live quite comfortably in Australia but for most women around the world, surviving their pregnancy is not taken for granted,” she said.
“So this is great recognition. But we don’t do these things to be recognised. We do it because we want to do it.”
Professor Goh is a dedicated gynaecologist who volunteers her time treating women in war zones and Third World countries.
She was named the AMA Woman in Medicine 2018 at the AMA National Conference in May.
She is a urogynaecologist who has devoted her career to women’s health. Her next stops are Bangladesh, Myanmar, and some African countries.
A world-renowned surgeon who has spent approximately three months every year for the past 23 years training doctors in Third World countries in repairing vesico-vaginal fistula – a devastating injury that can occur following prolonged, obstructive labour – Professor Goh was noticeably touched by the honour.
In presenting her the award, outgoing AMA President Dr Michael Gannon noted that Professor Goh’s nominators – colleagues from the Australian Federation of Medical Women and the Queensland Medical Women’s Society – have described her career as both humbling and inspirational.
“Since 1995, Professor Goh has donated her time and expertise, working abroad several times a year as a volunteer fistula surgeon in many parts of Africa and Asia, including Bangladesh, Sierra Leone, Ethiopia, Tanzania, Uganda, the Democratic Republic of Congo, and Liberia,” Dr Gannon said.
“Professor Goh runs the twin projects, Medical Training in Africa and Medical Training in Asia, via the charity, Health and Development Aid Abroad (HADA), using funds raised to help pay for women’s surgeries such as the correction of genital tract fistulae and prolapse, while training the local staff in these areas.
“To carry out her work within a dedicated team of professionals, Professor Goh often has to brave political unrest, and perform surgery in challenging environments, as well as deal with the emotional and social injuries to her patients due to war, rape, domestic violence, poverty, shame, and grief.
“Her work has changed lives for the better for hundreds of affected women, correcting their often long-standing and preventable obstetric trauma, including vesico-vaginal and recto-vaginal fistulae, with the minimum of overhead costs to maximise the reach of her services.
“Professor Goh uses her time abroad to upskill local practitioners in this area of medicine, and to raise awareness of the underlying causes of chronic complications of birth trauma, including poverty, lack of education, lack of awareness, and the subordination of women in some cultures.
“In 2012, she was made an Officer of the Order of Australia (AO) ‘for distinguished service to gynaecological medicine, particularly in the area of fistula surgery, and to the promotion of the rights of women and children in developing countries’.
“Her humble dedication within this field of women’s medicine, and her brave and generous service to women all over the world, is inspirational, and very worthy of recognition as a recipient of the AMA Woman in Medicine Award.”
Professor Goh said many women felt ashamed after delivering stillborn babies.
“In some places it is seen as a failure. There is even violence against them in some communities. We are building a community where lot of women can come together and feel supported,” she said.
“In our country we no longer really say ‘mother and child are well’ after a baby is born. It’s taken for granted, so the first question is how much did the baby weigh.
“But there are so many places in the world where this cannot be taken for granted.”
The AMA Woman in Medicine Award is presented to a woman who has made a major contribution to the medical profession by showing ongoing commitment to quality care, or through her contribution to medical research, public health projects, or improving the availability and accessibility of medical education and medical training for women.
CHRIS JOHNSON
WHO public health awards for Western Pacific Region
Public health champions from the World Health Organization (WHO) Western Pacific Region were recognised at the 71st World Health Assembly in Geneva, Switzerland.
Dr Nazni Wasi Ahmad from Malaysia received honours for her innovative research using insects to treat people with diabetes, and the Korea Institute of Drug Safety and Risk Management (KIDS) for contributions to drug safety in the country.
“Dr Nazni Wasi Ahmad and the Korea Institute of Drug Safety and Risk Management have made outstanding contributions to public health in our Region,” said Dr Shin Young-soo, WHO Regional Director for the Western Pacific.
“The recognition they are receiving today is a strong affirmation of the significance of that work, which positively impacts the lives of many people in Malaysia, the Republic of Korea and beyond.”
