The launch of Australia’s National Lung Cancer Screening Program (NLCSP) is a step forward in preventive healthcare — but screening thousands of high-risk Australians with low-dose CT scans will inevitably uncover a far greater number of people with undiagnosed chronic respiratory disease, particularly chronic obstructive pulmonary disease (COPD).
Lung cancer is the biggest cause of cancer deaths and continues to have a relatively poor prognosis. Timely detection offers more people the opportunity to access curative interventions such as surgery. Surveillance and early detection programs will drive clinicians to deliver timely diagnostics, stratification, and treatments.
July 2025 was a landmark moment for Australian healthcare with the launch of a NLCSP. For the first time, thousands of high-risk Australians aged 50 to 70 years with a significant smoking history will receive low-dose CT scan of their chest. The aim is to catch serious respiratory disease early and save lives.
But this isn’t (just) about lung cancer.
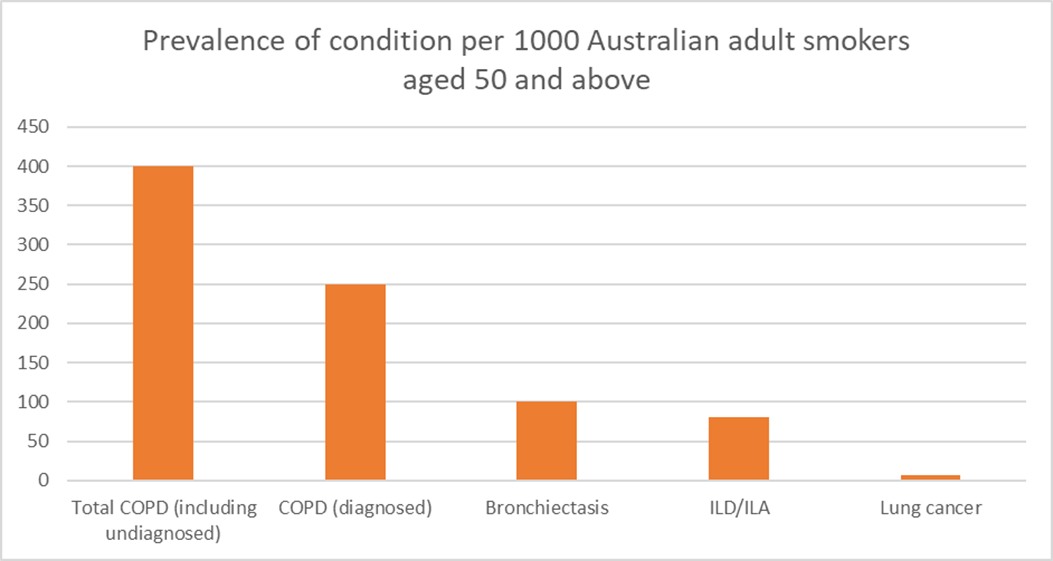
Let’s take a step back and consider what screening is likely to find. Considering the prevalences of relevant conditions gives an idea of the pre-test probability of finding various lung pathologies. Figure 1 presents the prevalence of respiratory conditions in the population that will be targeted with this NLCSP. Notably, lung cancer is relatively rare when compared with other chronic respiratory conditions, especially COPD.
Chronic obstructive pulmonary disease: a major and underdiagnosed burden
In Australia, COPD is the fifth leading cause of death, and its burden is staggering. Every 10 minutes, someone in Australia is hospitalised due to COPD. According to the Australian Institute for Health and Welfare (AIHW), these hospitalisations are the most preventable of any major condition. Yet this is just the tip of the iceberg. Earlier work suggests than this program will find changes consistent with COPD, that is of least moderate severity, in as many as 1 on 5 people who are screened. Alarmingly, up to half of Australians living with COPD are unaware they have this condition, and underdiagnosis of the highest in regional, rural, and remote communities. Timely detection of COPD offers the opportunity for evidence-based interventions that improve these outcomes (see Table 1). This is especially important for populations with worse than average health, such as those in lower socio-economic groups and indigenous populations. However, significant opportunities exist to improve outcomes across the spectrum of COPD.
