Close relatives of people diagnosed with coeliac disease should be screened for the disease themselves, according to an Australia-first study.
The study, published in the Medical Journal of Australia, has found significant prevalence of undiagnosed coeliac disease among first degree relatives of people already diagnosed.
The study findings support existing overseas recommendations for screening of first degree relatives for coeliac disease.
Coeliac disease is an autoimmune disorder where the ingestion of gluten in genetically susceptible individuals causes gastrointestinal symptoms.
Delayed diagnosis of coeliac disease can lead to serious health complications such as osteoporosis, infertility, and small bowel cancer.
“We undertook this research to look at the value of finding cases of coeliac disease in people at high risk of coeliac disease in Australia,” lead author Dr James Daveson told InSight+.
Dr Daveson is a gastroenterologist with a subspecialty clinical and research interest in coeliac disease and inflammatory bowel disease.
“First degree relatives (siblings, parents and children of people with diagnosed coeliac disease) are the highest-risk group for the development of coeliac disease.”
“We know in Australia we are not good at diagnosing coeliac disease. Although coeliac disease affects 1.4% of Australians, only one in three people with the disease are diagnosed.”

How the study was conducted
Researchers at the Wesley Research Institute in Brisbane set out to determine the prevalence of undiagnosed coeliac disease among first degree relatives of people who had been diagnosed.
A total of 202 first degree relatives (children, siblings or parents) of 134 people with coeliac disease were invited to undergo testing for coeliac disease.
Testing included HLA-DQ2/8/7 polymerase chain reaction genotyping for coeliac disease risk alleles and, where possible, small bowel biopsy.
The study found seven of 62 child first degree relatives of people with coeliac disease had biopsy-confirmed disease, yielding an estimated prevalence of 11%.
For those with coeliac disease susceptibility haplotypes, the prevalence was 14%.
The need for family screening
Dr Daveson told InSight+ he was surprised by the findings.
“The rate of undiagnosed high risk children in Australia with coeliac disease based on these findings is 14%, which is ten times the national prevalence of the disease,” Dr Daveson said.
“Whilst I expected there to be many undiagnosed children in this study (given we know that in Australia we underdiagnose people with this condition), I was surprised by just how high that number was.”
Dr Daveson hopes the study will emphasise to health practitioners the importance of family screening for coeliac disease.
“Defining such a high rate of undiagnosed … high risk children with coeliac disease is important for Australian health practitioners,” Dr Daveson said.
“The most important outcome of this study will be if it highlights the need for first degree relatives of people with coeliac disease to be screened for coeliac disease themselves.”
Read the research in the Medical Journal of Australia
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert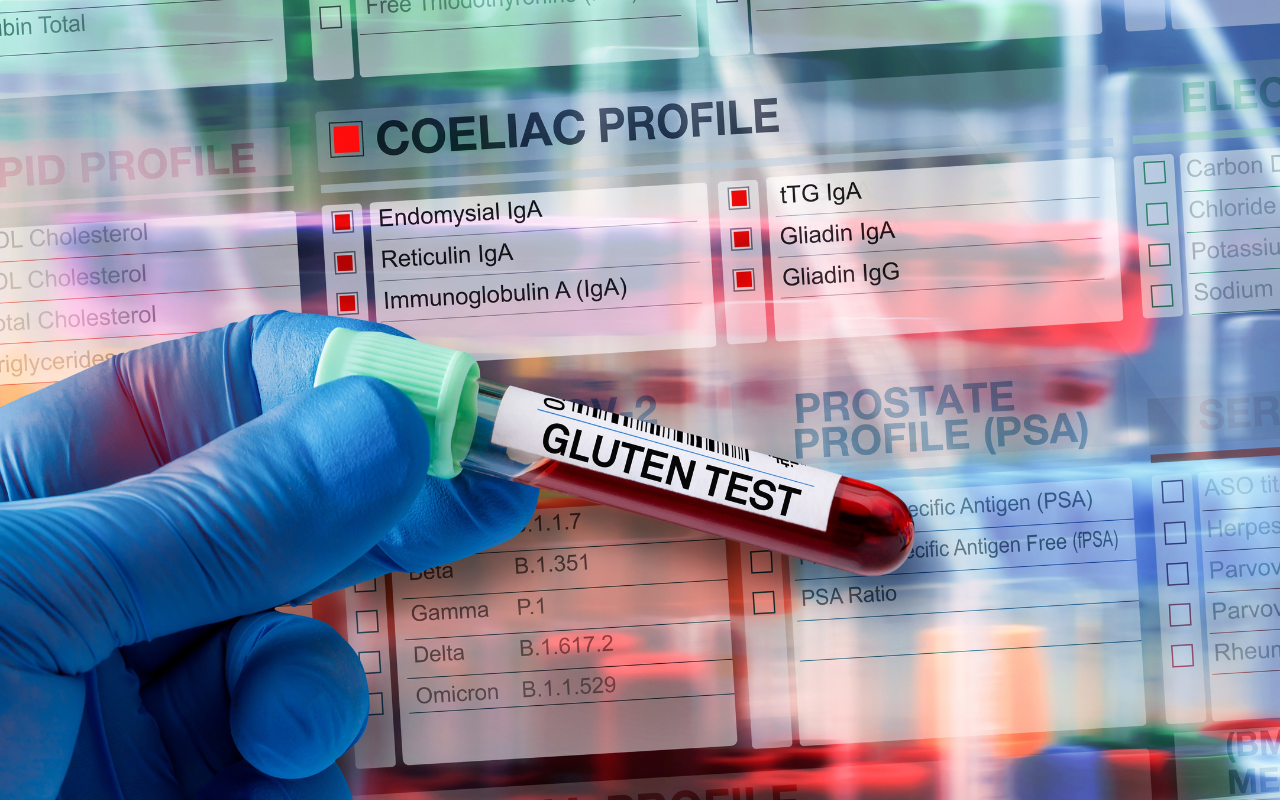
I applaud the above comment. We cant scope every person who has fatigue otherwise I would be referring 4 women a day. Let us know when there is a cheaper more convenient and accurate test.