Dr Ahmad was awarded the Dr LEE Jong-wook Memorial Prize for Public Health for her research on the therapeutic use of maggots (fly larvae) to clear and expedite the healing of wounds and foot ulcers caused by diabetes. The maggots remove dead tissue and secrete antimicrobial substances that fight infection and promote healing.
The number of people with diabetes is growing around the world, and diabetic foot ulcers are a serious but relatively common complication. If these wounds are not properly treated and become infected, especially with antibiotic-resistant bacteria, it could result in needing to amputate the affected limb.
In Malaysia, about six per cent of patients attending diabetic outpatient facilities develop foot ulcers, and foot complications account for 12 per cent of all diabetes hospital admissions.
Dr Ahmad’s method is effective, affordable, simple and available at any time and in any healthcare setting, including small local clinics, said the WHO.
When accepting the award, Dr Ahmad said: “Today, our therapy is being practised in health clinics in most districts in Malaysia, including in hard-to-reach areas. It is easy to access and affordable for the people, especially socially and geographically disadvantaged groups.
“We brought our research findings from the laboratory to the bedside, and now we’re preventing limb amputation in diabetic patients in health clinics. This is in line with achieving the ultimate goal of primary health care as advocated by WHO—reducing exclusion and social disparities in health and organizing health services around people’s needs and expectations.”
KIDS received the 2018 United Arab Emirates Health Foundation Prize for its outstanding contribution to health development. The Institute works to improve health in the Republic of Korea by working on prevention and recognition of drug safety-related issues, supporting evidence-based decisions on drug safety, disseminating safety information, and increasing public awareness.
The country’s pharmacovigilance system to monitor the effects of medical drugs consists of 27 regional centres. In this decentralised system, KIDS functions as the focal point, gathering and reporting data from these centres.
The data are used to provide the Ministry of Food and Drug Safety with statistics, safety information and reports of all adverse events. The reporting system further feeds into Vigibase, the global database managed by the WHO Programme for International Drug Monitoring.
“Nationwide, KIDS operates 27 regional pharmacovigilance centres, promoting the reporting of adverse drug reaction cases and incorporating the data into the WHO international pharmacovigilance programme. We take various safety measures proactively and are keen to share with WHO and other countries our experience and achievements in drug safety management,” said Dr Soo Youn Chung of KIDS.
Each year, at the World Health Assembly held in Geneva, prizes are given to recognise expertise and accomplishments in public health.
The prizes have been established either in the name of eminent health professionals and international figures or by prominent foundations committed to supporting international and global public health. Nominations are submitted by national health administrations and former prize recipients and reviewed by specialized selection panels of each of the foundations awarding a prize. The WHO Executive Board, in its January session, designates the winners based on recommendations made by the selection panels.
The Dr Lee Jong-wook Memorial Prize for Public Health is given to an individual whose work has gone far beyond the performance of duties normally expected of an official of a government or intergovernmental institution.
The United Arab Emirates Health Foundation Prize is awarded to a person, institution or nongovernmental organization that has made an outstanding contribution to health development.
Other prizes presented at the World Health Assembly this year were: the Ihsan Doğramacı Family Health Foundation Prize to Professor Vinod Kumar Paul (India); the Sasakawa Health Prize to the Fundación Pro Unidad de Cuidado Paliativo (Pro Palliative Care Unit Foundation) (Costa Rica); and His Highness Sheikh Sabah Al-Ahmad Al-Jaber Al-Sabah Prize for Research in Health Care for the Elderly and in Health Promotion to Association El Badr, Association d’aides aux malades atteints de cancer (El Badr Association, Cancer Patient Association) (Algeria).
CHRIS JOHNSON
More Medicare funding goes to wealthy kids: why, and what can we do about it?
When Medicare was in early development, the goal was to provide affordable, basic health care to all Australians. But a new study has found Medicare spending is higher for children from high socioeconomic backgrounds than their poorer counterparts.
Previous studies looking at the distribution of funding of Medicare have focused on adults. They show poorer adults are more likely to consult GPs and richer adults more likely to consult specialists.