| Core COPD interventions | Symptom improvement | Reduced unscheduled healthcare use | Mortality reduction |
| Smoking cessation | Yes | Yes | Yes |
| Pulmonary rehabilitation | Yes | Yes | Yes |
| Guideline concordant inhaler use | Yes | Yes | No |
| Vaccination | Yes | Yes | Yes |
The NLCSP is expected to ‘find’ thousands of Australians with CT changes consistent with COPD. Confirming these diagnoses, stratifying risk, and applying evidence-based interventions will require significant effort. This comes at a time when the traditional specialist medical model for outpatient clinics is already overwhelmed, with many patients experiencing complications and adverse outcomes while waiting months for review.
Those managed solely in primary care often receive suboptimal care, with limited access to diagnostic spirometry, guideline-directed inhaler therapy, or pulmonary rehabilitation.
Gaps in Current Practice
National data from the Australian Commission on Safety and Quality in Health Care show that between 2015–16 and 2022–23, rates of COPD spirometry assessment decreased by 31%, while prescriptions for triple-therapy inhalers increased by 130% — highlighting a worrying disconnect between diagnosis and treatment.
To take advantage of the opportunity presented by the NLCSP, healthcare systems cannot rely on traditional models that are already stretched thin. Innovation is essential to improve accessibility and efficiency. This can be achieved by leveraging expertise beyond the medical profession, particularly where non-pharmacological interventions — smoking cessation, pulmonary rehabilitation, weight management, inhaler training, and vaccination — are best delivered by specialist allied health professionals and nurses under appropriate clinical governance.
The Role of Multidisciplinary Pathways
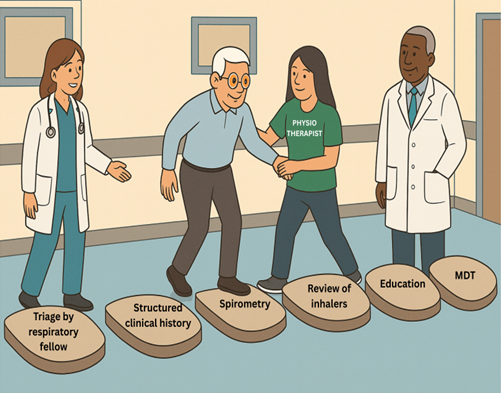
In response to the anticipated increase in COPD detection, there will need to be an increase in capacity in outpatient services. Such services are likely to be led by nurses or allied health professionals with the collaboration of specialist physicians. Figure 2 gives an example of a streamlined multidisciplinary pathway currently in use. Such services will make most efficient use of clinical time and allow of discussion of complicated cases in multidisciplinary team meetings.