After nearly 40 years in general practice , mostly rural and isolated rural, I think of coeliac disease all the time in anyone with fatigue , chronic gut issues or family history . Progressively over these years Medicare Australia , governments and hospitals put you on notice if you try to explore the diagnosis of coeliac disease . Anti gliaden antibody is a limited test at best, that is very useful if it is positive. The antibody testing can be deemed screening and is NOT SUPPORTED BY A MEDICARE REBATE . If medicare decides you are screening, a gp can be forced to pay back all the testing for the previous 2 years . Genetic testing for coeliac predisposition is seriously frowned upon by medicare . I personally know of a couple of gps’ who were audited and subject to very distressing peer review as a result of working in their subspecialty field in general practice . Waiting for referrals for gastroscopy and biopsy to be acted on can take many years now for public patients. Waiting for a gastroenterologist referral ( to be acted on , public or private ) can be arduous for both the patient and gp these days ..Some years ago as a rural gp I could at least talk to a specialist about options while waiting for a definitive diagnosis or appointment to become available. Since then I am truly shocked if I get past any reception. Registrars at big hospitals used to be helpful. Now most of them are warned against giving any advice! Faced with an unwell patient , with the potential consequences of untreated coeliac, the patient often feels alot better gluten free . Gluten free diets without proof of coeliac are then frowned upon ( both the patient and the doctor ) !! Most patients choose to stay gluten free and when it finally comes time for their small bowel biopsy …they do not want to become very sick with a decent gluten challenge and most do not want to take the risk ( all be it small) of upper gi perforation/bleeding to have the proof that they need to be back on a gluten free diet . The testing for the consequences of coeliac disease ( particularly the nutritional deficiencys like b12, iron, and VITAMIN D deficiencys ), and osteoporosis are frowned upon by peers and medicare. It is no longer unusual to be given a really hard time from both peers and m/c rebate regulators regarding implementation of best practice . Even the pathology guidelines regarding vitamin D deficiency suggest deficiency at less than 50 . All the evidence says a minimum of 75 for vitamin D to be considered adequate to perform its many functions.
Perhaps, instead of trying to repeatedly infer that doctors need better education as to the importance of early diagnosis of coeliac, could we all accept that doctors are acutely aware of the clinical importance of early diagnosis ( not just coeliac disease ) and put our efforts into making it possible for both the patient and the doctors to achieve best practice outcomes in the application of their clinical knowledge ??
In my view and experience in Australia , as our knowledge increases the need and demand for access to the application of this clinical knowledge increases . The response from governments ( state and federal ) and regulatory bodies is to put up ever increasing barriers to accessing the best outcomes for patients . Most of general practice is private sector. My simplistic observation is that increaseing demand for the doctors services /HEALTH PRODUCT is met with essentially delaying or blocking access to supply . I am not sure that reigning in demand for any popular product in business has ever worked . “The good health product” surely could do with a full throttle attempt at meeting demand by increasing supply of good health product services ???