The overall funding provided by the government favours those with low income once you control for health-care needs.
For our new study, we used the Longitudinal Study of Australian Children, a large study assessing over 10,000 Australian children over time, and linked this to the children’s Medicare data.
From this, we assessed the amount of Medicare spending on children according to five family income groups, from poorest to richest. We made adjustments to the analysis to make sure we were comparing children with equal health needs.
The results of our study show Medicare is fair for government spending on GP consultations for children, but it’s not fair for spending on specialists and testing. Overall, Medicare spending was also not evenly distributed, particularly in the first year of life.
The blue line on the graph indicates equal or fair Medicare spending, with a curve below the blue meaning more is spent on richer children.
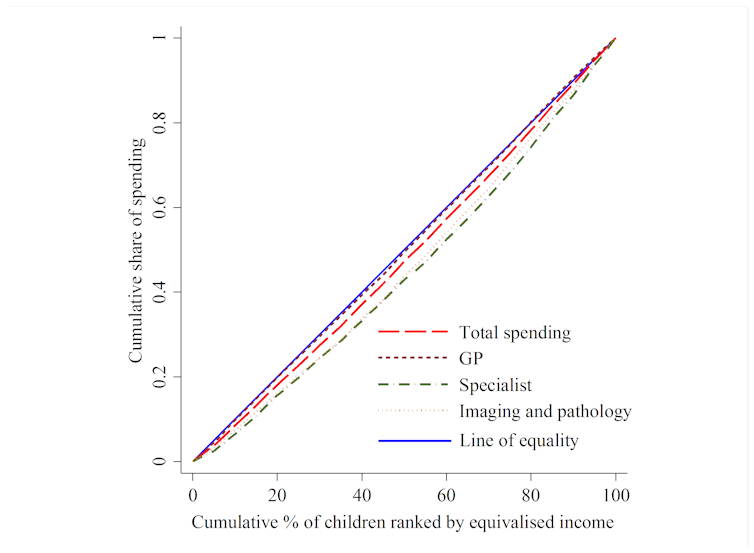
Children from higher income households gained a greater share of Medicare resources over the first 1,000 days of their lives. For children aged zero to one year, the richest 20% used 30% of specialist resources, and the poorest 20% of children used only 12%. As the children grew older, the payments became more even.
This is a worrying finding, as we know the first 1,000 days of a child’s life are critical for future health, education and well-being. Children need more health services early in life, and a healthy early childhood is increasingly recognised as protecting against chronic disease in older life. For example, low birth weight is related to increasing rates of heart disease, diabetes and bone disease in adult life.
Possible explanations
There are many efforts in Australia to ensure all children receive fair health care such as vaccinations, child health nurse visits, bulk billed GP visits and additional school services.
Part of the problem could be the patient payment that is often required when seeing a specialist. A recent study found an average co-payment of A$127 to see a paediatrician in Australia, with some costing much more.
This may be a barrier to poorer families using specialists for their children’s care. According to the Australian Bureau of Statistics, around 8% of people in Australia who need health care report delaying or not seeking care because of cost.
Another explanation could be getting specialist health care to children in rural areas, away from large children’s hospitals.
What can be done?
One solution could be to have salaried paediatricians whose services are low or no-cost available in the community, including rural areas. Preferential visits would then be given to lower income children and those with greater health needs.
![]() Seeking solutions to these problems, particularly for poorer children and rural children in the early years of life, is critical to the health of our nation. Work is still required to achieve the vision that Medicare be simple, fair and affordable for all Australians.
Seeking solutions to these problems, particularly for poorer children and rural children in the early years of life, is critical to the health of our nation. Work is still required to achieve the vision that Medicare be simple, fair and affordable for all Australians.
Kim Dalziel, Associate Professor Health Economics, University of Melbourne; Harriet Hiscock, Principal Fellow, Department of Paediatrics, The University of Melbourne, Murdoch Childrens Research Institute; Li Huang, Health Economist, University of Melbourne, and Philip Clarke, Professor of Health Economics, University of Melbourne
This article was originally published on The Conversation. Read the original article.