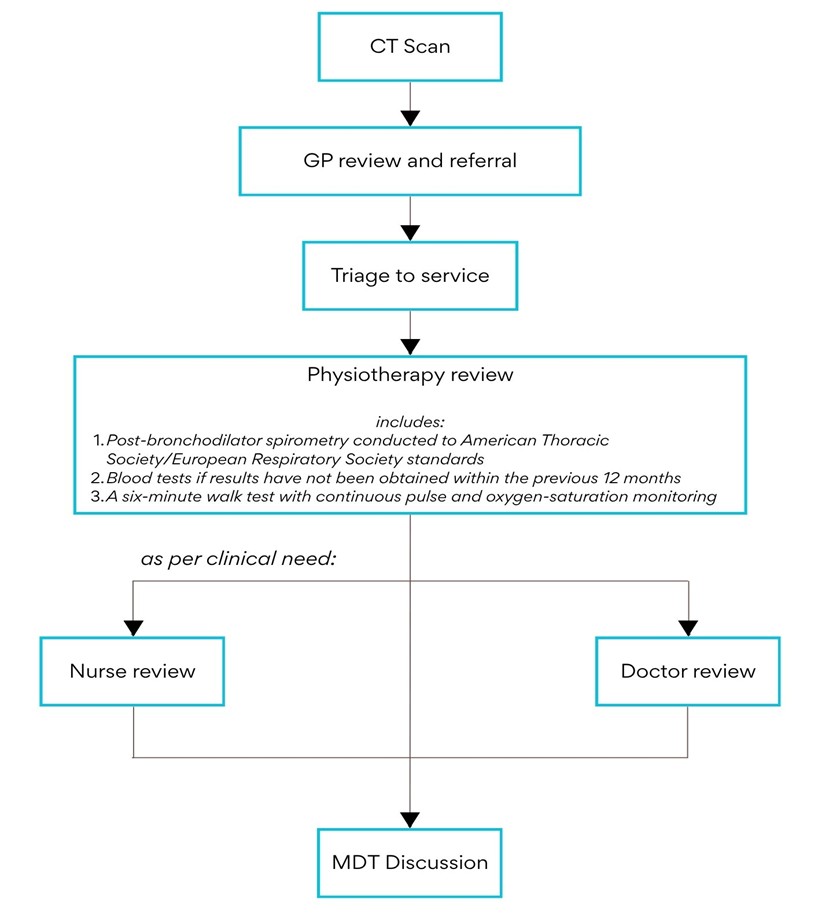
Following assessment, the physiotherapist presents each case at a multidisciplinary team meeting within a fortnight. The team then decides the next steps in the care pathway — such as discharge, further allied-health follow-up, or referral to a respiratory physician for ongoing specialist review.
This model of care delivers high-quality, patient-centred management that bridges diagnostic and therapeutic gaps and reduces pressure on traditional outpatient clinics. By enabling allied health professionals to play a central role in early COPD management — with medical oversight where needed — such clinics exemplify how innovation can transform efficiency, maintain safety, and improve outcomes within Australia’s respiratory care landscape.
Conclusion
COPD is a serious, costly and relatively underdiagnosed condition. Crucially it is also treatable, with major benefits when interventions are made early. However, care is often suboptimal, and usually when substantial harm has been accrued. The NLCSP is a very welcome addition the healthcare landscape, and brings with it the prospect of improving COPD management and outcomes. However, newer multidisciplinary ways of working will be required to get the most from this opportunity.
Dr Sanjay Ramakrishnan is an airways specialist respiratory physician at Sir Charles Gairdner Hospital. He also leads the Perth Exacerbation Research group at the Institute for Respiratory Health, UWA.
Clinical Professor John Blakey is a respiratory physician with clinical expertise in obstructive airways diseases, and a record of quality improvement interventions.
Dr Christopher Kosky is a respiratory and sleep physician with an interest in COPD, particularly advanced therapies for severe disease.
Tamara Thornton is a clinical respiratory physiotherapist with expertise and specialist interest in adult chronic lung disease.
Kylie Hill is a Professor of physiotherapy with experience in management of chronic lung disease, especially pulmonary rehabilitation.
Zoe Castillo is a research administration officer at the Institute for Respiratory Health, UWA.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
In the model under Physiotherapy review, it appears they are ordering pathology ( “blood tests if results have not been obtained in last 12 months”- how is this in a physio scope of practice? Who’s provider number would be used for this pathology and exactly what tests need to be done
Perfection is the enemy of good care. Fine to say a single patient should get multidisciplinary care, especially when your practice is a large urban teaching hospital, but its not going to happen. I work in an area of Sydney where specialist appointments have a 6 months waiting period and the local populace generally can’t afford the exorbitant fees. Chronic disease needs to be GP-led care with specialist referrals for a small subset of the unwell population.
underdiagnosis of the highest in regional, rural, and remote communities Don’t worry about that. They won’t get screened anyway – or at least not as frequently as urban dwellers.
Retired regional public health medical officer