What the new AMA President wants to do
Melbourne GP and former AMA vice president Dr Tony Bartone was elected to the presidency of the AMA at the conclusion of the Association’s conference on Sunday. He beat two other candidates, Professor Brad Frankum, president of the AMA’s NSW branch, and Brisbane obstetrician Dr Gino Pecoraro.
Does the changing of the guard signify any change of emphasis or policy at the head of the AMA? In his acceptance speech at the AMA conference and in subsequent media interviews, Dr Bartone has urged action and says “the time for rhetoric is over”. Here are some of his key priorities in the coming two years:
- Renewed focus on general practice
Electing a GP to the presidency of the AMA sends a strong message to the government about the importance of primary care, Dr Bartone says. A decade of cuts has “systematically starved” general practice of funding and put pressure on the viability of practices around the country. The new AMA president wants “significant, targeted investment in general practice, rewarding patient-centred care”. The 55-cent rebate increase due in July after years of rebate freeze is “insulting”, he says.
He says that with the right support, GPs can help governments deliver “more health care, more efficiently, more timely, and to more Australians”. That support means rewarding work that is not just face-to-face consultations, but also efforts to prepare, structure and curate detailed health records that will become the backbone of My Health Record.
- Equitable access to healthcare
Dr Bartone says he wants significant investment to address inequitable access to services. That includes better funding of public hospitals, access to mental health care, quality aged care service provision, and access to health care services in remote and rural areas. He says we need to “change the paradigm of the way we support, fund and maintain a high-quality health system”.
- Training workforce pipeline
There are “enormous bottlenecks” in the training pipeline, which “not robust and almost broken”. This translates into a need for a national workforce strategy with quality flexible training solutions, Dr Bartone says.
- Private health
Dr Bartone’s predecessor, Michael Gannon, lobbied for more transparency and value in private health insurance. The new AMA president says he will continue to lobby for reform but he adds that private health insurance is an essential piece of the health puzzle, noting that 53% of elective surgery occurs in private hospitals. If that were to collapse, it would place an intolerable burden on public hospitals, he says.
Interestingly, he has hinted that private insurers may have a role to play in funding GP consultations, although he adds that it is “not a priority”.
- Doctors’ health
Dr Bartone says doctors’ health is an area that he is particularly passionate about. He wants an added focus on supporting colleagues who are experiencing mental health and well-being issues. He says he will work with the government and stakeholders to resolve the impasse over mandatory reporting and to ensure bullying, harassment and discrimination are a thing of the past.
- Euthanasia
While Michael Gannon was keenly opposed to Victoria’s voluntary assisted dying legislation, the new AMA president may be a little less invested in this area. He says he agrees with the AMA’s most recent position statement, which acknowledges “divergent views” among doctors concerning euthanasia and states that laws governing its practice are “ultimately a matter for society and government”.
- Asylum seekers
It seems unlikely that Dr Bartone will be returning to the asylum seeker advocacy of Michael Gannon’s predecessor, Brian Owler. When prompted by a Sky News reporter on the welfare concerns of refugees on Manus Island and Nauru, Dr Bartone had little to say other than that there are international conventions and that treatment of refugees should be “no less than the minimum that’s required”. He did not mention the asylum seeker issue in his acceptance speech.
[Comment] Offline: “The world has been warned”
What is the extent of the obligation health professionals have to the society in which they live? Beyond immediate patient care, a health worker will be an advocate for a properly financed and functioning health system. But what about the broader political context of health? To support publicly provided health services, governments must generate revenue. Adequate financing for health demands economic growth to create the fiscal space for investment. A health professional might reasonably have an interest in policies that ensure sustainable economic growth—for without that growth, health services will fall into disrepair and the quality of care will inexorably decline.
[Department of Error] Department of Error
Bertram MY, Sweeny K, Lauer JA, et al. Investing in non-communicable diseases: an estimation of the return on investment for prevention and treatment services. Lancet 2018; 391: 2071–78—In this Series paper (published online first on April 4, 2018), a copyright line has been added. This correction has been made to the online version as of April 5, 2018, and the printed Series paper is correct.
AMA President opens his last conference
Dr Michael Gannon opened the AMA National Conference 2018 by figuratively saying goodbye.
In his last opening address as AMA President, which was at times emotional, Dr Gannon detailed a long list of achievements secured by the AMA during his two-year tenure.
And he poured praise on the organisation he said he enjoyed leading since 2016.
“I must say that it has been a huge honour and privilege to serve the AMA and the medical profession as Federal President,” Dr Gannon said.
“It is demanding, challenging, rewarding, and life-changing. The issues, the experiences, the depth and breadth of policy and ideas, and the interface with our political leaders and the Parliament are unique to this job.
“The responsibility is immense. The payback is the knowledge that you can achieve great things for the AMA members, the whole medical profession and, most importantly, the community, and the patients in our care.”
His address focused largely on the ground covered since the AMA met for national conference in 2017.
Describing it as a “very busy and very successful year for the Federal AMA,” Dr Gannon said time had passed very quickly in the job but much had been accomplished.
“Throughout the last 12 months, your elected representatives and the hardworking staff in the Secretariat in Canberra have delivered significant achievements in policy, advocacy, political influence, professional standards, doctors’ health, media profile, and public relations,” he said.
“We all worked tirelessly to ensure that health policy and bureaucratic processes were shaped to provide the best possible professional working environments for Australian doctors and the highest quality care for our patients.
“The unique role of the AMA in health advocacy is that we are looked to for commentary on the breadth and depth of health policy, social policy, and the health system.”
Dr Gannon said strong and robust advocacy led to a number of policy outcomes at the federal political level.
He said many organisations get nothing for their efforts, but the AMA never gives up.
“To be successful in Canberra, you have to learn to take the knocks along with the wins, then go back again and again for a better outcome,” he said.
“It is breathtakingly naïve to think it works otherwise. And that is what we have done, and keep doing.”
In 2017, the AMA launched its regular Safe Hours Audit Report, which gave added focus to the emerging issue of doctors’ health.
To enhance this focus on doctors’ health, AMA coordination of Doctors’ Health Services continues all around the country, with funding support from the Medical Board of Australia.
“We maintained a strong focus on medical workforce and training places, which resulted in the National Medical Training Advisory Network significantly increasing its workforce modelling work,” Dr Gannon told the conference.
“We secured a number of concessions in the proposed redesign of the Practice Incentive Program, as well as a delay in the introduction of changes.
“The AMA lobbied at the highest level for a more durable solution to concerns over Pathology collection centre rents. We focused on effective compliance, and achieving a fair balance between the interests of GP members and Pathologist members.
“We led the reforms to after-hours GP services provided through Medical Deputising Services to ensure that these services are better targeted, and there is stronger communication between them and a patient’s usual GP.
“We successfully lobbied the ACCC to renew the AMA’s existing authorisation that permits GPs to engage in intra-practice price setting. This potentially saves GPs thousands of dollars every year in legal and other compliance costs.
“We ensured a proportionate response from the Government in response to concerns over the security of Medicare card numbers. This avoided more draconian proposals that would have added to the compliance burden on practices, and added a barrier to care for patients.
“We fundamentally altered the direction of the Medical Indemnity Insurance Review.”
The AMA campaigned on the issue of doctors’ health and the need for COAG to change mandatory reporting laws, promoting the WA model.
It led a nationally coordinated campaign with the State AMAs and other peak bodies to uphold the TGA’s decision to up-schedule Codeine.
It campaigned against an inadequate, poorly conceived, and ideological National Maternity Services Framework, which has now been scrapped.
The 2018 AMA Public Hospital Report Card put the political, media, and public focus on the stresses and pressures on public hospitals and all who work in them. The current funding model, based entirely around payments for activity, discourages innovation and is inadequate in addressing the demands placed by an ageing population.
“We prosecuted the case for vastly improved Private Health Insurance products through membership of the Private Health Ministerial Advisory Committee, my annual National Press Club Address, an appearance before a Senate Select Committee, and regular and ongoing media and advocacy,” Dr Gannon said.
“This work was complemented by the launch of the AMA Private Health Insurance Report Card.
“We successfully lobbied for a fundamental change in the direction of the Anaesthesia Clinical Committee of the MBS Review. The Australian Society of Anaesthetists were grateful for our assistance and leadership. Many other Colleges, Associations and Societies have worked out that partnership with, rather than competing with, the AMA is the smartest way to get results.
“We launched a new AMA Fees List with all the associated benefits of mobility and regular updates.
“We saw a number of our Aged Care policy recommendations included in a number of Government reviews.
“We lobbied against what could easily have been an ill-thought-out UK-style Revalidation proposal. Our work resulted in a vastly improved Professional Performance Framework based around enhanced Continuing Professional Development.”
Dr Gannon said the AMA had provided strong leadership right across the busy public health landscape over the past year.
The AMA Indigenous Health Report Card focused on ear health, and specifically chronic otitis media.
The Federal Council endorsed the Uluru Statement from the Heart, acknowledging that Recognition is another key social determinant of health for Aboriginal and Torres Strait Islander Australians.
A product of a policy session at last year’s AMA National Conference was the subsequent updating of the AMA Position Statement on Obesity,
“I think that it is inevitable that we will eventually see a tax on sugar-sweetened beverages similar to those recently introduced in Britain and Ireland,” Dr Gannon said.
“In fact it is so simple, so easy, and so obvious, I worry that it will be seen by a future Government as a ‘silver bullet’ to what is a much more complex health and social policy issue.”
Position Statements on an Australian Centre for Disease Control; Female Genital Mutilation; Infant Feeding and Maternal Health; Harmful Substance Use, Dependence, and Behavioural Addiction; and Firearms were also highlighted.
“We conducted ongoing and prominent advocacy for the health and wellbeing of Asylum Seekers and Refugees,” he said.
“We promoted the benefits of immunisation to individuals and the broader community. Our advocacy has contributed to an increase in vaccination rates.
“We provided strong advocacy on climate change and health, among a broader suite of commentary on environmental issues.
“We consistently advocated for better women’s health services. And released a first ever statement on Men’s Health.”
New Position Statements were also released on Mental Health, Road Safety, Nutrition, Organ Donation and Transplantation, Blood Borne Viruses, and Rural Workforce.
“We promoted our carefully constructed position statement on Euthanasia and Physician Assisted Suicide during consideration of legislation in Tasmania, Victoria, New South Wales and WA,” Dr Gannon said.
“That advocacy was not universally popular. Our Position Statement acknowledges the diversity of opinion within the profession…
“We led the medical community by being the first to release a Position Statement on Marriage Equality, and advocated for the legislative change that eventuated in late 2017.”
In July 2017, AMA advocacy was publicly recognised when the Governance Institute rated the AMA as the most ethical and the most successful lobby group in Australia.
Dr Gannon added that the highlight of the 2017 international calendar for him was the annual General Assembly of the World Medical Association.
“Outcomes from that meeting included high level discussions on end-of-life care, climate change and environmental health, numerous other global social and ethical issues, and seeing the inclusion of doctors’ health as a core issue in both medical ethics and professionalism,” he said.
“I get goosebumps when I read aloud the Declaration of Geneva. It is a source of immense personal pride that I was intimately involved with its latest editorial revision, only the fifth since 1948.
“But our focus remained at home, and your AMA was very active in promoting our Mission: Leading Australia’s Doctors – Promoting Australia’s Health.
“We had great successes. We earned and maintained the respect of our politicians, the bureaucracy, and the health sector.
“We won the support of the public as we have fought for a better health system for all Australians.”
Dr Gannon thanked his family, staff, the AMA Secretariat, Board and Federal Council.
CHRIS JOHNSON

 more_vert
more_vert